Obsessive-Compulsive Disorder (OCD)
advertisement

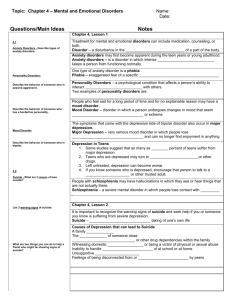
Stages 1 & 2 Anxiety & Mood Disorders Science is a systematic pursuit of knowledge through observation Forming a theory Systematically gathering data to test a theory (Observations must be replicable) Forming a Hypothesis (what should occur if the theory is true) Science proceeds by disproving theories Mental health is a term used to describe either a level of cognitive or emotional wellbeing or an absence of a mental disorder American Psychiatric Association (2000) Diagnostic and Statistical Manual Revision IV, Text Revision Reliability & Validity – Psychometrics DSM is so widely accepted that a psychiatrist must classify their patients’ disorders according to DSM listing number in order to be reimbursed by government of insurance companies Childhood experiences help shape adult personality There are unconscious influences on behaviour The causes and purposes of human behaviour are not always obvious Freud: Psychopathology results from unconscious conflict - Anecdotal evidence, not the scientific method Benefits of gameplay, maintenance of negative schema internal cognitive processes Thorndike (1874-1949): Law of Effect Behaviour that is followed by consequences satisfying to the organism will be repeated, and behaviour that is followed by noxious or unpleasant consequences will be discouraged Skinner (1904-1990): operant conditioning -Positive reinforcement -Negative reinforcement -Automatic reinforcement Problem behaviour is thought to be reinforced by four possible consequences: Getting attention Escaping from tasks Generating sensory feedback (automatic) Gaining access to desirable things or situations Trauma Fear Conduct Disorder Autistic Spectrum Disorder etc Perceiving, recognising, conceiving, judging and Reasoning The learning process is far more complex than stimulus-response associations (behaviourism) The learner is an active interpreter of a situation using past experience in a cognitive set/schema Individuals with psychopathologies tend to focus their attention on threats or anxiety, producing events or situations in the environment. e.g. “The world is a dangerous place” Self-fulfilling prophecy Many people who are depressed believe that they have no important effect on their surroundings regardless of what they do Completing a developmental stage supports the healthy awakening of the next stage Developmental behaviour usually graduates in sequence along with chronological age Needs on lower levels must be met before larger identities can be sustained. Lower identities take their places as no less important, but supporting of a larger and more powerful whole. A.H. Maslow, A Theory of Human Motivation, Psychological Review 50(4) (1943):370-96. Stage 1: Womb – 12 months Stage 2: 6 months – 2 years old Stage 3: 18 months – 4 years old Stage 4: 4 – 7 years old Stage 5: 7 – 12 years old ◦ Motor Functions and security ◦ Mobility and emotion ◦ Will and action ◦ Social Identity ◦ Social contract Stage 6: Adolescence Stage 7: Early Adulthood and Beyond ◦ Reconstitution ◦ Self-knowledge Formation of the physical body during prenatal development and infancy Body growth is rapid at this stage Motor operations: suck, eat, digest, grasp, crawl, stand, walk, manipulate objects, gravity Little awareness of the outside world Fused symbiosis with the mother No separate sense of self Awareness of survival and physical comfort Freud: Oral Stage ◦ Oral cavity is primary focus of libidal energy Characterised by under-nursing: pessimism, envy, suspicion and sarcasm Characterised by over-nursing: optimistic, gullible, admiration for others Conflicts in nursing: deprivation of sensory pleasure and mothering Erikson: Trust vs Mistrust (predictability) Piaget: Sensory-motor stage 1 & 2 ◦ All knowledge is acquired through senses ◦ No sign of object permanence (ability to know that an object exists when it is out of reach of your senses) ◦ Primary circular reactions: repetition of movement (e.g. touching hand and foot) ◦ Vision can follow moving objects Basic psychological identity associates with the physical body. The self is identified with biological urges I Am hungry When to eat, When to rest, Limitations of the body Individuality & The feeling of having the right to exist Independence & The right to take care of