Review of Antiplatelet and Anticoagulation Therapy
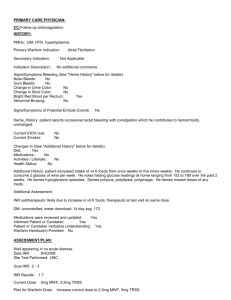
advertisement
Review of Antiplatelet and Anticoagulation Therapy Steven W. Harris MHS, PA-C Coagulation system • Two pathways – Intrinsic – Extrinsic – Combine into the final common pathway • Intrinsic: clotting factors are intrinsic to the blood – Measured by aPTT • Extrinsic: triggered by the addition of thromboplastin (tissue factor) – Measured by PT What happens? • Damage to endothelium: 1. platelets adhere 2. Trigger formation of factor VII and X 3. VII and X facilitate conversion of prothrombin to thrombin 4. Converts fibrinogen to fibrin 5. Activation of more platelets 6. Platelets release thromboxane A2,serotonin, and ADP which enhance platelet aggregation. What Happens? • Direct tissue damage in the body – Release of thrombin which activates the fibrinogen system – Aids in activation of platelets – Continue cascade. Why and What • Prevention and treatment of thromboembolic events – – – – CVA MI DVT PE • Types of drugs – Heparins – Anticoagulants – Antiplatelets Heparins • • • • Heparin sodium: Enoxaparin sodium: Fondaparinux: Dalteparin: generic Lovenox Arixtra Fragmin • Have no effect on existing clots, but prevents or retards formation of new thrombi. Oral Anticoagulants: only one • Warfarin • Jantoven • Coumadin • Blocks vitamin K binding sites inhibiting synthesis of vit-K dependent factors – II, VII, IX, X • Do not lyse existing thrombi, but prevent extension and formation Antiplatelets • • • • • • • • • Acetylsalicylic acid (ASA) Clopidogrel Ticlodipine Dipyridamole Tirofiban * Eptifibatide* Anagrelide* Abciximab* Dipyridamole + ASA *IIb/ IIIa Inhibitors Aspirin, Ecotrin Plavix Ticlid Persantine Aggrastat Integrilin Agrylin ReoPro ??? Antiplatelets • ASA: inhibits cyclooxygenase – Prevents formation of thromboxane A2 • Clopidogrel: inhibits ADP binding to platelet receptor Prevent platelet aggregation Effect is irreversible Antiplatelets • IIb/ IIIa Inhibitors: newest group of antiplatlets – Reversibly inhibit platelet aggregation through blocking the binding site of glycoprotein IIb/IIIa and fibrinogen. Heparins: Indications • Acute treatment of thromboembolic event – (DVT, PE, CVA, ACS) • • • • • Early treatment of AMI Cardiac surgery Vascular surgery During and after PTCA, PCI Select pts with acute stroke, unstable angina, atrial fibrillation, precardioversion, prophylaxis of DVT and PT in high risk pts. Heparin • Begin with standard loading dose of 5000 U IV – Then follow appropriate dosing schedule – Commonly 15-25 U/kg/hr. • Monitor with aPTT • Caution: HIT – Treat with direct thrombin inhibitors • argatroban or bivalirudin (angiomax) Low Molecular Weight Heparins (LMWH) • Enoxaparin, Fondaparinux – Advantages of predictable anticoagulant effect – Dosing – Inhibits generation of thrombi higher in the clotting cascade • Prophylaxis – Lovenox 30 mg – Lovenox 40 mg • Therapeutic Dose – Lovenox Warfarin: Mechanism of Action • Warfarin interrupts the ability to recycle Vit K • Vitamin K dependent procoagulants: – Prothrombin (Factor II) – Factor VII – Factor IX – Factor X • Vitamin K dependent Anticoagulants: – Proteins S and C. Pharmacokinetics Therpeutic challenges – Delayed optimal anticoagulant effect • Has no effect on available clotting factors • No anticoagulant effect until these decay – 5-7 days until clotting factors are at a minimal level – Warfarin half-life of 36 to 48 hours • Persistent anticoagulant effect after warfarin is discontinued Considerations • hepatitis, cirrhosis, and cancers that degrade liver function result in a deficiency of clotting factors • green leafy vegetables & fish oil contain Vitamin K • normal flora – produce Vitamin K (broad spectrum antibiotic effects) • Multiple Drug interactions Monitoring • Prothrombin Time – Used to assess Extrinsic Pathway – Normal range 12-15 seconds – Must be used with INR for Coumadin Dosing to “Standardize Test” • The normal range for the INR is 0.8-1.2 – Patients fondly refer to this test as “Pro-time” – Adjusted from the