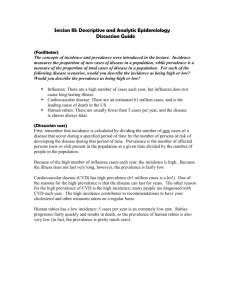
Risk and frequency: incidence and prevalence
advertisement

Risk and frequency: incidence and prevalence Raj Bhopal, Bruce and John Usher Professor of Public Health, Public Health Sciences Section, Division of Community Health Sciences, University of Edinburgh, Edinburgh EH89AG Raj.Bhopal@ed.ac.uk Risk and frequency: incidence and prevalence- educational objectives You should understand: Risk is the likelihood of an individual developing a disease/problem Epidemiology measures risk (actual or absolute measures) and how this compares with other populations (relative measures). A risk factor is a characteristic associated with disease. The meaning of the words rate, ratio and proportion in everyday and epidemiological language. The principal measures of risk- the incidence and prevalence rates. Risk Risk in everyday language and in epidemiology Risk markers Associations Risk factors Causes Numbers, proportions, ratios and rates Epidemiology needs the number and characteristics of disease cases, of people with risk factors, and of the population from which the above people derive. Numbers of cases, or people with the risk factors comprise the numerator-the top half of the fraction- the population from which they come is the denominator-the bottom part in of factions The fraction, numerator divided by the denominator, is usually called the rate in epidemiology A ratio is one number in relation to another, and a rate is a ratio. Measures in Epidemiology Numbers of cases Proportional mortality Proportional mortality ratio Actual/Crude prevalence and incidence rates Specific prevalence and incidence rates Standardised rates Standardised ratios Relative risk Odds ratio Attributable risks Numbers needed to treat and prevent Life years lost Disability adjusted life year (DALY) Quality adjusted life year (QALY) Incidence rate Dictionary definition: the act of happening, and, the occurrence or the extent or frequency of occurrence Count of new cases over a period of time in a population size defined by characteristics (age, sex, etc), and place and time boundaries Obtain from disease register or cohort study or trial The two key formulae are: New cases Population-at-risk, or New cases Time spent by the study population at-risk Denominator What might be your denominator for a study defining the incidence of (a) infant mortality (b) the sudden infant death syndrome (‘cot’ death) and (c) myocardial infarction? What information would you need to make a rational choice? Incidence rates: a variety of names Incidence density is also known as incidence rate, person-time incidence rate, instantaneous incidence rate, hazard rate and force of morbidity or mortality Cumulative incidence is usually simply referred to as incidence rate (or rarely, cumulative proportion) Incidence: shifting population at risk Assume that the incidence rate of a disease is 20% per year and we follow up 100 people How many people at an six months, on average, will develop the disease? For diseases that occur only once how many are at risk after six months, or a day, or in the first hour? How many are at risk after one month? How should we take into account this shifting denominator in large studies? Incidence density is a measure of the occurrence of disease over a period of time approaching zero Figure 7.1 very short time span approaching zero Incidence density time Figure 7.2 Numerator: 0 cases 1 2 3 Denominator: (years of observation 0 10 assuming each case occurs at midstudy start - year 1 point of interval and contributes 0.5 years) 10 19.5 - year 2 19.5 28 - year 3 28 35.5 - year 4 time Incidence density and a person-time denominator If the incidence is constant over time then the incidence density is estimated by the probability that a person well at that time will develop the disease in a moderate interval of time, i.e. not a period approaching zero. When might this assumption of constant incidence be true? In this circumstance using a person-time denominator estimates the average value of the incidence density. The person-time denominator is the amount of time that the study population has spent at risk (diseasefree, or alive, in the case of mortality studies) When would this approach be either inappropriate or unnecessary? Person denominator (cumulative incidence rate) Ranges from 0 to 1 Measures absolute risk (probability) of disease e.g. cases/10,000 people = 5% Can be used to construct relative risks Incidence rates can be calculated with population estimates, e.g., from a census, and disease from a register Can only be used with cohort studies where study participants are enrolled at about the same time Time denominator (estimate of incidence density) Ranges from zero to infinity Not clearly interpreted as a measure of absolute risk e.g. 50 cases per 1,000 person-years Can be used to construct relative risks Migration loss to follow-up and migration data are not usually available in population estimates so person-time cannot be calculated Can be used either when enrolment is at about the same time or when enrolment is spread over time Prevalence rate Count of cases (new and old) at a point in time in a population size defined by characteristics (age, sex, etc) and place Obtained from cross-sectional studies or disease registers The formula is: All cases Population-at-risk Types of prevalence For prevalence, unlike incidence, include those people who have the disease in the denominator The point prevalence rate comprises all the cases of a disease that