Antihyperlipidemic
advertisement
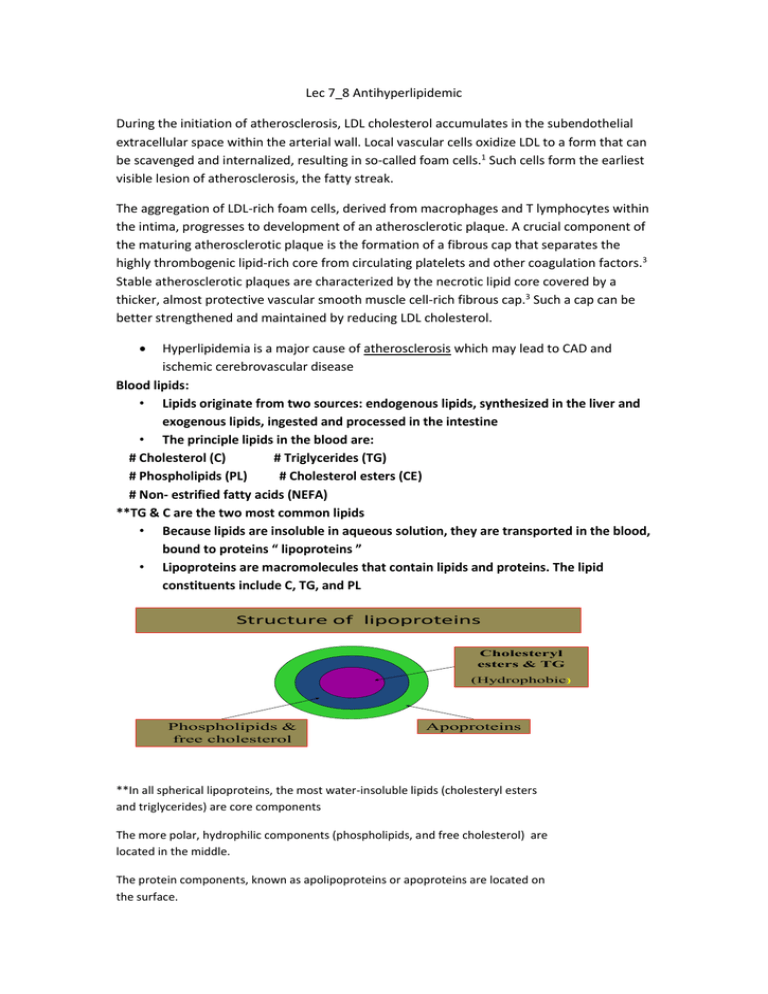
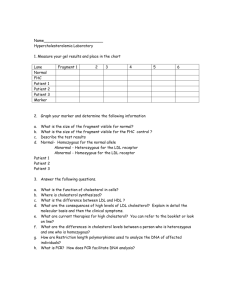
Lec 7_8 Antihyperlipidemic During the initiation of atherosclerosis, LDL cholesterol accumulates in the subendothelial extracellular space within the arterial wall. Local vascular cells oxidize LDL to a form that can be scavenged and internalized, resulting in so-called foam cells.1 Such cells form the earliest visible lesion of atherosclerosis, the fatty streak. The aggregation of LDL-rich foam cells, derived from macrophages and T lymphocytes within the intima, progresses to development of an atherosclerotic plaque. A crucial component of the maturing atherosclerotic plaque is the formation of a fibrous cap that separates the highly thrombogenic lipid-rich core from circulating platelets and other coagulation factors.3 Stable atherosclerotic plaques are characterized by the necrotic lipid core covered by a thicker, almost protective vascular smooth muscle cell-rich fibrous cap.3 Such a cap can be better strengthened and maintained by reducing LDL cholesterol. Hyperlipidemia is a major cause of atherosclerosis which may lead to CAD and ischemic cerebrovascular disease Blood lipids: • Lipids originate from two sources: endogenous lipids, synthesized in the liver and exogenous lipids, ingested and processed in the intestine • The principle lipids in the blood are: # Cholesterol (C) # Triglycerides (TG) # Phospholipids (PL) # Cholesterol esters (CE) # Non- estrified fatty acids (NEFA) **TG & C are the two most common lipids • Because lipids are insoluble in aqueous solution, they are transported in the blood, bound to proteins “ lipoproteins ” • Lipoproteins are macromolecules that contain lipids and proteins. The lipid constituents include C, TG, and PL Structure of lipoproteins Cholesteryl esters & TG (Hydrophobic) Phospholipids & free cholesterol Apoproteins **In all spherical lipoproteins, the most water-insoluble lipids (cholesteryl esters and triglycerides) are core components The more polar, hydrophilic components (phospholipids, and free cholesterol) are located in the middle. The protein components, known as apolipoproteins or apoproteins are located on the surface. Atherosclerosis Normal Endothelium Development of Atherosclerotic Plaques Normal Fatty streak Lipid-rich plaque Foam cells Fibrous cap Thrombus Lipid core Lipoprotein Classes (5) Lipoproteins are classified into five major families which differ in the amounts of C, TG and types of apoproteins they contain Chylomicrons (CM) Very low density - lipoproteins (VLDL) Intermediate - density lipoproteins (IDL) Low density - lipoproteins (LDL) High density- lipoproteins (HDL) Atherogenic Lipoproteins: Atherogenic lipoproteins that convey lipids into the artery wall Low-density lipoprotein (LDL) main atherogenic lipoprotein (60% to 70% of TC) Very-low-density lipoprotein (VLDL) Lipoprotein a, Lp(a) is a species of LDL that is strongly associated with atherosclerosis and is localized in atherosclerotic lesions Atherogenic Particles VLDL 0.95 VLDL Remnants IDL 1.006 Density, g/mL Chylomicron Remnants 1.02 LDL 1.06 1.10 Chylomicron Chylomicron VLDL VLDL HDL2 Lp(a) HDL3 1.20 5 10 20 40 60 80 1000 Diameter, nm *Key Point:or Lp(a), is a species of LDL that is strongly associated with atherosclerosis and is localised in atherosclerotic lesions. What is LDL - Cholesterol • “Bad” cholesterol • Major C carrier in blood High levels cause slow build up of plaques in the walls of the arteries (atherogenic) A blood clot may form in the area of a plaque and block the flow of blood causing a heart attack or stroke • What is HDL – Cholesterol “Good” cholesterol Carries cholesterol away from the arteries and back to the liver Low HDL indicates a greater