259_2010_1666_MOESM1_ESM
advertisement

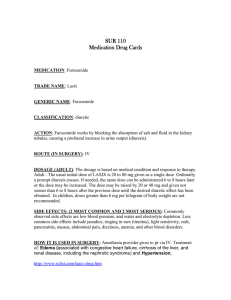
Human Biodistribution and Radiation Dosimetry of Novel PET Probes Targeting the Deoxyribonucleoside Salvage Pathway APPENDIX Dosimetry, calculation of Absorbed Dose, and estimation of Effective Dose Imaging and quantification. Imaging was performed on an ECAT/EXACT HR+ positron emission tomograph (CTI/Siemens, Knoxville, TN) [1]. This scanner acquires 63 image planes simultaneously and has an axial field of view of 10.2 cm; 6 or 7 bed positions were sufficient for acquisition of the upper body (base of skull to mid-thigh) in our 9 volunteers. A transmission scan was acquired first for correction of photon attenuation; a duration of 4 min per bed position was used. Transmission images were segmented into bone, soft tissue and lung, before they were applied as attenuation correction on a voxel basis. After intravenous administration of the 18 F labeled probe, three emission scans were acquired, starting at approximately 20, 45, and 70 minutes. Duration of emission scans was also 4 minutes per bed position. PET images were reconstructed using an iterative algorithm (OSEM, 2 iterations, 8 subsets). A 6 mm Gaussian smooth was applied post reconstruction. The axial slices were assembled into a volume set of the upper body, from which coronal and sagittal planes could be extracted. The voxel size of the reconstructed data was 3.5 x 3.5 x 2.4 mm. The spatial resolution of the scanner in the center of the field of view was 6 mm FWHM with the used iterative reconstruction and Gaussian smooth. Voxel content represents the local concentration of activity in Bq/mL. Appendix PET Probes Targeting Nucleoside Salvage -1- Image analysis The average concentration of 18 F in source organs was retrieved from the images by drawing a region of interest on axial planes. A 50% isocontour of the maximum uptake in an organ, and consecutive planes above and below, was used to include the entire organ, creating a 3D volumeof-interest (VOI). The average activity concentration inside the VOI was calculated and expressed in Bq/mL. The VOIs were generated on the first upper body scan and copied to the second and third scan, i.e. the organ volume remained constant for each individual volunteer. The bladder was an exception, where a 25% isocontour was used to create the VOI and the actual volume was measured separately for each scan (bladder volume increased with time). Previously, we have shown that the volume and activity concentration can be estimated accurately with PET by measuring spheres and cylinder inserts in a Jaszczak phantom. By filling the spheres with 11 C and the background with 18 F, the contrast could be varied over a wide dynamic range, and spheres went from hot to cold lesions in a few hours [2, 3]. The effect of iterative reconstruction on contrast was also investigated [3]. The Nijmegen group argued in their perspective that isocontours at a given percentage of the tumor maximum were accurate to measure tumor size and tracer uptake [4]. VOIs were drawn over the heart, kidneys, liver, marrow (spine), muscles (deltoid and trapezius), salivary glands, spleen, and urinary bladder. The scans did not include the upper part of the head. Since the probe does not cross the blood-brain-barrier, cerebral uptake does not contribute to internally absorbed dose. No scans of the lower extremities below the mid thigh were obtained, but activity concentration in the muscles and bone marrow were assumed to be the same as measured in the upper body. Appendix PET Probes Targeting Nucleoside Salvage -2- In this way, a time-activity-curve (TAC) was generated where the 18 F activity concentration is depicted as a function of time for the various organs. Dosimetry The OLINDA/EXM (Organ Level Internal Dose Assessment Code, Vanderbilt University, 2003) program was used to estimate the absorbed dose for the source and target organs [5]. The input variables for this program are the residence times for each organ and remainder of the body. The program uses standardized human phantoms, of which we used the adult male or adult female, to estimate the absorbed dose for every organ and the total body. In the