INR value Monitoring • Warfarin is a narrow therapeutic index drug (NTI). When the INR falls below 2.0 thrombosis risk increases and when the INR rises above 4.0 serious bleeding risk increases. • Target INR ranges: • Disease INR Range DVT/PE 2.0-3.0 Atrial Fibrillation 2.0-3.0 Myocardial Infarction 2.0-3.0 Mechanical Heart Valves 2.5-3.5 Initiating Therapy • Contraindications • Initiating a Plan: – Rx for medication • interactions – Pt Education • Diet • Timing • Warning signs – Laboratory findings • Baseline PT INR, aPTT, platelet count • Follow-up PT INR Drug Interactions Drugs That May Lengthen PT • Antibiotics • Antiarrhythmics • Others – Anabolic steroids Omeprazole Cimetidine Phenytoin Clofibrate Tamoxifen Disulfiram Thyroxine Lovastatin Vitamin E (large doses) Drugs That May Shorten PT • Alcohol Penicillin • Antacids Rifampin • Antihistamines Spironolactone • Barbiturates Sucralfate • Carbamazepine Trazodone • others Dietary Interactions • Patients taking warfarin should eat a diet that is constant in vitamin K. • Minimize changes in intake of green leafy vegetables (spinach, greens, and broccoli), green peas, and oriental green tea – http://www.med.umich.edu/cvc/services/site_ant icoag/healthprof.html Co-morbid Conditions • Expect a longer prothrombin time in patients with CHF, jaundice, hepatitis, liver failure, diarrhea, or extensive cancer or connective tissue disease. • Expect a longer prothrombin time when patients receiving warfarin are hospitalized for any reason. • Metabolic alterations can affect the prothrombin time. • Expect a longer prothrombin time in patients with hyperthyroidism or high fever. • Expect a longer prothrombin time in elderly patients. • Expect a shorter prothrombin time in patients with hypothyroidism Initiating Warfarin Therapy • Large loading doses do not markedly shorten the time to achieve a full therapeutic effect. • Initiate therapy with the estimated daily maintenance dose (2-5 mg daily) • Elderly or debilitated patients often require low daily doses of warfarin (2-4 mg daily). Initiating Warfarin Therapy • In Patient • Check daily PT INR – – – – 5mg Day 1 5mg Day 2 2-5mg Day 3* 2-5 mg Day 4* • Concurrent LMWH or Heparin management Initiating Warfarin Therapy • Out patient • 2-5 mg daily • Check INR on day 3-5 – Insure anticoagulation achieved and stable • Recheck one week from initiation • Additional anticoagulant? – Urgent anticoagulation needed • Concurrent LMWH or Heparin – Non-urgent anticoaglation • Start with anticipated daily dose Initiating Therapy • Contraindications • Initiating a Plan: – Rx for medication • interactions – Pt Education • Diet • Timing • Warning signs – Laboratory findings • Baseline PT INR, aPTT, platelet count • Follow-up PT INR Case 1 • 70 y/o male with new dx atrial fibrillation. Hemodynamically stable, HR 70 bpm. • PMH: CAD • Habits: occasional ETOH, eats a healthy diet. Case 2 • 55 y/o healthy female. Recently returned from visiting tour de France . Found to have unilateral R leg swelling, U/S comes back confirming R DVT. • PMH: G2 P2 Case 3 • 80 y/o female with SOB, tachypnea, tachycardia, hypoxia. Found to have massive PE on CT angiogram. • PMH: Prior DVT no workup, DM, HTN. Case 3 • 80 y/o female with SOB, tachypnea, tachycardia, hypoxia. Found to have massive PE on CT angiogram. • PMH: Prior DVT no workup, DM, HTN. • Day 3 INR is 2.0 • Day 4 INR is 3.2 Altering Chronic Therapy • Significant changes in INR can usually be achieved by small changes in dose (15% or less). • 4-5 days are required after any dose change or any new diet or drug interaction to reach the new antithrombotic steady state. • Patients are confused by multiple dosages of pills. Antiplatelets • • • • Aspirin Clopidogrel Aggrenox Ticlid Resources Clotting Cascade • Web based aid to help determine dose http://warfarindosing.org/Source/Home.aspx • ACC foundation guide to therapy http://circ.ahajournals.org/cgi/content/full/107/12/1692 ?eaf • Excellent Resource for managing Warfarin http://www.med.umich.edu/cvc/services/site_anticoag/ healthprof.html