14steriod
advertisement

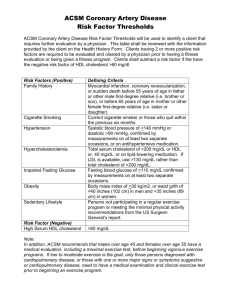
* Biosynthesis of Cholesterol, Steroids and Isoprenoids - Important lipid 1- structural lipid present in membrane. 2- precursors of steroidal hormones. - 27 C of cholesterol is derived from acetate. * The isoprene units are key intermediates in pathway from acetate to cholesterol and also they are precursors to many natural lipids Cholesterol is NOT important to be in the diet because it can be synthesized in all of the cells. Cholesterol is made of Acetyl CoA in four stages 6 Carbon 5 Carbon 30 Carbon 27 Carbon Cystolic - hydroxy - methyl glutaryl CoA synthase In the cytosol (HMG CoA synthase) Is different from HMG-CoA synthase in the mitochondria in keton body formation. The committed step HMG-CoA reductase : integral protein in endoplasmic reticulum and it is a point of regulation. Biosynthesis of Cholesterol Biosynthesis of Cholesterol * Cholesterol has several fates : - Most of cholesterol is synthesized in liver, a little amount is synthesized in the cells. - Small fraction is incorporated into the cell membrane of hepatocytes. - Most of it is exported in one of three forms. - Bile acids and salts. - Cholesterol esters formed in the liver by acyl- CoA- cholesterol acyl transferase (ACAT) - Adrenal gland and gonads use cholesterol for sex hormonal biosynthesis and vitamin D. * Degradation of cholesterol - The ring structure of cholesterol cannot be oxidized or metabolized into CO2 and H2O in humans, So intact ring is eliminated in form of : 1- Bile salt that eliminated by feces. 2- Secretion of cholesterol into bile, that also go with feces. - Some cholesterol is modified by normal flora to give Cholestanol and Caprostanol * Regulation of cholesterol synthesis 1- Feed back inhibition. - Cholesterol is a feed back inhibitor of HMG-CoA reductase decrease cholesterol synthesis. - HMG-CoA reductase activity is the rate limiting step in the biosynthesis of cholesterol and subjected to different controls. 2- Hormonal regulation of cholesterol biosynthesis. - HMG- reductase is controlled by Glucagon and Insulin. - Glucagon increase formation of inactive (phosphorylated) form of the enzyme decrease cholesterol biosynthesis. - Insulin increase formation of active (unphosphorylated) form of the enzyme increase cholesterol biosynthesis. 3- Sterol-mediated regulation of transcription. - cholesterol taken by cells from lipoproteins decrease biosynthesis of cholesterol by decrease of transcription of DNA of the HMG-CoA reductase enzyme. 4- Inhibition of drugs. Lovastatin and Mevastatin are competitive inhibitors of HMG-CoA reductase. * Regulation of cholesterol synthesis * Regulation of cholesterol synthesis * Bile acids and Bile salts - Bile consist of a watery mixture of organic and inorganic compounds. Bile can go from the liver directly to the intestine or to be stored at bilary gland. - The most common bile acid : Cholic and Chenodeoxycholic acid. - Bile acids are not fully ionized at pH = 7 because they have pKa = 6, (they are amphipathic compounds) Synthesis of bile acids - Synthesized in the liver. - Reduction of the double bond, insertion of hydroxyl groups and shortening of cholesterol. - The rate limiting step is insertion of -OH group at C7, by 7 -hydroxylase. Action of intestinal flora 1- removing of glycin and taurine 2- modification at the bile acids to produce secondary bile acids (removing OH groups) deoxycholic acid and lithocholic acid. Synthesis of bile salts - Bile acids are released from liver. They conjugated with amino acid Glycin or Taurine by amide linkage and called bile salts - glycocholic and glycochenodeoxycholic acid - taurocholic and taurochenodeoxycholic acid - The addition of glycin or taurine decrease pKa increase ionization of these compounds at pH = 7.4 because of the presence of COO- and sulfate - Bile salts are more effective detergent than that of bile acids - only bile salts, are found in the bile, Bile acids and Bile salts Biosynthesis of steroidal hormones steroidal hormones are derived from cholesterol Adrenal cortex mineralocorticoids glucocorticoids Sex hormones