following paragraph the basics of the equations and calculations are shown. MIRD schema (Medical Internal Radiation Dose) The fundamental quantity is absorbed dose D given by equation 1. D d dm Eq. 1. Where d is the mean energy imparted to matter of mass dm by ionizing radiation. The unit for absorbed dose is joule per kilogram or Gray (Gy). According to the simplified equations of the MIRD schema [6] the mean absorbed dose in a target organ is given by equation 2. Mean Absorbed Dose = D = A0 S Eq. 2 A0 is the administered activity is the residence time S is the dose to the target from unit cumulated activity in the source, also called S-value Appendix PET Probes Targeting Nucleoside Salvage -3- Radiopharmaceuticals used in nuclear medicine, emit either photons or electrons, for which the radiation weighting factor is equal to 1. If E is the mean energy per particle, and n is the number of particles emitted per transition, then Mean Absorbed Dose = A~ n E / m Eq. 3 A~ is cumulated activity in the source n is number of particles per transition E is mean energy per particle is the fraction of emitted energy that is absorbed in the target m is the mass of the target The radiation absorbed dose is the radiation energy imparted to unit mass, which is given by equation 3. Substituting S = n E m yields, Mean Absorbed Dose = A~ S Eq. 4 Thus, S reflects the mean absorbed dose in the target per unit cumulated activity in the source. It is convenient to express the dose to the target per unit administered activity, by defining the residence time = A~ / A0 Eq. 5 The mean dose to the target organ per unit administered activity then becomes: D / A0 = S Eq. 6 The above equation 6 is the same as equation 2 and forms the basis of estimating absorbed doses and S-values by the OLINDA/EXM program. Derivation of the above equations can be found in the MIRD primer [6]. More information about the OLINDA/EXM program can be found in reference [5] and in the help files of the program. Appendix PET Probes Targeting Nucleoside Salvage -4- Average organ activity in Bq/mL was measured with VOI analysis at different time points (vide supra), and was not decay corrected. Organ mass was estimated to be a fraction of body weight as given in ICRP-53 [7] and OLINDA/EXM. The actual weight of a volunteer was used to estimate his or her organ masses, which were then ‘mapped’ to the standard phantom applied in OLINDA/EXM. Separate phantoms were used for the adult male (73.7 kg) and adult female (56.9 kg). The actual volume of the urinary bladder was derived from the VOI analysis, by calculating the number of voxels enclosed within the VOI [2]. Measured activity in Bq/mL multiplied by organ mass yields total organ activity, and was measured as a function of time. The tissue density was assumed to be 1 kg/L (the bladder consists of muscle and is filled with urine). As explained above, an individual TAC had only 3 measured data points related to the 3 scan times. For most organs the probe uptake is rapid, and we assumed instantaneous uptake for our calculations. This corresponds to Fig 5 in the MIRD primer for absorbed dose calculations (page 11 of reference [6]). Measured organ activity was extrapolated to the zero time point by assuming a linear function. After the last measured point it was hypothesized that the activity remained in the organ and decayed with the physical half-life of 18 F. Thus, the TAC for an organ consisted of an initial curve of 4 points followed by an exponential with a half-life of 109.77 min (Fig A1, red curve). Appendix PET Probes Targeting Nucleoside Salvage -5- Figure A1 Time activity curves of the liver (red) and bladder (blue). The column width indicates the duration of the scans. The activity at time zero is 0 for the bladder, and is extrapolated from the measured data with a linear fit for other organs. After the last data point the activity decays with the physical half life of 18F. For the bladder a different TAC was hypothesized. At the time of injection (T0) the bladder activity is zero, which increased linearly to the first measured time point. After the last time point, it was assumed that bladder contents remained the same with physical decay