Urinary System
advertisement

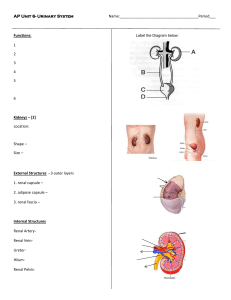
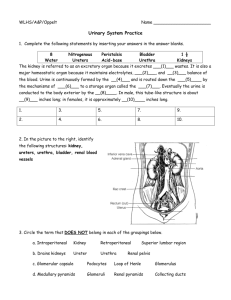
Urinary System Chapter 25 Urinary System Organs • 2 Kidneys forms urine • 2 Ureters transport urine • Urinary bladder stores urine • Urethra transports urine http://findmeacure.com/2008/03/27/hematuriablood-in-the-urine/ Functions • Primary – Filters and excretes toxins, wastes, and ions – Regulates blood volume, pressure, & composition – Maintain balance in blood (H20, salt, acids & bases) • Supporting – Gluconeogenesis w/ fasting – Renin and EPO production – Vitamin D activation Kidney Anatomy (external) • Paired retroperitoneal organs – Right lower b/c liver – Renal ptosis: kidney falls w/ emaciation kinks ureters • Hydronephrosis w/ resulting urine backup • Adrenal glands on top • Renal hilum for vessel entry http://www.arizonatransplant.com/image s/kidney_large_1.JPG Kidney Anatomy (internal) • Renal capsule • Renal cortex • Renal medulla – Renal (medullary) pyramids w/ papilla – Renal columns • Renal pelvis – Walls are smooth muscle peristalsis – Major and minor calyces – Pyelitis when inflamed • Pyelonephritis all inflamed http://tejatechblog.blogspot.com/2010/06/internal-strutureof-kidney.html Blood and Nerve Supply • ¼ total CO – 90% of supply enters cortex • Renal plexus off of celiac plexus (SNS) Nephron • Forms urine from filtrate • Renal corpuscle – Glomerulus is a fenestrated capillaries – Glomerular (Bowman’s) capsule surrounds • Outer sim. squ. & inner podocyte • Renal tubules – PCT: sim. cub. w/ microvilli & mitochondria (cortex) • Increase SA for absorbing H20 & solutes and secretion – Loop of Henle: sim. cub. sim. squ. sim. cub/col • Cortical vs juxtamedullary nephrons http://kvhs.nbed.nb.ca/gallant/b iology/nephron_structure.html – DCT: see PCT, but no microvilli (cortex) • Collecting ducts: sim. cub. (medullary pyramids) – Intercalated cells: abundant microvill and maintain acid/base balance – Principal cells: sparse microvilli and maintain H2O and Na+ balance Nephron Blood Supply • Glomerulus – Afferent artery in from cortical radiate – High BP (wider too) force solute & fluid out – Produces filtrate • Peritubular capillaries – Efferent artery out – Porous & low pressure to reabsorb filtrate (99% to venules) – Modified as vasa recta in juxtamedullary nephrons Juxtaglomerular (JG) Apparatus • Regulate BP and rate of filtrate formation • Specialized cells – Juxtaglomerular (JG) cells in afferent arteriole • Smooth muscle w/ renin secreting granules • Mechanoreceptors for BP – Macula densa in renal tubule • Columnar cells • Chemoreceptors for changing [NaCl] in filtrate http://pclab.cataegu.ac.kr/physiology/Kidney.htm Filtration Membrane • B/w blood and intercapsular space • Layers – Fenestrated epi. of glomerulus • All, but blood cells pass – Basement membrane (b/w epi and podocytes) • All, but smallest proteins • (-) electrical charge assists repulsion of (-) proteins – Podocyte • Filtration slits b/w feet w/additional slits prevent macromolecule escape Kidney Physiology (overview) • Steps – Cell and protein free blood into tubules/collecting duct (1) – Vasa recta reclaims needs and excretes rest • All glucose, AA’s, salt, and 99% H2O (2) – Selective addition of other molecules (3) • Terminology – Filtrate is everything in blood, but protein – Urine is metabolic waste & excess substances Glomerular Filtration (1) • More efficient than other capillaries – High permeability and SA of glomerulus – Glomerular BP higher – Higher net filtration pressure (NFP) • H2O, glucose, AA’s, & nitrogenous waste diffuse – Similar composition of filtrate & blood • Large proteins prevented – Maintain colloid pressure – Prevent all H2O loss from blood – Proteins in blood = imbalance Net Filtration Pressure (1) • Review chpt 19 – Hydrostatic pressure, fluid force on wall • Filters fluids from cells and proteins – Colloid osmotic pressure • Nondiffusible molecules encourage osmosis • Determines filtrate formation (glomerulus) – Glomerular hydrostatic pressure pushes H2O out into intercapsular space – Colloid osmotic pressure of glomerular blood and capsular hydrostatic pressure opposes – NFP = HPg – (OPg + HPc) Glomerular Filtration Rate (GFR) (1) • Volume of filtrate made/min (~ 120 -125 ml/min) • Regulation – SA for filtration – Filtration membrane permeability – NFP • Directly proportional to NFP Intrinsic Regulation of GFR (1) • Myogenic mechanism (JG cells monitor) – Up systemic BP vasoconstrict aff. art. down flow to glomerulus • Decreased GFR protects glomerulus – Down systemic BP reverses • Tubuloglomerular feedback mechanism (macula densa monitor) – GFR up = insufficent reabsorption = high NaCl vasoconstrict aff. art. = down flow to glomerulus • NFP and GFR down to allow time for filtration – Low NaCl reverses – Adaptable except low BP (< 80 mm Hg) = stops Extrinsic Regulation of GFR (1) • SNS maintain systemic BP – NE w/ stress vasoconstrict aff. art. down filtrate formation – Stimulates macula densa and JG cells • Renin – angiotensin mechanism restores blood volume and BP – Renin converts angiotensinogen to angiotensin I • Renin w/ down stretch, activation