risk for CAD Inhibits atherogenesis (accounts for 20% to 30% of TC). **High-density lipoprotein (HDL) inhibits atherogenesis (only accounts for 20% to 30% of TC). Reverse C Transport via HDL Peripheral Tissues Blood Excess Cholesterol Liver Bile ** High-density lipoproteins (HDL) are responsible for movement of most cholesterol from peripheral tissues through the blood back to the liver. Because the liver is the center of cholesterol homeostasis in the body, cholesterol that moves from peripheral tissues to the liver is considered to be moving in the reverse direction. Normal Lipid Profile < 200 Total Cholesterol < 150 TG ‘Ugly’ Lipid < 100 ‘Bad’ Cholesterol LDL > 50 HDL ‘Good’ cholesterol < 30 VLDL is Ugly (TG ÷ 5) • • • • • < 3.5 Total C : HDL-C ratio • (a useful predictor of CHD) | **Lipoprotein disorders are detected by measuring lipids in serum after a 10-hour fast. Risk of heart disease increases with high concentrations of the atherogenic lipoproteins, It is inversely related to levels of HDL, Factors promoting elevated blood lipids: • family history of CAD • smoking (reduced levels of HDL, cytotoxic effects on the endothelium, increased oxidation of lipoproteins, and stimulation of thrombogenesis) • hypertension • obesity • DM • inactivity / lack of exercise • alcohol intake ( increases TGs) ** family history of CHD Cigarette smoking is a major risk factor for coronary disease. It is associated with reduced levels of HDL, cytotoxic effects on the endothelium, increased oxidation of lipoproteins, and stimulation of thrombogenesis hypertension low HDL-C. , obesity diabetes mellitus (source of oxidative stress) inactivity/ lack of exercise Alcohol intake ( increases TGs) Cholesterol Metabolism: Cholesterol Absorption in the Intestine ** Cholesterol from dietary or biliary sources enters the intestine where the cholesterol is emulsified in the lumen by bile acids to form mixed lipid micelles (micellar cholesterol). Micelles move lipids from the intestinal lumen to the mucosal surface where they are absorbed by enterocytes.8,9 Once inside epithelial cells, free cholesterol is esterified and assembled into chylomicrons (CMs), which are secreted into the lymph and subsequently enter the blood.6 Cholesterol-lowering drugs have been developed to act at various steps in this process. Resins increase fecal excretion of bile acids, while plant stanols interfere with the formation of micellar cholesterol ** Lipids originate from two sources: endogenous lipids, synthesized in the liver, and exogenous lipids, ingested and processed in the intestine. Dietary cholesterol and triglycerides are packaged into chylomicrons in the intestine, before passing into the bloodstream via lymphatics. Chylomicrons are broken down by lipoprotein lipase (LPL) in the capillaries of muscle and adipose tissue to fatty acids, which then enter the cells. The chylomicron remnants, which have lost much of their triglyceride content, are taken up by the liver for disposal. The liver synthesizes triglycerides and cholesterol, and packages them as VLDLs before releasing them into the blood. When VLDLs (which consist mainly of triglyceride) reach muscle and adipose blood vessels, their triglycerides are hydrolyzed by LPL to fatty acids. The fatty acids that are released are taken up by the surrounding muscle and adipose cells. During this process, the VLDLs become progressively more dense and turn into LDLs. While most of the resulting LDLs are taken up by the liver for disposal, some circulate and distribute cholesterol to the rest of the body tissues. HDLs, which are also secreted from the liver and intestine, have the task of preventing lipid accumulation. They remove surplus cholesterol from tissues and transfer it to LDLs that return it