only. Thus, the bladder TAC consists of a triangular upslope, followed by 3 measured points, and terminated with an exponential (Fig A1, blue curve). Appendix PET Probes Targeting Nucleoside Salvage -6- Figure A2 Computation of the time-integrated activity or accumulated activity. Numerical integration over equidistant time intervals of 10 min (width of a column). The dimension of the accumulated activity is [ MBq hr ], expressed as MBq-hr by the OLINDA/EXM program. These organ activity curves, i.e. 3 measured data points supplemented with 1 extrapolated point at T0 for organs, and zero activity for the bladder, and ending with the exponential of late decay (Fig A1), were interpolated over equidistant time intervals of 10 minutes. Numerical integration of this interpolated TAC provided the area under the curve (Fig A2). Dividing this integral, i.e. accumulated activity in [ MBq hr ], by the administered activity A0 [ MBq ] yields the residence time in hours [ MBq hr / MBq ] = [ hr ]. The remainder of the body was calculated by subtracting the activity in the organs from the total body activity. The residence times were Appendix PET Probes Targeting Nucleoside Salvage -7- entered into OLINDA/EXM and the absorbed doses calculated for the target organs taking all source-target combinations into account. Absorbed doses were estimated for each volunteer individually. In MIRD pamphlet-21 [8] the residence time is called ‘time-integrated activity coefficient’. Equivalent dose, H and Effective dose, E The formalism of ICRP-103 [9] was used to estimate the effective dose for the reference person as proposed in 2007. Recently, the SNM MIRD committee proposed to adopt the same terminology in order to standardize nomenclature [8]. The mean absorbed dose per organ and the remainder of the body are the starting point. These doses are estimated using the MIRD formalism as implemented in OLINDA/EXM. The equivalent dose HT in a tissue or organ [9] is defined as H T wR DT , R Eq. 7 R The radiation weighting factors wR are 1 for our 18 F probes emitting positrons, which are annihilated to twice as many photons. DT,R is the mean absorbed dose from radiation R in an organ or tissue T. Compared to prior publications, ICRP-103 [9] has increased the number of tissues to 15 with varying weighting factors in order to calculate the effective dose E. Please note that we use a bold E to distinguish effective dose from mean energy per transition in equation 3. E wT wR DT , R wT H T T R Eq. 8 T The tissue weighting factors wT can be found in Tables A.4.3 (page 182) and B.2 (page 261) of ICRP publication 103 [9]. There are four groups of tissues with different weighting factors. The number of tissues within a group varies from 2 (gonads) to 14 (remainder). A total of 15 tissues Appendix PET Probes Targeting Nucleoside Salvage -8- is used to compute the value of equation 8. The effective dose is calculated separately for a male and female reference person. Averaging the two provides the effective dose E for the reference person. This value is used for radiation protection and dose estimates. The unit for effective dose is Sievert (Sv). Absorbed doses are estimated for a reference male and female as shown in Fig B.3 of ICRP-103 (p 274 of reference [9]). The arithmetic mean provides the estimate for a reference person and is no longer gender dependent. For L-18F-FAC we had only female volunteers and for L-18FFMAC only males. Thus, we had to generate data for a reference male with L-18F-FAC and reference female with L-18F-FMAC. Residence times were calculated using the average activity concentration of L-18F-FAC and assuming a male person for organ masses, as well as average activity concentration of L-18F-FMAC and assuming a female person. Subsequently, OLINDA/EXM was run using the adult male or adult female phantom. In this way, male and female reference persons were available for all probes, and effective dose could be estimated for the reference person [9]. The effective dose per administered activity was 5.24E-03, 7.55E-03, and 9.10E-03 mSv/MBq for 18F-FAC, L-18F-FAC and L-18F-FMAC, respectively. FAC-probes In the current study 3 probes labeled with probe. 