ourselves Interaction & The right to have, contain and create Self-preservation Trauma may result in fear, insecurity, confusion Symptoms of disorganisation or depression Feelings of insanity, excessive thinking Little “grounding” – detachment from body and basic consensus reality structures Anxiety in mundane tasks, hypervigilance (high responsiveness to stimuli and constant scanning of environment for threats) Healthy development teaches security, focus, calm and vigilance Visual acuity allows the child to focus on outside objects and gain a wider visual perspective Awareness grows of objects outside of immediate range “Hatching” (Mahler) – moving away from mother in brief episodes of independence Begins to separate self from other eliciting ◦ Fear and excitement ◦ Diversity and choice Primary method of obtaining information about our well-being Primary language prior to verbal language Adds dimension and texture to the mindbody experience Identification with emotional body ◦ I am scared, rather than I have fear Freud: Oral stage ◦ The id: need, sensation and desire is the fundamental cause of motivation. ◦ Seeing something, moving towards it, merging with it (usually through the mouth) Erikson: ◦ Trust vs mistrust ◦ Attachment vs separation Separation from the mother corresponds with separation of self from other Separation from primary attachment figure leads to binary distinctions Duality: good-bad, pleasure-pain, closeness-distance, self-other Trauma may cause numbness (lack of feeling), disconnection with self Difficulty in knowing what we want Unhealthy sexuality Excessive inhibition Guilt ‘Angere’: to choke, to torment Fear: Reaction to immediate danger Anxiety: Apprehension over an anticipated problem Both are adaptive strategies A small degree of anxiety has been found to improve performance on laboratory tasks Specific Phobia Panic Disorder Separation Anxiety Disorder Generalised Anxiety Disorder Obsessive-Compulsive Disorder Post-Traumatic Stress Disorder Phobia: A disruptive fear of a particular object or situation that is out of proportion to any danger posed 3-5% prevalence in children and adolescents There is a great deal of overlap between Axis I Anxiety Disorders and axis II Personality Disorders. Personality disorders (e.g. Borderline, Paranoid, or Avoidant Personality Disorders) may be considered to evoke contrasting ways of perceiving and coping with Axis I disorders Children’s Anxiety may not be focused enough to make specific diagnoses useful for intervention. Culture influences the development of anxiety disorders Alliumphobia Fear of garlic Musophobia Fear of mice Helienophobia Fear of pseudoscientific terminology Arachibutyrophobia Fear of peanut butter sticking to the roof of the mouth www.phobialist.com 2 - 4% prevalence in children More common in girls Some have clear genetic influences (e.g. snakes, injections) 1% prevalence in children and adolescents May lead to substance related disorders and depression 33% concordant with Avoidant Personality Disorder Panic attacks: ◦ Intense apprehension, terror, feelings of impending doom ◦ Choking, nausea, sweating, etc. ◦ Recurrent, uncued panic attacks Agoraphobia ◦ Anxiety about situations in which it would be embarassing or difficult to escape 2 – 4% prevalence from preschool Specific to children Often tied to stressful life event of loss/separation Unable to let go of a worrisome problem Typically chronic, beginning in adolescence or late adolescence 2% prevalence, common onset around age 10 Obsessions: Compulsions: ◦ Intrusive and recurring thoughts, images or impulses that are uncontrollable and come unbidden ◦ e.g. contamination, safety, religious issues ◦ Repetitive, clearly excessive behaviours or mental acts to reduce anxiety caused by obsessive thoughts. ◦ e.g. elaborate rituals of orderliness, repetitive, magically protective acts (superstitions) ◦ Repeatedly checking that these acts are carried out lack of confidence in memory, unduly concerned about gaps in memory 78% of compulsives viewed their rituals as rather silly or absurd, but unable to stop performing them. Rituals allow attention to be drawn away from the obsessions. This perpetuated the obsessions, as thought supression makes thoughts stronger and more frequent Exposure and Ritual prevention (ERP) Also Acute Stress Disorder Extreme response to an actual