to the liver ** The chylomicron remnants (diameter 30-50 nm), still containing their full complement of cholesteryl esters, pass to the liver, bind to receptors on hepatocytes and undergo endocytosis. Cholesterol liberated in hepatocytes is stored, oxidised to bile acids, secreted unaltered in bile, or can enter the endogenous pathway In the endogenous pathway, cholesterol and newly synthesised triglycerides are transported from the liver as VLDL (diameter 30-80 nm) to muscle and adipose tissue, where triglyceride is hydrolysed to fatty acids and glycerol; these enter the tissues as described above. During this process, the lipoprotein particles become smaller (diameter 20-30 nm) but retain a full complement of cholesteryl esters. Consequently, they increase in density to intermediatedensity cholesterol and ultimately LDL-C particles. LDL-C provides the source of cholesterol for incorporation into cell membranes and for synthesis of steroids 1-Chylomicrons (rich in TG) in The intestinal mucosa ,dietary cholesterol and triglycerides are packaged into chylomicrons , before passing into the bloodstream via lymphatics. 2-VLD Lipoproteins VLDL are secreted by liver and export triglycerides to peripheral tissues , lipoprotein lipase degrades TG in chylomicrons, VLDL to Free fatty acids. Chylomicrons lose TG content --------CM remnants bind to specific receptors on thee liver , where the endocytosed VLDL ::::::::::::::::::::::----------LDL bind to specific receptors on the liver, extrahepatic tissue , where the endocytosed 3- LD Lipoproteins Normally, about 70% of LDL is removed from plasma by hepatocytes by receptor-mediated endocytosis. Cholesteryl esters from LDL are hydrolyzed, yielding free cholesterol 4- LP(A) Lipoproteins Lp(a) is found in atherosclerotic plaques and may contribute to coronary disease by inhibiting thrombolysis. 5- HD Lipoproteins This is the good one. HDL also acquires cholesterol from peripheral tissues, protecting the cholesterol homeostasis of cells. Hepatic Cholesterol Metabolism Diet De novo synthesis Cholesterol synthesized in extrahepatic tissues Absorption Liver cholesterol pool Reverse transport Transport Secretion of HDL and VLDL Free cholesterol in bile Conversion to bile salts/acids ** Peripheral tissues produce within cells all the C needed for cellular homeostasis. However, the liver is the only organ that is capable of degrading cholesterol. Treatment Strategies: I. Non- Pharmacological Therapy Therapeutic Lifestyle Changes: # Maintaining ideal body weight # Healthy diet: (_) calories, C-rich meals, saturated fat, alcohol (+) dietary fibers, fruits, vegetables (antioxidants), omega 3 in fish # Regular physical activity Regular exercise also increases circulating HDL-C; drug treatment to increase HDL-C is less established than drugs that lower LDL-C, because until recently such drugs (e.g. fibrates and nicotinic acid derivatives-see below) have had only modest effects on HDL-C, accompanied by effects on LDL-C and triglycerides that complicate interpretation of clinical trials 2-Antioxidants (e.g. vitamin C and vitamin E) are of interest, both because of evidence that they improve endothelial function in patients with increased oxidant stress, and because of epidemiological evidence that a diet rich in antioxidants is associated with reduced risk of coronary artery disease II. Antihyperlipidemic (hypolipidemic ) drugs The risk of CAD is correlated with elevated LDL- C and TGs and with low levels of HDL-C Reduction of LDL- C is the primary goal of antihyperlipidemic therapy Antihyperlipidemic drugs prevent the sequelae of atherosclerosis (heart attacks, angina and stroke) and decrease mortality in patients with a history of CAS and hyperlipidemia Inhibition of Cholesterol Biosynthesis