lecture twenty-one – reproductive system
advertisement

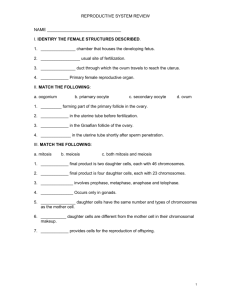
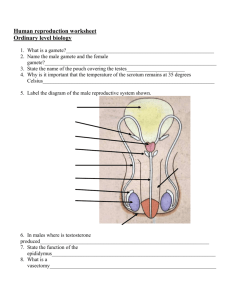
HUMAN ANATOMY LECTURE TWENTY-ONE REPRODUCTIVE SYSTEM FUNCTIONS MALE REPRODUCTIVE FUNCTIONS • Production of sperm cells • Sustaining and transfer of sperm to female - nutrients, environment to mature, and secretions of semen • Production of male sex hormones - control male development and functioning of male reproductive system FEMALE REPRODUCTIVE FUNCTIONS • • • • Production of female sex cells Reception of sperm cells from the male and transportation to site of fertilization Nurturing development of and providing nourishment for fetus Production of female sex hormones - control development of female reproductive system and female body, reproductive behaviour MALE ANATOMY MALE PERINEUM SCROTUM • 2 chambered sac divided into right and left halves separated by a C.T. septum (raphe) • Beneath epidermus is layer of loose C.T. and smooth muscle (dartos) • Dartos and cremasteric muscles help regulate temperature of the testes by raising them into the abdomen TESTIS • Located outside the body to keep sperm at lower than body temperature for development • Serve as both exocrine - produce sperm and endocrine - release testosterone • Tunica Vaginalis - serous membrane lining scrotal cavity and reduces friction between scrotal and testicular surfaces • Tunica Albuginea - thick white C.T. - divides testes into lobules - within lobules are seminiferous tubules and interstitial (Leydig) cells (secrete testosterone) • Tubes carrying sperm: - seminiferous tubules (site of sperm production) - tubuli recti and rete testis (pathway to epididymis) DESCENT OF THE TESTES SPERM CELL DEVELOPMENT Spermatozoa are produced in seminiferous tubules at puberty. GnRH secretion increased leading to increased LH and FSH release. FSH promotes sperm production and also promotes interstitial cells to produce large amounts of testosterone. • Spermatogonia divide (mitosis) forming primary spermatocytes • Primary spermatocytes divide (1st division of mitosis) forming secondary spermatocytes • Secondary spermatocytes divide (2nd division of mitosis) forming spermatids • Spermatids develop an acrosome and flagellum • Sustentacular (Sertoli or nurse) cells nourish sperm cells, form a bloodtestis barrier and produce hormones - attached to sperm during development • Sperm move to epididymis to mature MALE DUCTS (not ducks) EFFERENT DUCTULES - lead out of testis, rete empty into EPIDIDYMIS - site of sperm cell maturation - long coiled tubules on surface of teste - have stereocilia in pseudostratified columnal epithelium increasing surface area to facilitate absorption of fluid from lumen of the duct - smooth muscle moves sperm through DUCTUS DEFRENS - from epididymis into abdominal cavity - associated with blood vessels, lymphatic vessels, and nerves supplying testis all form spermatic cord (surrounded by cremaster muscle and C.T. sheath) - extends into abdominal wall through inguinal canal - just before reaching prostate gland diameter increases to become ampulla of ductus deferens - smooth muscle wall that propels sperm cells by peristalsis EJACULATORY DUCT - joins ductus deferens and seminal vesicle - extends into prostate gland and joins urethra within prostate ACCESSORY GLANDS SEMINAL VESICLES - saclike glands near ampulla of ductus deferens • Empty into ejaculatory duct • Produce 60% of semen • Secretion contains: fructose, prostaglandins (stimulates muscle contractions in both male and female), fibrinogen (forms clot in vagina for protection) • Secretion are alkaline to neutralize acids of vagina • Activate flagella in previously inactive sperm cells PROSTATE GLAND - muscular gland surrounding urethra and the two ejaculatory ducts • Produces 30% of semen • Thin, milky secretion high pH containing seminalplasmin (antibiotic preventing urinary tract infection in males) BULBOURETHRAL GLANDS - at base of penis • Ducts empty into urethral lumen • Have compound tubuloalveolar mucous glands that secrete thick alkaline mucus to lubricate glans of penis and neutralize any urinary acids URETHRA • Extends from urinary bladder to distal end of penis • Passageway for urine and semen • Divided into three parts: - prostatic region which passes through the prostate - membranous region which passes through the floor of the pelvis and is surrounded by external urinary sphincter - spongy (penile) region extending the length of the penis • Parasympathetic reflex prevents urine from passing from urinary bladder while semen is exiting PENIS • Functions for urination, semen transport EXTERNAL ANATOMY • Overlying skin resembles scrotum with layer of smooth muscle under dermis continuous with the dartos muscle of scrotum • Crus and bulb = root of penis – fixed to body wall • Shaft (body) - moveable portion • Glans of penis - enlargement of corpus spongiosum • Prepuce or foreskin covers glans (circumcision - surgical removal) • External urethral orifice INTERNAL ANATOMY • Erectile tissue is a maze of vascular channels incompletely separated by elastic C.T. and smooth muscle - during rest arteriole branches are constricted and muscular partitions tense to prevent blood flow in - when nitric acid is released at synapses smooth muscles relax , arterioles dilate and blood flows in = erection • Three