stressor involving threatened death, serious injury, or threat of these. ◦ E.g. war veterans, rape victims Symptoms are categorised under ◦ Re-experiencing the trauma (e.g. night terrors) ◦ Avoidance of associated stimuli (numbing) ◦ Increased arousal high anxiety (problems with sleep and concentration) Comorbidity ◦ Over 50% of those diagnosed meet criteria for another anxiety disorder ◦ ~60% of people in treatment for Anxiety disorders meet criteria for Depression ◦ Substance disorders and Personality Disorders Women are twice as likely to be diagnosed with anxiety disorders (except in OCD) Syndromes are related to beliefs and attitudes of specific cultures Genetic vulnerability Increased activity in the fear circuit of the brain (amygdala) Decreased functioning of GABA and serotonin, increased norepinephrine activity Behavioural Inhibition – agitation to new stimuli in infancy ◦ Predictive to a 30% level of development of social anxiety Neuroticism ◦ Personality trait with a tendency to react with greater than average negative emotion ◦ Twice as likely to develop into an Anxiety Disorder Cognitive Factors (e.g. attention to cues of threat and low perception of control) Negative Life events Fewer than 20% of people with Anxiety Disorders receive minimally adequate treatment Psychological: Exposure Cognitive reorganization, rationalizing, etc. Medical Treatment: Sedatives, tranquilizers and anxiolytics (“to loosen”) Benzodiaxepines (e.g. Valium, Xanax) GABA. Cognitive and motor side effects memory lapses and addiction Antidepressants, tricyclics and SSRIs (e.g. Fluoxetine, Imipraming – Prozac, Zoloft) Jitteriness, weight gain, high blood pressure, sexual dysfunction Mood Disorders E.g. Depression: Depressed mood, inability to experience pleasure, fatigue, concentration problems and suicidal ideation. Children and adolescents show higher rates of suicide attempts and guilt Major Depressive Disorder (MDD) Diagnosis MDD: Sad mood or loss of pleasure for 2 weeks, with at least 4 other symptoms, such as Changes in sleep pattern Change in appetite Problems with attention Feelings of worthlessness Suicidality Not just a single episode Episodic Disorder: may be periodic, then clear Subclinical depression can remain for years Dysthymic Disorder (Dysthymia): Chronic depression for more than half the time for 2 years Depression One of the most prevalent psychiatric disorders Adults: ~ 16.4% of adults are diagnosed with MDD 2.5% with dysthymia Children & Adolescents: 1% in preschoolers 2-3% in school-age children 7-13% in adolescent (girls) Up to 18% in late adolescents over 20% in 12-16 year olds (Burns and Rapee, 2006) Twice as common among girls than boys (women than men) after the age of 12 Twice as common in women (except for Jewish men) Three times more common in impoverished Socio-economic conditions Depression Age of Onset is in late teens, early 20s, and decreasing Varies culturally People of Mexican descent are more likely to develop MDD if born in USA 1.5% in Taiwan, 19% in Beirut, Lebanon Comorbidity: Two thirds of MDD diagnoses will meet criteria for diagnosis of an anxiety disorder Comorbid with Anxiety and Substance-related disorders Bipolar Disorder Mania: A state of intense elation or irritability lasting from weeks to months Flight of ideas Imprudent sexual activities, over-spending, risk-taking, anger or rage Hypomania: less extreme Bipolar Disorder Bipolar I Disorder: “Manic Depressive Disorder” Bipolar II Disorder Cyclothymic Disorder (Cyclothymia) Chronic mood disorders for at least 2 years Mild alternative depression and mania 1% Prevalence rate for BPI, 40,000 in Ireland 4% for BPII and Cyclothymia Bipolar Disorder Average age is in the 20’s, but is increasing among children and adolescents Equal in men and women (more depression in women) High risk for cardiovascular disease, diabetes, obesity and thyroid disease Associated with creativity and achievement Etiology of Mood Disorders Genetics Neurobiology Social Factors Psychological Factors Etiology of Mood Disorders Genetics: Heritability estimates of 37% for depression (i.e. 37% of variance in whether or not a person will develop depression is explained by genes) 70% concordance rate for Bipolar Disorder in monozygotic twins 25% in fraternal twins 85% heritability estimates for BP Genes may guide the way people regulate emotions