Arterial blood pressure
advertisement

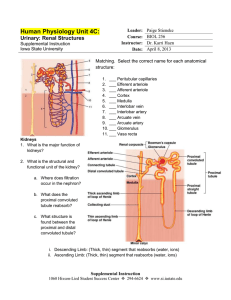
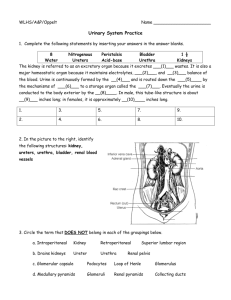
Urinary System Topics & Objectives Kidney 1. • • Anatomy Function 2. Glomerular filtration 3. Tubular reabsorption & secretion 4. Urine excretion & plasma clearance Kidney Functions: Ultimately regulate ECF volume (receive ~ 20% of cardiac output!) 1. Maintain H2O balance in the body 2. Maintain osmolarity 3. Regulation of ECF ions • Na+, Cl-, K+, H+, etc. 4. Maintain plasma volume & acid-base balance 5. Excretion of end products and foreign compounds 6. Producing EPO & renin Renal cortex Renal pyramid Renal medulla Renal pelvis Renal vein Inferior vena cava Urinary bladder Urethra Renal artery Ureter Kidney Aorta Ureter Figure 14.1 Page 513 Nephrons • ~ 1 million within kidney Medulla Cortex Functional unit for urine formation • Arrangement comprises renal cortex & renal medulla • Each nephron composed of: 1. Vascular component 2. Tubular component Proximal tubule Juxtaglomerular apparatus Distal tubule Collecting duct Efferent arteriole Afferent arteriole Bowman’s capsule Glomerulus Cortex Medulla Figure 14.3 Page 514 Peritubular capillaries Loop of Henle To renal pelvis Vascular Component: Glomerulus • Location for H2O and solute filtration from blood Efferent arteriole Afferent arteriole Glomerulus Arterioles • Afferent: to glomerular capillaries • Efferent: drains capillaries No O2 extraction! Peritubular capillaries • Supply renal tissue Peritubular capillaries Tubular Component: Bowman’s capsule • Proximal tubule Distal tubule Juxtaglomerular apparatus Collects fluid from glomerulus Fluid travels to: Bowman’s capsule 1. Proximal tubule 2. Loop of Henle 3. Passes through juxtaglomerular apparatus Vascular/tubular component 4. Distal tubule Loop of Henle Cortical nephron Juxtamedullary nephron Urine Formation Glomerular filtration (protein-free) 1. • • ~ 20% of the plasma (1st step of urine formation) ~ 50 gallons each day (PV ~ 65x/day) Tubular reabsorption 2. • Of the 50 gallons filtered, about 98% reabsorbed Tubular secretion 3. • ~ 80% of the plasma into the peritubular capillaries Efferent arteriole Afferent arteriole Glomerulus 80% of the plasma that enters the glomerulus is not filtered and leaves through the efferent arteriole. GF Bowman’s capsule 20% of the plasma that enters the glomerulus is filtered. TR TS Kidney tubule (entire length, uncoiled) Urine excretion (eliminated from the body) Peritubular capillary To venous system (conserved for the body) Figure 14.6 Page 516 Figure 14.7 Page 517 Blood pathway Filtrate pathway Glomerular capillaries Glomerular filtration Bowman’s capsule Efferent arteriole Venous blood Peritubular capillaries Tubular reabsorption Tubular secretion Tubule (from proximal tubule to collecting duct) Urine Glomerular Filtration Afferent arteriole Efferent arteriole Glomerulus Glomerular capillary Bowman’s capsule Basement membrane Proximal convoluted tubule Figure 14.8 (1) Page 518 Glomerular Filtration Endothelial cell Lumen of glomerular capillary pores Basement membrane podocytes Lumen of Bowman’s capsule Figure 14.8 (3) Page 518 Glomerular Filtration (cont.): Occurs through pressure gradients… 1. Capillary blood pressure (~55mmHg) Favors filtration 2. Plasma osmotic pressure (~30mmHg) Caused by distribution of plasma proteins across glomerular membrane Cannot cross into Bowman’s capsule 3. Bowman’s capsule hydrostatic pressure (~15mmHG) Pressure by the fluid All three pressures determine filtration rate! 1) Changes in BP 2) Osmotic pressure Look at Table 14.1! 