columns of erectile tissue: - corpora cavernosa (2) expands at base to form crura - each surrounds a central artery - corpus spongoisum (1) surrounds spongy urethra forms the bulb of penis - expands to form the glans - contains many elastic fibers and a pair of small arteries FEMALE ANATOMY • Internal organs found within the pelvis, between urinary bladder and rectum • Broad ligament attaches to both sides of the uterus and spreads out attaching fallopian tubes and ovaries OVARIES • Function to produce immature oocytes, secretion of female hormones • Outermost covering is the ovarian epithelium (visceral peritonium) • Dense fibrous C.T. layer (tunica albuginea) lies under epithelium • The ovary is divided into: - cortex is the outer, dense region containing follicles with oocytes - medulla is the inner, looser region containing blood vessels, nerves, lymphatic vessels - stroma is the C.T. that divides the ovary • Ovaries are held in the pelvic cavity by ligaments - suspensory ligament extends from ovary to body wall - ovarian ligament attaches ovary to uterus, blood vessels and nerves enter ovary through here - mesovarium is a peritoneal fold attaches ovary to posterior surface of broad ligament MATURATION OF OOCYTE • Oogenesis - production of a secondary oocyte in ovary beginning before birth • Oogonia - cells that divide by meiosis producing primary oocytes • 5 million oocytes are produced by the 4th month of pregnancy - about 2 million begin dividing but stop in prophase until puberty • Primary oocytes are surrounded by granulosa cells and called a primordial follicle (only 400 will reach final stages of development) • Primordial follicle becomes a primary follicle when oocyte and granulosa cells enlarge • Primary follicle becomes secondary follicle and enlarges to form a Graafian follicle (matures) - only one matures each month, others degenerate OVULATION AND FERTILIZATION • Ovulation - release of a secondary oocyte from the ovary - blood, follicular fluid and oocyte are all released out of ruptured follicle • Graafian follicle becomes the corpus luteum • Secondary oocyte completes meiosis after fertilization occurs • Fertilized egg is now a zygote • If no fertilization - corpus luteum becomes corpus albicans (a knot of pale scar tissue) • If fertilization - corpus luteum persists producing progesterone until placenta forms UTERINE (FALLOPIAN) TUBES • Extend from ovary, opening directly into peritoneal cavity, to uterus • Fimbriae - thin, finger-like processes that extend from infundibulum (funnel) • Inner surfaces lined with cilia that beat toward the ampulla (middle segment of tube where fertization occurs) • Isthmus - short, narrow segment connected to uterus • Mesosalpinx - area of broad ligament associated with uterine tube • Three layers: outer serosa, middle smooth muscle layer, inner mucosa - mucosa is simple ciliated columnar epithelium with longitudinal folds - provide nutrients for oocyte or embryo - cilia move fluid and oocyte/embryo toward uterus UTERUS • Provides protection, nutrition, waste removal for developing embryo • Pear-shaped organ bent anteriorly near the base covering the anterior and superior surfaces of the urinary bladder • Composed of: fundus (superior region), body (main region), and cervix (narrow, inferior area) • Three layers: perimetrium - outer serous membrane myometrium - thick, smooth muscle endometrium - mucous membrane - simple columnar epithelial cells with simple tubular glands - functional layer that is sloughed off during menstruation • Cervix - more rigid and less contractile than the rest • Cervical canal - lined with mucous glands, mucus plug near ovulation forms when consistency of secretion changes to seromucus VAGINA • Extends from uterus (cervix) to outside • Receives penis during intercourse, allows menstrual flow and childbirth • Hymen (thin mucous membrane) covers vaginal opening - several holes allows menstrual flow • Outer smooth muscle layer with many elastic fibers allow stretching during intercourse and child birth also longitudinal folds and rugae • Inner mucous membrane lining of moist stratified squamous epithelium forms protective layer • Fornix - superior domed portion attached to sides of cervix EXTERNAL GENITALIA • • • • • • • Vulva or pudendum - external area including vestibule and external genitalia Vestibule - space where vagina and urethra open Labia minora - thin, longitudinal skin folds bordering the vestibule Clitoris - small erectile structure in anterior of vestibule, has fold of skin covering called prepuce On either side of vestibule there are openings to the greater vestibular glands - maintain moistness Vaginal orifice - contains erectile tissue Labia majora - prominent rounded folds of skin on either side of labia minora, conceal contents of vulva - meet anteriorly to form elevated tissue mons pubis over the symphsis pubis - medial surfaces covered with sebaceous and sweat glands PERINEUM MENSTRUAL CYCLE At puberty • Begins with menarche (first episode of menstrual bleeding) • Begins when GnRH levels increase Menstrual Cycle • About 28 days long • Phases: - menses - proliferative or follicular phase (follicle matures) - secretory phase (maturation and secretion of uterine glands, presence of corpus luteum) • Amenorrhea - absence of menstrual cycle • Menopause - cessation of menstrual cycles