exist at a point in time Period prevalence is all cases whether old, new or recurrent, arising over a defined period, say a year or two. The denominator is the average population over the period (or midpoint estimate) Lifetime prevalence is the proportion of the population who have ever had the disease Figure 7.4 Incident cases Prevalent cases Deaths, emigrations and recovery Figure 7.7 Recoveries Births Population reservoir Immigration Incident cases Emigrant cases, unmeasured cases Prevalent cases occurring abroad, and deaths Emigrant and nonmeasured cases, Recoveries deaths Incidence and prevalence and preferences For studies of the causes of disease the incidence rate is preferred. Why? For studies of the burden of diseases of short duration e.g. measles incidence is also preferred. Why? The prevalence rate is generally preferred as the measure of burden for long-lasting diseases. Why? For health behaviours and other disease risk factors prevalence is the preferred measure (even in studies of disease causation). Why? Overall and specific rates The rate can be subdivided by any characteristic of epidemiological interest eg age, sex, place and time. Such rates are called specific rates, e.g. age or sex specific rates Specific rates permit rational and easy comparison of disease patterns in different places and times for they can be directly compared with each other Why is this not true for overall rates? Prevalence and incidence In fixed populations, the prevalence is equal to the incidence rate x average duration of disease It follows that incidence rate = point prevalence rate duration; and duration = point prevalence rate ÷ incidence rate. In a dynamic population, however, the prevalence of a disease cannot be predicted from knowledge of the incidence (or vice versa) because of migration into and out of the population, deaths, changing disease rates, changes in prognosis and error in measuring the incidence (or prevalence) accurately. In practice, either the prevalence and incidence are both measured or a choice of one is made. Entering diagnosis on a death certificate: exercise A person who has a feverish illness diagnosed on laboratory tests as influenza, develops cough and shortness of breath shown to be pneumonia, followed by a deep venous thrombosis. The doctors suspect that pulmonary embolus has occurred but before it can be confirmed by tests, the patient collapses and dies unexpectedly. Assume that there is no post-mortem because the relatives refuse permission Complete the specimen death certificate in table 7.5 for the above person. Take care to order the causes as instructed and note that as the death certificate states that the underlying cause of death goes on line 1(c) Table 7.5 Specimen death certificate: exercise I (a) Disease or condition directly leading to death (b) Other disease or condition, if any, leading to I(a) (c) Other disease or condition, if any, leading to I(b) II Other significant conditions CONTRIBUTING TO THE DEATH but not related to the Disease or condition causing it CAUSE OF DEATH The condition thought to be the "Underlying Cause of Death" should appear in the lowest completed line of Part Death certificate Compare your completed certificate with mine below. 1a Pulmonary embolus b Pneumonia c Influenza 11 Deep venous thrombosis Coding of diagnosis: exercise Based on your completed death certificate code the causes of death (see table 7.6). Reconsider your choice of order of causes of death after reading the coding rule from the ICD (see table 7.6). Death certificate: coded Compare your completed certificate with mine below. 1a Pulmonary embolus (I26) b Pneumonia (J18) c Influenza (J10.0) 11 Deep venous thrombosis (I80.1) Lower limb amputation: measurement To calculate the frequency of disease we need rules to judge whether a case is a case, whether it is new or old and to decide whether to include recurrences Each study will need to make this decision in the light of its aims Decisions are not easy except for the incidence of mortality, diseases which are irreversible e.g. amputation of a limb, disease which usually occur only once e.g. measles, or diseases agreed by definition or convention to be lifelong diseases, e.g. diabetes So how will we define lower limb amputation and measure its prevalence? Where will the data come from? Figure 7.1 Hospital discharge data N = 165 Limb fitting centre N = 66 65 26 8 75 17 15 85 Operating theatre records N = 192 Class exercise: angina A health authority (or an equivalent body such as an insurance agency or a managed care organisation) serving 500,000 people wishes to cost and plan a service for the medical and surgical management of angina of the population, with particular emphasis on the numbers of cases requiring surgery. You are invited to assist. Consider the general principles that you would apply to the task. Consider the relative merits of incidence, point prevalence, period prevalence and lifetime prevalence. Summary Risk is the possibility of harm In epidemiology risk is the likelihood of an individual in a defined population developing a disease or other adverse health problem In epidemiology the association between risk of disease and both individual and social characteristics (risk factors) is often the starting point for causal analysis Measures of risk include incidence and prevalence rates. The incidence rate focuses on new cases prevalence on all cases In a fixed population prevalence rate is equal to the incidence rate multiplied by the duration of the disease