or respond to life stressors Etiology of Mood Disorders Neurobiology Amygdala – elevated Hippocampus – diminished Prefrontal cortex – diminished Anterior cingulate – diminished Assessment of how emotionally important a stimulus is Effective focus Making plans based on emotionally relevant cues Etiology of Mood Disorders Neurobiology Seratonin regulates norepinephrine and dopamine. Mania and depression were thought to be symptoms of low levels of seratonin, but the research indicates otherwise Sensitivity of neurotransmitter uptake (Poor seratonin sensitivity) Etiology – Conflicting Research Depression is a result of low absolute levels of neurotransmitters? Antidepressants take 7 to 14 days to relieve depression, by which time the neurotransmitter levels have already returned to their previous state Metabolite studies (enzymes that break down neurotransmitters) are not consistent Caused by low sensitivity of post-synaptic receptors (that detect the presence of a neurotransmitter) Dopamine can be overly sensitive in Bipolar disorder Depleting tryptophan causes temporary depressive symptoms relationship with other neurotransmitters Second messengers adjust postsynaptic receptor sensitivity (e.g. G-proteins – guanine nucleotide-binding proteins) Etiology of Mood Disorders Neurobiology Over-activity of the amygdala (threat) during depression causes oversensitivity to emotionally relevant stimuli Less activity in systems involved in weighing rewards and costs, making decisions and systematically pursuing goals in the face of emotions Feel the fear and Do It Anyway May react with increased emotion, but decreased ability to plan In Bipolar Disorder, there are neurological changes in the sensitivity of the reward system Basal ganglia Increased amygdala Etiology of Bipolar Disorder Mania may be a protective ‘mechanism’ against a painful psychological state Grandiosity Compensation Reflects a disturbance in the reward system (Highly responsive) Marshmallow Test Etiology of Mood Disorders Cortisol (Stress Hormone) Hypothalamus-Pituitary-Adrenocortical Axis (HPA) Signals transmitted from the Amygdala E.g. Cushings Syndrome - Oversecretion of cortisol - Frequent depressive symptoms Dexamethasone Supression Test - Should supress corticol secretion - In some mood disorders, it does not Treatment of Depression Medication: Monoamine Oxidase Inhibitors (MAOIs) Tricyclic Antidepressants Selective serotonin reuptake inhibitors (SSRIs) (e.g. Fluoxetine, Imipramine – Prozac, Zoloft) 50-70% show improvement Suicidality associated with SSRIs Relapse is common after drugs are withdrawn Treatment of Depression Electroconvulsive Therapy (ECT) Only used in cases that do not respond to medication Involve deliberate induction of seizure and momentary unconsciousness by passing a current of 70-130V through the non-dominant brain hemisphere Short-acting anesthetic and strong muscle relaxant administered ECT is the most reliable treatment available for depression with psychotic features We don’t know why it works. Treatment of Bipolar Disorder Medication: Lithium mostly for prevention of manic episodes Lithium toxicity – tremor, nausea, confusion, seizure, coma, death Olanzapine (antipsychotic) e.g. Haldol Treatment of Bipolar Disorder Psychoeducational approaches Family-focused Treatment (FFT) High Expressed Emotion (EE) predicts faster relapse Childhood Depression in Ireland 90% of Irish Child Psychiatrists prescribed psychotropic drugs The prevalence of use of medication was lowest at 8% in Denmark 75% of MDD cases do not receive effective treatment May stop treatment early Too low dosage Childhood Depression in Ireland No anti-depressant medications are licensed for use in children (up to 18 years of age) in Ireland. This is mainly the case because of the expense involved in clinical trials to be undertaken by drug companies to have these products licensed. Some trials are being conducted in the US at the moment. Doctors do have the discretion to prescribe any medication they deem necessary for their patient of any age. The Irish Medicines Board has acknowledged that depression can be a serious condition in children and that drug treatment may be necessary. They are currently working on guidelines and have issued a warning about the use of Seroxat as it increases the risk of agitation. Fitzpatrick Coping with Depression in