by macula densa, and Epi receptor stimulation – Angiotensin I to angiotensin II • MAP up (vasoconstriction) • Increase Na+ reabsorbed by PCT • Adrenal cortex release aldosterone Tubular Reabsorption (2) • All glucose and AA’s • H2O and ions dependent on hormones • Can be active or passive – Transcellular route though renal tubule cells • Lumen and basement membrane peritubular capillaries – Paracellular route between renal tubule cells • Tight junctions hinder, but in PCT (Ca2+, Mg2+, K+, & Na+) Na+ Reabsorption(2) • Primary cation in filtrate moved actively – 1° active transport: • Na+-K+ ATPase pumps Na+ into interstitial fluid • Low HP and high OP (undiffusible proteins) into capillaries – 2° active transport • From (-) electrochemical gradient primary set up – Na+ low inside and K+ rapidly leak out – Na+ passively into cells (facilitated diffusion) • Cotransport of glucose, AA’s, lactic acid ,and vitamins More Reabsorption(2) • Passive tubular transport from 1° and 2° active transport – Aquaporins • Responsible for obligatory H2O reabsorption in PCT • Absent in collecting ducts w/o ADH – Up [solute] in filtrate solutes diffuse out • Lipid soluble toxins and drugs also – (-) electrochemical gradient anions diffuse out • Transport maximum (Tm) reflects number of carriers present – Relative to need for molecule – At saturation excess molecules excreted • Diabetes mellitus has increase [glucose] in urine Renal Tubular Activity (2) • PCT (previously) most active • Loop of Henle – Descending H2O in, but no ascend [aquaporins] – Solutes opposite – Role in dilute vs concentrated urine • DCT – Depends on body needs • ADH adds aquaporins = H2O reabsorption up • Aldosterone (renin-angiotensin) up Na+ reabsorption – H2O follows = BP increase • ANP encourages Na + loss – W/ high atrial pressure to drop blood volume and pressure Diuretics (2) • Chemicals enhancing urine output – Substances nor reabsorbed – Substances exceeding renal tubules ability to reabsorb – Substances inhibiting Na+ reabsorption • Alcohol inhibits ADH (H2O reabsorption) • Caffeine, drugs, and other Na+ reabsorption inhibitors • Stop obligatory H2O reabsorption Tubular Secretion (3) • Reabsorption in reverse – PCT mainly, but cortical collecting ducts too • Functions – Eliminate drug bound proteins (not filtered) – Eliminate urea and uric acid (protein metabolism) – Eliminate excess K+ ions – Control blood pH • Up acidity = excess H+ in urine and HCO3- reabsorbed • Down acidity = HCO3- in urine and Cl- reabsorbed Ureters • Two tubes containing a tri-layered wall – Transitional epi. mucosa (kidney pelvis and bladder too) – Inner longitudinal & outer circular smooth muscle • 3rd external longitudinal layer in lower 1/3 – Fibrous CT adventitia • Urine transport through peristalsis – Stretch signal more than neural • Imbalances – Renal calculi (kidney stones) from Ca2+, Mg2+, or uric acid salts precipitating • Bacterial infections, urine retention, high ion levels, and alkaline pH predispose • Cranberry juice acidifies and H2O dilutes Urinary Bladder • Ureteral and urethral orifices form trigone – Common site of infections • Similar tri-layer wall as ureters – Middle layer resemble lower 1/3 ureter = detrusor muscle – Walls w/ rugae for distension Urethra • Trans. pseudostrat. colum. strat. sqam. • Internal urethral sphincter @ junction w/ bladder – Contraction opens • External urethral sphincter @ urogenital diphragm – Levator ani assists • External urethral orifice • Males w/ 3 regions – Prostatic, membranous, and spongy • Imbalances – Dysuria (painful urination) • Indicators: up urgency, frequency, and/or presence of blood – UTI’s from bacterial infections • Females predisposed b/c location, intercourse, wiping • Can cause urethritis, cystitis, pyelitis , inflammation of urethra, bladder, or kidney Urine Characteristics • Color and turbidity – – – – Yellow shades from urochrome, product of Hb breakdown Higher concentration is darker yellow Abnormal colors from foods, bile pigments, or blood Cloudiness could indicate UTI • Odor – Fresh is aromatic, but standing more ammonia b/c bacterial activity – Drugs, vegetables (asparagus & onions), & diseases can alter • pH – Usually ~ 6 – Down w/ acidic diet (high protein, whole wheat) – Up w/ vegetarian diet, prolonged vomiting, and infection • Specific gravity, ratio of urine to dH2O – Higher than 1.0 b/c H2O + solutes – [solutes] determines, 1.001 – 1.035 is normal Chemical Composition of Urine • 95% water • 5% solutes – Nitrogenous wastes • Urea, uric acid, and creatinine (AA, nucleic acid, & CP breakdown respectively) – Na+, K+, Ca2+, Mg2+, HCO3- also • Abnormal amounts, protein, or WBC presence indicates disease/imbalance Micturition (Urination) • Voiding of bladder • Distension of bladder walls initiates spinal reflex – Contraction of external urethral sphincter – Inhibit detrusor muscle and internal sphincter (temporarily) • Reflexive control till ~ 2 or 3 years of age (pons) • Incontinence when can’t control – Laughing and coughing up abdominal pressure – Pregnancy stretches muscles • Urinary retention when can’t go – Common after anesthesia or w/ prostate enlargement