are synthesized in male and female Gonads * Cholesterol and other lipids are carried on plasma lipoproteins: - cholesterol, cholesterol esters and other lipids are essentially insoluble in water. To be moved from one part to another they should carried as plasma lipoprotein. Plasma lipoproteins - Macromolecular complexes of lipids and specific proteins called apolipoprotein with a various combination of phospholipids, cholesterol, cholesterol esters and TG. * Function : to keep the lipid soluble for transporting them between organs and also provide efficient mechanism for delivering their lipid contents to the tissues. * Composition of plasma lipoproteins - TG and cholesterol esters are mainly carried by lipoprotein (In the core : TG + cholesterol ester, In the surface : hydrophilic parts of cholesterol, phospholipids and hydrophilic parts of apolipoproteins. Apolipoproteins : the free form, have several functions , structural component, recognition sites, activators or coenzymes. * Size and density of lipoprotein particles different combinations of lipids and proteins produce different particles that differ in densities ranging from lowest density Chylomicrons to HDL (high density lipoprotein) can be separated by ultra centrifugation. lipoproteins Each class of lipoprotein has specific function determined by point of synthesis, lipid composition and apolipoprotein content. Apolipoproteins classified A to H. each class has subclasses * Metabolism of Chylomicrons - The largest in size and least density of lipoproteins. - Synthesized in the endoplasmic reticulum of epithelial cells that line the small intestine, then they are packaged in secretory vesicles by Golgi and exported to lymphatic system then enter the blood stream. * The “nascent chylomicron” that released by intestinal mucosal cells contain apo B-48 (unique for chylomicrons) then this nascent chylomicron is rapidly modified receiving apo E and apo C.II from circulating HDL. * Degradation of chylomicrons lipoprotein lipase : (activated by apo C.II) hydrolyses TG in these particles into free fatty acids and glycerol. *Chylomicrons lipoprotein lipase chylomicron remnants (decrease size, increase density) - apolipoprotein C is returned to HDL and the remnant is taken up by hepatocytes. - Receptors of hepatocytes recognize the remnant through apo E and apo B-48 activation of up taking by endocytosis release cholesterol. - The release of cholesterol regulate the cholesterol synthesis in the liver by decrease HMG CoA reductase and also inhibit allosterically this enzyme. * Metabolism of very low density lipoprotein (VLDL) - Excess of F.A can be converted into TG in the liver and packaged with specific apolipoprotein to form VLDL. - F.A , excess CHO 1- can be converted into TG stored in adipocyte. 2- TG packaged into VLDL (liver) * VLDL : TG, cholesterol, cholesterol esters, apo C.I, C.II, C.III, apo E. * VLDL are transported in the blood from the liver to muscle and adipose tissue. VLDL lipoprotein lipase free F.A - oxidation (myocytes) OR resynthesis of TG (adipocytes) * VLDL : produced in liver and composed mainly of TG and their function to carry lipids from liver to peripheral tissues and are degraded by lipoprotein lipase. * Fatty liver : imbalance between hepatic TG synthesis and secretion of VLDL, diseases as hepatitis, uncontrolled diabetes, chronic ethanol ingestion can cause fatty liver. * VLDL is released from the liver as nascent VLDL containing apo- 100 and apo A.I and then it will take apo C.II and apo E from circulating HDL. Metabolism of lipoproteins * Modification of circulating VLDL : TG are removed from VLDL (decrease size , increase density) - IDL : VLDL remnants - apo C.II and apo E are returned to HDL - cholesterol esters transfer from HDL to IDL by enzyme lecithin- cholesterol acyl transferase - The VLDL is converted into LDL in the plasma. * Metabolism of LDL - LDL particles have apo B-100, contain less TG, high concentration of cholesterol and cholesterol esters. - The primary function of LDL is to provide the peripheral tissue by cholesterol and this process is Receptor- mediated