18 F were investigated; there were 3 volunteers per The residence time for various target organs was calculated by measuring the accumulated activity per unit administered activity. Residence time was measured for each probe and every volunteer separately, i.e. modified by individual mass (= weight if tissue density = 1 kg/L). The ’s were the input for the OLINDA/EXM program and the internal absorbed radiation dose was calculated for the target organs. Appendix PET Probes Targeting Nucleoside Salvage -9- The highest estimated absorbed dose was for the bladder with L-18F-FMAC. Administering an activity of 400 MBq to this volunteer would furnish an absorbed radiation dose of 27 mGy to the bladder. This ‘worst case scenario of no voiding’, is still within the allowed limit of 50 mSv as established by guideline 21CFR361.1 [10] Specifically, 21CFR361.1 or Code of Federal Regulations Title 21 Part 361 Section 1 states: “For a single radiopharmaceutical administration, the absorbed dose should not exceed 3 rem for the whole body, active blood forming organs, lens of the eye and gonads; or 5 rem for any other organ.” Please note that 3 rem = 30 mSv and 5 rem = 50 mSv. This guideline is applied to new and/or investigational radiopharmaceuticals by the RDRC (Radioactive Drug Research Committee) at UCLA for research studies in human subjects. The organ receiving the highest absorbed dose, i.e. the critical organ, was the bladder wall for all three probes. Thus, 400 MBq administered activity would result in an effective dose of 2.1, 3.6, and 3.6 mSv for 18F-FAC, L-18F-FAC and L-18F-FMAC, respectively [10]. More realistic scenarios will also include urinary voiding and excretion from organs. In other words, our calculation method is overly conservative. Assuming similar uptake in the bone marrow of the legs as in the spine, for instance, is also overestimating the absorbed dose. On the other hand, the bladder maximum is probably underestimated since we did not know the true maximum bladder uptake in 6/9 volunteers. Since we did not perform precise dosimetry, but wanted to demonstrate that we are staying within the limits of our RDRC, this conservative approach is warranted. Appendix PET Probes Targeting Nucleoside Salvage -10- In clinical practice, the radiopharmaceutical will be removed faster from the body than assumed in our dosimetry. In reality, the actual absorbed organ and body doses will be lower than estimated here. References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Wienhard K, Dahlbom M, Eriksson L, Michel C, Bruckbauer T, Pietrzyk U, et al. The ECAT EXACT HR: performance of a new high resolution positron scanner. J Comput Assist Tomogr. 1994;18:110-8. Schiepers C, Brown M, McNitt-Gray M, Rogers S, Phelps M, Dahlbom M. Combining PET and CT: effect on volume measurements. In: Metzler SD, editor. Norfolk, VA,: Ieee; 2003. p. 1102-4 vol.2. Schiepers C, Brown M, Rogers S, McNitt-Gray M, Phelps ME, Dahlbom M. Lesion size and volume in combining PET and CT: Phantom experiments. Journal of Nuclear Medicine. 2002;43:14P. Visser EP, Boerman OC, Oyen WJ. SUV: from silly useless value to smart uptake value. J Nucl Med.51:173-5. doi:jnumed.109.068411 [pii] 10.2967/jnumed.109.068411. Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 2005;46:1023-7. doi:46/6/1023 [pii]. Loevinger R, Budinger TF, Watson EE, Society of Nuclear Medicine (1953- ). Medical Internal Radiation Dose Committee. MIRD primer for absorbed dose calculations (Revised Edition). New York, NY: Society of Nuclear Medicine; 1991. ICRP-53. Radiation dose to patients from radiopharmaceuticals. ICRP Publication 53. Approved by the Commission in March 1987. Elmsford, NY: Pergamon Press; 1988. Bolch WE, Eckerman KF, Sgouros G, Thomas SR. MIRD Pamphlet No. 21: A Generalized Schema for Radiopharmaceutical Dosimetry-Standardization of Nomenclature. Journal of Nuclear Medicine. 2009;50:477-84. doi:DOI 10.2967/jnumed.108.056036. ICRP-103. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37:1-332. doi:S0146-6453(07)00031-0 [pii] 10.1016/j.icrp.2007.10.003. FDA. 21CFR361 - Code of Federal Regulations Title 21 Part 361 Section 1. HHS; 1975 (Revised April 1, 2010). Appendix PET Probes Targeting Nucleoside Salvage -11-