Reductase Inhibitors “ Statins ” ** - COMPETITIVE INHIBITORS OF HMG-COA REDUCTASE (REDUCTASE INHIBITORS; "STATINS") HMG-Co A Reductase Inhibitors: • 3 Hydroxy 3 MethylGlutaryl-Coenzyme A reductase inhibitors or statins are the most effective and best-tolerated agents for treating hyperlipidemia • Statins lower blood C levels by inhibiting hepatic C synthesis Hepatic Cholesterol Synthesis Rate Limiting Only pathway for cholesterol degradation HMG-CoA reductase is the major ratelimiting enzyme in cholesterol synthesis ** Statins are potent competitive inhibitors of 3-hydroxy-3-methyl glutaryl coenzyme A (HMG-CoA) reductase, which catalyzes an early, rate-limiting step in cholesterol biosynthesis. Thus, HMG-Co A is not converted to mevalonic acid Statins: Mechanism of Action LDL Receptor Acetate HMG-CoA Reductase Cholesterol LDL **Statins lower blood C levels by inhibiting do-novo hepatic C synthesis The liver compensates by increasing the number of LDL receptors on the surface of hepatocytes (upregulation of LDL- R) This results in increased removal of LDL from the blood, thereby lowering serum LDL- C levels. Statins cause modest decreases in plasma triglycerides and small increases in HDL. Statins: Mechanism of Action: 1- Inhibition of C synthesis by the liver 2- The liver compensates by increasing the number of LDL receptors on the surface of hepatocytes (upregulation of LDL- R) 3- This results in increased removal of LDL from the blood and lowering of serum LDL- C levels 4(-) production of VLDL because C is required for the synthesis of VLDL which is a precursor of LDL-C 5-Statins cause modest decrease in plasma TG and slight( +) in HDL-c **Effect on LDL-C: Statins decrease LDL-C by two mechanisms: Up-regulation of LDL-R with increase of clearance of LDL-C and decrease LDL-C. Decrease of very low density lipoprotein (VLDL) production because cholesterol is a required component of VLDL which is a precursor of LDL-C Statins: Preparations: • Rosuvastatin (Crestor) • Atorvastatin (Lipitor) • Simvastatin (Zocor) • Pravastatin (Pravachol) • Lovastatin (Mevacor Used alone or with other anti-hyperlipidemic drugs in R/ of elevated plasma levels of LDL-C • Statins: Pharmacokinetics: After oral administration, statins undergo extensive 1st pass metabolism Greatly bound to plasma proteins Many statins are taken orally at bedtime because hepatic C synthesis is maximal between midnight and 2:00 A.M. except atorvastatin taken at any time because of its long half-life (14 hours) ** Their dominant effect is on the liver Hepatic C synthesis is maximal between midnight and 2:00 A.M. Thus, statins with half-lives of 4 hrs or less should be taken at bedtime. Atorvastain with long half-live can be taken at any time. Statins: Advantages: • Statins are the drugs of choice in patients with a high risk of CV disease • Statins reduce MI, strokes, mortality • Statins are the drug of first choice for treating hypercholesterolaemia and moderate Statins: Adverse Effects: • Hepatotoxicity, raised concentrations of liver enzymes (serum aminotransferases) • Myopathy (increased creatine kinase, CK released from muscles) • Rhabdomyolysis: rare • Teratogenicity, statins should be avoided during pregnancy **Myopathy especially when combined with: Other lipid lowering drugs; fibrates Other drugs that are metabolized by 3A4 isoform of cytochrome P450 e.g. erythromycin, cyclosporine, verapamil Statins: Precautions: Baseline determinations of serum alanine aminotransferase (ALT) and CK, must be regularly measured during therapy with statins Hypothyroidism should be treated before the start with treatment with statins? Correction of hypothyroidism may resolve the lipid abnormality **Correction of hypothyroidism may resolve the lipid abnormality