3) Hydrostatic pressure GFR Regulation 1. Autoregulation • Prevents spontaneous changes in GFR Vasoconstriction & vasodilation a. Myogenic mechanism – response to stretch b. Tubuloglomerular feedback mechanism 2. Extrinsic sympathetic control • Long-term regulation of arterial BP Sympathetic nervous system (no parasympathetic activity) • Baroreceptor reflex GFR autoregulation 1. Alterations in arteriolar afferent & efferent blood pressures Glomerulus Afferent arteriole Arterial blood pressure (increases blood flow into the glomerulus) Figure 14.10 Page 520 Glomerular capillary blood pressure Net filtration pressure GFR Efferent arteriole GFR autoregulation (cont.) Glomerulus Afferent arteriole Vasoconstriction (decreases blood flow into the glomerulus) Glomerular capillary blood pressure Net filtration pressure GFR Efferent arteriole GFR autoregulation Glomerulus Afferent arteriole Glomerular capillary blood pressure Net filtration pressure Vasodilation (increases blood flow into the glomerulus) GFR Efferent arteriole GFR Autoregulation – Tubuloglomerular feedback 1. Smooth muscle cells within afferent arteriole Granular cells – secretory capabilities Distal tubule Bowman’s capsule 2. Tubular cells (macula densa) Detect changes in the rate of fluid passing through tubule Bring about vasoconstriction or vasodilation Efferent arteriole Afferent arteriole Efferent arteriole Endothelial cell Lumen of Bowman’s capsule Smooth muscle cell Glomerular capillaries Macula densa Podocyte Granular cells Distal tubule Afferent arteriole Arterial blood pressure Driving pressure into glomerulus Glomerular capillary pressure GFR Rate of fluid flow through tubules Stimulation of macula densa cells to release vasoactive chemicals Chemicals released that induce afferent arteriolar vasoconstriction Blood flow into glomerulus Glomerular capillary pressure to normal GFR to normal Extrinsic Control – Baroreceptors Response to decreased BP • Sympathetically induced vasoconstriction • Afferent arterioles (sympathetically innervated) Response to increased BP • Sympathetic stimulation decreases Short-term adjustment for Arterial blood pressure Cardiac output Total peripheral resistance Arterial blood pressure Detection by aortic arch and carotid sinus baroreceptors Sympathetic activity Generalized arteriolar vasoconstriction Afferent arteriolar vasoconstriction Glomerular capillary blood pressure GFR Urine volume Conservation of fluid and salt Arterial blood pressure Long-term adjustment for Tubular Reabsorption Efferent arteriole Afferent arteriole Glomerulus GF Bowman’s capsule TR Peritubular capillary Figure 14.6 Page 516 Tubular reabsorption: Ultimately attempting to maintain body’s internal environment • Proper composition & volume Table 14.2 Filtered substance reabsorbed Filtered substance excreted 99 1 Sodium 99.5 0.5 Glucose 100 0 Urea (waste product) 50 50 Phenol (waste product) 0 100 Water Material must pass through the cells (5 steps) Tubular lumen Peritubular capillary Tubular epithelial cell Plasma Tight junction 1) Luminal membrane 4) Interstitial fluid 2) Cytosol 3) Basolateral membrane 5) Capillary wall Figure 14.17 Page 526 Transepithelial transport Passive & Active Reabsorption 1. Passive: all steps follow electrochemical or osmotic gradients 2. Active: any one of the steps requiring energy • Sodium (80% of kidney’s total energy requirement) ~ 67% in proximal tubule Constant percentage of Na+ reabsorption ~ 25% in loop of Henle ~ 8% in distal and collecting tubules • • Glucose Phosphate Na+ pumped out against concentration gradient • Creates higher concentration in interstitial fluid & allows for passive diffusion back into lumen Lumen Tubular cell Interstitial fluid Diffusion Na+ channel Active transport Basolateral Na+– K+ ATPase carrier Diffusion Figure 14.18 Page 527 Peritubular capillary Distal tubule (~ 8% of total reabsorption) is hormonally regulated • Related to total Na+ load in body Changes in ECF affect osmotic pressures ex: Increased Na+ in ECF causes increased H2O in ECF • Ultimately regulates blood pressure Renin-angiotensinaldosterone system ↑ Atrial natriuretic peptide ↓ Distal tubule Within juxtaglomerular apparatus… Granular cells release renin • In response to fall of NaCl/ ECF volume/ BP • Recognized by intrarenal baroreceptors Sympathetic response to secrete more renin • Ultimately trying to increase plasma volume NaCl / ECF volume / Arterial blood pressure Liver Kidney Adrenal cortex Lungs Kidney H2O conserved Na+ (and CI–) osmotically hold more H2O in ECF Renin Angiotensinogen Na+ (and