endocytosis. * apo B-100 is recognized by LDL- receptor activate the degradation by endocytosis. - VLDL contains apo B-100, but can’t bind to LDL receptors. (the conversion of VLDL into LDL) exposes of the receptor- binding domain of apo B-100 * Fate of cholesterol - cholesterol that enter the cell can be incorporated into the cell membrane or can be reesterified by ACAT for storage as form of cholesterol esters. * LDL also con be up taken by liver cells mediated by apo E. cholesterol esters transfer from HDL to IDL by enzyme lecithin- cholesterol acyl transferase *Receptor- mediated endocytosis Cholesterol is delivered from LDL into the peripheral cells. * LDL receptors deficiency elevation of plasma LDL increase plasma cholesterol. Type II hyperlipidemia Peripheral cell needs cholesterol. Receptor-Mediated endocytosis * Effect of endocytosed cholesterol on cell cholesterol content. Chylomicron remnant, HDL, LDL, drive cholesterol into liver cells decrease cholesterol synthesis and content in three ways * Metabolism of HDL - Synthesized in the liver and small intestine as small, protein- rich particles that contain little cholesterol and no cholesterol esters. (nascent HDL, depleted HDL) - Contain apo A.I, C.II, C.III and others and LCAT (lecithin- cholesterol acyl transferase) PCAT (phosphatidyl choline- cholesterol acyl transferase) - LCAT at the surface of nascent HDL converts the cholesterol and PL of chylomicron as VLDL remnant to cholesterol esters that forms the core of HDL and formation of mature spherical HDL particle. - Then the cholesterol rich HDL returns to the liver where the cholesterol is unloaded that can be converted into bile salts. * Depleted HDL can be pick up cholesterol stored in extra hepatic tissues and carry it to the liver in “ Reverse Cholesterol Transport ” pathway. Nascent HDL binding cholesterol rich cell from cell to the HDL goes to the liver. passive movement of cholesterol - up taking of cholesterol from cells by enzyme LCAT and storing of cholesterol ester in the core of HDL. 1-HDL as reservoir of apolipoproteins It act as circulating reservoir of apo C.II that can be transferred to VLDL and chylomicron. And also takes back the apoprotiens before VLDL remnants and chylomicron remnants are taken by the liver. 2-Up taking of free cholesterol 3-Esterification of free cholesterol into CE by LCAT. * CE (cholesterol esters) that stored in HDL can be transferred into VLDL and exchanged by TG or PE by CE transfer protein. VLDL LDL CE is utilized by cells. * Fate of HDL - HDL is taken by liver by receptor- mediated endocytosis. And CE are degraded and cholesterol can be repackaged in lipoprotein, converted into bile acids or secreted into bile. * Role of lipoproteins in heart disease - high levels of cholesterol increase risk of atherosclerosis linked to high level of LDL, decrease HDL. The End * Bile acids and Bile salts - Bile consist of a watery mixture of organic and inorganic compounds. Bile can go from the liver directly to the intestine or to be stored at bilary gland. - The most common bile acid : Cholic and Chenodeoxycholic acid. - Bile acids are not fully ionized at pH = 7 because they have pKa = 6, (they are amphipathic compounds) * Synthesis of bile acids - Synthesized in the liver. - Reduction of the double bond, insertion of hydroxyl groups and shortening of cholesterol. - The rate limiting step is insertion of -OH group at C7, by 7 hydroxylase. * Synthesis of bile salts - Bile acids are released from liver. They conjugated with amino acid Glycin or Taurine by amide linkage and called bile salts - glycocholic and glycochenodeoxycholic acid - taurocholic and taurochenodeoxycholic acid - The addition of glycin or taurine decrease pKa increase ionization of these compounds at pH = 7.4 because of the presence of COO- and sulfate - Bile salts are more effective detergent than that of bile acids - only bile salts, are found in the bile, * Action of intestinal flora 1- removing of glycin and taurine 2- modification at the bile acids to produce secondary bile acids (removing OH groups) deoxycholic acid and lithocholic acid.