Statins: Drug Interactions: Drugs that increase the risk of statin-induced myopathy include: • # Other antihyperlipidemics ( fibrates ) # Drugs metabolized by 3A4 isoform of cytochrome P450: erythromycin, cyclosporine, verapamil # Pravastatin is the drug of choice for use with the above –mentioned drugs why ? Bile Acid – Binding Resins, Cholestyramine & Colestipol Cholesterol Absorption in the Intestine **Cholesterol from dietary or biliary sources enters the intestine where the cholesterol is emulsified in the lumen by bile acids to form mixed lipid micelles (micellar cholesterol). Micelles move lipids from the intestinal lumen to the mucosal surface where they are absorbed by enterocytes.8,9 Once inside epithelial cells, free cholesterol is esterified and assembled into chylomicrons (CMs), which are secreted into the lymph and subsequently enter the blood.6 Cholesterol-lowering drugs have been developed to act at various steps in this process. Resins increase fecal excretion of bile acids, while plant stanols interfere with the formation of micellar cholesterol Resins: Mechanism of Action **Colestyramine and colestipol are anion exchange resins. Taken by mouth, they sequester bile acids in the intestine and prevent their reabsorption and enterohepatic recirculation (Fig. 20.1). The concentration of HDL-C is unchanged, and they cause an unwanted increase in triglycerides. Resins: Mechanism of Action: • They are +ve charged compounds that bind –ve charged bile acids in the small intestine • The resin/bile complex is excreted in the feces preventing the recycling of bile acids (normally over 95% are reabsorbed) • Resins divert hepatic C to synthesize new bile acids thus decreasing hepatocyte C content • A compansatory increase in the synthesis of LDL receptors increases, leading to removal of LDL from the blood Resins : Adverse Effects: • Resins are clinically safe as they are not systemically absorbed – GIT upset: abdominal discomfort, bloating, constipation • Decreased absorption of: fat soluble vitamins (Vitamin A, D, K), some drugs Resins: Drugs interactions: Interfere with the absorption of: • Chlothiazides N.B. wait 1 hour before or 4 hrs after administration of resins • Statins **such as chlorothiazide (Chs 19 and 24), digoxin (Ch. 18) and warfarin (Ch. 21), which should therefore be taken at least 1 hour before or 4-6 hours after the resin Cholesterol Absorption Inhibitors: • : Ezetimibe Cholesterol Absorption Inhibitors LDL Liver Duodenum VLDL Ezetimibe X Jejunum Ileum CM Remnant CM Colon Ezetimibe reduces cholesterol absorption. This decreases the content of cholesterol in chylomicrons. In the circulation, chylomicrons deliver triglycerides to muscle and fat tissue, but return to the liver with a full complement of cholesterol that was absorbed by the intestine. Therefore, ezetimibe reduces the flux of cholesterol from the intestine to the liver. Because this cholesterol is packaged and resecreted by the liver into the blood as VLDL particles, containing apo B-100, and because VLDL particles are the precursor particles of LDL in plasma, reduced flux of cholesterol to VLDL particles will lower LDL cholesterol. This mechanism is distinct from that of statins, which promote the clearance of LDL principally in the liver. Evidence that ezetimibe reduces LDL production may be inferred from a study in which patients with homozygous familial hypercholesterolemia were treated with ezetimibe plus statin therapy. The efficacy of statins is reduced in these individuals, in whom the LDL receptor is functionally absent. However, the efficacy of ezetimibe is largely unaffected. It is important to consider that ezetimibe therapy may lead to increased LDL receptor expression in individuals with functional LDL