Young People Treatment of Depression Interpersonal Psychotherapy Focus on current life, rather than trauma Transitions, conflicts, bereavement Decision making, techniques to improve communication etc Prevents relapse Cognitive Therapy Altering maladaptive thought patters More successful than imipramine (tricyclic antidepressant) Mindfulness-based Cognitive therapy Decentered perspective “I am not my thoughts” Etiology of Mood Disorders Social Factors Stressful life events 42-67% of depression occurs within a year of a major stressful life event Long-term chronic stressors e.g. poverty Vulnerability to stress Lack of social support Support minimises the effect of social stressors E.g. 40% prevalence in women without confidants, 4% in women with confidants Interpersonal relations Depressive symptoms elicit negative reactions Excessive reassurance seeking results in rejection Etiology of Mood Disorders Psychological Factors Affect Negative affect: distress and worry Positive affect: happiness, contentment Somatic arousal Negative Affect Positive Affect Somatic Arousal Depressive Disorders High Low Moderate Anxiety Disorders High Moderate High Comorbidity of Depressive and Axiety Disorders High Low High Etiology of Depression Schemata: Hopelessness Theory 1. 2. Pay more attention to negative stimuli Remembers negative information more than positive information Feeling of being in an uncontrollable aversive situation (e.g. abusive family) “Desirable outcomes will not occur” “I cannot change my situation” Neuroticism predicts the onset of depression Remember: Genes + Stressful Life Event risk of depression Nutritional Treatment Potential therapeutic benefit of n-3 polyunsaturated fatty acids (Omega 3) Vitamin B12, B3 - necessary for the synthesis of red blood cells, the maintenance of the nervous system and growth and development in children deficiency of this particular vitamin results in an build up of a compound called homocysteine - this may enhance depression. Depression in Children Early onset depression Depression with an onset in early adolescence Remember: 2% children 4% mid adolescent 18% late adolescent Behaviours to note: Chronic sadness and/or irritability Decline in interest in activity Sleep disturbance, fatigue, appetite change Worthlessness, concentration problems Withdrawn, social exclusion Poor concentration Children 12-20% children and adolescents would be diagnosed with anxiety disorders Parent-Child relationships – criticism, hostility Suicide 10-20% of people report suicidal ideation 2-5% make attempts 7% deliberately harm themselves. Men are 4 times more likely to kill themselves 60% of all suicides are with guns Up to 90% of people who attempt suicide are suffering from mental illness (usually comorbid with Depression or Borderline Personality Disorder) Suicide is now the leading cause of death in young men in the 15-24 year old age range Suicide in Ireland In a study of suicide victims in Dublin over a year it was found that 70% were male, 35% had previously attempted suicide, and 53% saw a Doctor in the previous month. 44% experienced hopeless feelings. The Central Statistics Office at the time the study was done underestimated the suicide rate by 20% An eight year follow-up of attempted suicide found that 2 out of the 26 had died and 19% had further suicide attempts Suicide Possible Reasons Few ties to family or community Atruism: for the good of society Anomic – sudden change in persons relation to society (e.g. in rural china, suicide is one of the leading causes of death) Retaliation – to induce guilt in others To force love/attention from others To rejoin a dead loved one Sociocultural models (suicide rose 12% after Marilyn Monroe’s suicide) Prevention of Suicide Who is at Higest Risk? 1. 2. 3. Desire to escape aversive self-awareness Problem-solving deficits Hopelessness Prevention Reduce intense psychological pain Help the person see options other than suffering Encourage the person to pull back from the selfdestructive act Reasons for Living Inventory Suicide prevention centres Phone services Prevention of Suicide Psychoeducation “Mental Health Literacy”, help-seeking adolescents do not consider doctors appropriate helpers for a depressed peer in-adequate service provision Cognitive Restructuring Exposure Modeling Skills training Relapse prevention Prevention of Suicide