CI–) conserved Angiotensinconverting enzyme Angiotensin I Angiotensin II Vasopressin Thirst H2O reabsorption by kidney tubules Fluid intake Aldosterone Na+ reabsorption by kidney tubules ( CI– reabsorption follows passively) Arteriolar vasoconstriction Figure 14.19 Page 529 Helps correct NaCl / ECF volume / Arterial blood pressure Helps correct Cardiac atria Atrial natriuretic peptide Na+ reabsorption by kidney tubules Salt-conserving renin-angiotensinaldosterone system Inhibits aldosterone & renin secretion Na+ excretion in urine Smooth muscle of afferent arterioles Afferent arteriolar vasodilation GFR Na+ and H2O filtered H2O excretion in urine Sympathetic nervous system Cardiac output Total peripheral resistance Arterial blood pressure Figure 14.20 Page 530 Glucose and amino acid reabsorption • Na+ dependent secondary active transport Co-transporters that do not require energy • Maximal reabsorption rate depends on substance No energy required Cotransport carrier Luminal border Energy required Na+–K+ pump No energy required Blood vessel Glucose carrier Basolateral border Phosphate & Calcium reabsorption • Dependent upon total body content • Regulated by kidneys Hormonally (parathyroid hormone) Na+ reabsorption responsible for passive reabsorption of Cl-, H2O, and urea H2O (passive) reabsorption • 80% in proximal tubules & loops of Henle Lumen Proximal tubular cell Interstitial fluid Peritubular capillary Osmosis Figure 14.22 Page 533 Water channel Osmosis Hydrostatic pressure Urea (passive) reabsorption • Waste product of protein • Becomes increasingly concentrated Glomerulus Bowman’s capsule Peritubular capillary 125 ml of filtrate Beginning of proximal tubule Na+ (active) H2O (osmosis) Na+ (active) H2O (osmosis) Figure 14.23 Page 534 End of proximal tubule = Urea molecules 44 ml of filtrate Passive diffusion of urea down its concentration gradient Tubular Secretion Efferent arteriole Afferent arteriole Glomerulus GF Bowman’s capsule TS Kidney tubule (entire length, uncoiled) Peritubular capillary Figure 14.6 Page 516 Tubular secretion: Hydrogen ions (H+) • Acid-base regulation throughout the body Potassium (K+) • Early reabsorption into tubules not regulated • Secretion in distal tubules regulated Na+-K+ pump Aldosterone Organic anions & cations • Foreign compounds, chemical messengers Na+/ ECF volume/ arterial pressure Aldosterone dual regulation Renin 1) Na+ & K+ Angiotensin I Plasma K+ Angiotensin II Figure 14.25 Page 536 Aldosterone Tubular K+ secretion Urinary K+ excretion Tubular Na+ reabsorption Urinary Na+ excretion Plasma Clearance Substance: 1) Filtered Peritubular capillary 2) NOT reabsorbed 3) NOT secreted Glomerulus All filtered plasma is cleared of substance Tubule In urine Fig. 14.26a Page 539 Substance: 1) Filtered 2) NOT secreted 3) Completely reabsorbed None of filtered plasma is cleared of substance Substance: 1) Filtered 2) NOT secreted 3) Partially reabsorbed Portion of filtered plasma is cleared of substance Substance: 1) Filtered 2) Secreted 3) NOT reabsorbed ALL of filtered plasma is cleared of substance Regulation of plasma H2O Fluids & solutes • Normal balance in body fluids called isotonic 300 mosm/liter • Hypotonic Too much H2O compared to solute (osmolality < 300) • Hypertonic Too little H2O compared to solute (osmolality > 300) Osmotic gradient maintained in interstitial fluid of medulla • Dependent upon hydration levels From proximal tubule To distal tubule Medullary interstitial fluid Medullary interstitial fluid Descending limb of loop of Henle of juxtamedullary nephron Ascending limb of loop of Henle of juxtamedullary nephron Initial scene Fig. 14.28a (2) Page 542 Step 1 From proximal tubule Step 2 To distal tubule Step 3 From proximal tubule Step 4 To distal tubule Step 5 From proximal tubule To distal tubule Step 6 and on Further regulation Vasopressin • Anti-diuretic hormone from hypothalamus Tubular lumen filtrate Water channel Distal tubular cell Increases permeability of luminal membrane to H2O by inserting new water channels Peritubular capillary plasma Figure 14.29 Page 544