receptors, and that this may comprise a component of the mechanism by which ezetimibe lowers plasma LDL cholesterol and triglyceride concentrations. Ezetimibe: Mechanism of action Ezetimibe selectively inhibits intestinal absorption of C in the small intestine leading to a decrease in the delivery of C to the liver which triggers the following:1- a compensatory increase in C synthesis (can be inhibited by statins) 2- great expression of hepatic LDL receptors, enhances LDL-C clearance form the plasma **Bile acid sequestrants inhibit absorption of ezetimibe (Don’t give them together) Ezetimibe, statins: Dual Inhibition LDL apoB100 Liver Statin Duodenum X VLDL apoB100 Ezetimibe X Jejunum Ileum CM Remnant apoB48 CM apoB48 Colon **By adding a statin to ezetimibe therapy, we take advantage of two mechanisms. First, the statin promotes clearance of LDL particles from blood into the liver as shown by the white arrow. Second, statins reduce the compensatory response whereby the liver upregulates synthesis to compensate for the reduced flux of cholesterol from the intestine to the liver. The combination of these two therapies would be expected to lead to potent reductions in plasma LDL cholesterol concentrations Niacin (Nicotinic Acid): Water soluble B-complex vitamin Multiple actions Niacin :Mechanism of action 1. Niacin strongly inhibits lipolysis in adipose tissues ( FFA ) 1. Niacin reduces hepatic TG production and VLDL secretion 2. Since VLDL is a precursor of LDL –LDL is reduced 4. Enhances LPL activity which promotes clearance of TGs in CM and VLDL 5. Niacin incrases HDL-C levels **Nicotinamide inhibits hepatic triglyceride production and VLDL secretion (see Fig. 20.1), with reductions in triglyceride and LDL-C including Lp(a), and increase in HDL-C. The mechanism is poorly understood Niacin : Adverse Effects The most common side effect is cutaneous flushing, (which is prostaglandin mediated avoided by low dose aspirin ½ h before niacin) GIT disturbances: Nausea , vomiting ( can be decreased if taken after meal) High doses: Liver toxicity • • • Hyperglycemia Hyperuricemia **Adverse effects include flushing, palpitations and gastrointestinal disturbances. Flushing is associated with production of PGD2 (Ch. 13) and is reduced by taking the dose 30 minutes after aspirin. High doses can disturb liver function, impair glucose tolerance, and precipitate gout by increasing circulating urate concentration Fibric Acid Derivatives: Clofibrate & Gemfibrozil Fibrates :Mechanism of Action Fibrates are agonists of peroxisome proliferator • activated receptors (PPARα) which are a class of intracellular receptors that modulate fat metabolism They increase the activity of lipoprotein lipase • increased catabolism of VLDL and chylomicrons **The mechanism of action of fibrates is complex (see Fig. 20.1). They are agonists for a subset of lipid-controlled gene regulatory elements (PPARs4), PPARα, which are members of the superfamily of nuclear receptors (Ch. 3); in humans, the main effects are to increase transcription of the genes for lipoprotein lipase, apoA1 and apoA5. Fibrates: Pharmacological action a marked reduction in circulating VLDL, and hence TG (due to stimulation of catabolism of VLDL) a modest (approximately 10%) reduction in LDL-C and an approximately 10% increase in HDL-C (by increasing the production of the apoprotein components of HDL) Fibrates : Adverse Effects • GIT (indigestion, abdominal pain, diarrhea) • Muscle: Myositis can occur resulting in weakness and tenderness • Myositis can also be caused by statins , and the combined use of fibrates with statins is therefore generally inadvisable • Clofibrate predisposes to gallstones, and its use is therefore limited to patients who have had a cholecystectomy Thank You