Huntington*s Disease
advertisement

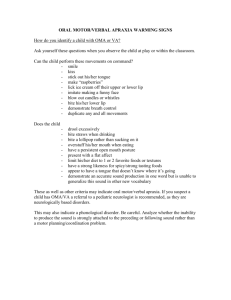
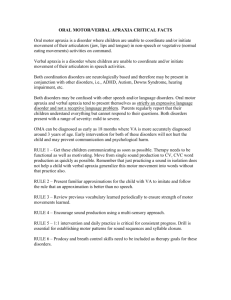
Motor Control and Disorders Basal Ganglia Disorders • Parkinson’s Disease • Huntington’s Disease • Tourette’s Syndrome Parkinson’s Disease • damage to cells in the substantia nigra pars compacta (80% of dopamine producing cells are damaged – therefore, dopamine deficiency results). • typically idiopathic (of unknown cause) but can result from encephalitis, toxins, trauma (e.g., boxer’s encephalopathy), designer drugs (MPTP). Parkinson’s Disease Parkinson’s Disease • hypokinesia (akinesia, bradykinesia) • lack of movement or limited movement • resting tremors (pill rolling) • cogwheel rigidity • intermittent in nature • posture and gait disturbances PD - hypokinesia • hypokinesia – difficulty initiating movements. • bradykinesia – a slowness in control of movements (bradyphrenia – slowness of thought). • Parkinsonian mask – frozen facial features. PD - tremors • resting tremors – can be used to determine the laterality of PD – PD is most often unilateral but can be bilateral. • pill-rolling tremor – refers to a stereotypical movement made at rest that resembles rolling a pill between your fingertips and thumb. PD – cogwheel rigidity • increased muscle tone in extensor and flexor muscles leads to resistance to movement. • cogwheel rigidity refers small rigid steps in a passive movement (i.e., when the examiner tries to move the patient’s arm she encounters resistance leading to brief rigid steps rather than smooth movement). PD – postural disturbances • bent posture, sometimes to point of falling. • head droops. • postural adjustments can be impaired – may fall when bumped. PD – gait disturbances • shuffling gait – very different from Ozzy’s wide based gait! • gradually diminishing distance between steps. • eventual freezing. • virtual lines as treatment. Treatment of PD • L-dopa • dopamine does not cross the blood-brain barrier. • L-dopa is a precursor for dopamine. • anti-cholinergic drugs reduce the uptake of acetylcholine restoring the balance between dopamine and acetylcholine (a balance disrupted by the depletion of dopamine). • new combination medicines like Stalevo. Treatment of PD • pallidotomies – Michael J Fox has two! • the internal globus pallidus is lesioned during stereotaxic surgery. • stimulated first to determine region responsible for excessive inhibition. • internal stimulators – like a brain pacemaker. An electrode implanted in the thalamus stimulates the motor pathways (bypassing the connections from the basal ganglia). Pallidotomies and stimulators Huntington's Disease Huntington's Disease Healthy brain • inherited, autosomal dominant, degenerative disease affecting the caudate. • St. Vitus’ dance – 16th century Germany. Dance in front of statue for good health – mistaken for chorea. • Huntington’s chorea • begins between 30 and 45 years of age. • death occurs 10 to 15 years after onset. HD brain Huntington’s Disease Huntington’s Disease • Hyperkinesias • chorea (Greek for dance). • athetosis – writhing contractions. • contorted postures – head, arms and legs in constant motion. • also demonstrate bradykinesia – a slowness in control of movement. • more closely associated with degeneration of the caudate. • disease was brought to North America by Europeans fleeing persecution (burned as witches). • European origin to HD in Asian cultures too. Huntington’s Disease – Nancy Wexler • Nancy Wexler is a scientist whose mother died of HD. • she and her colleagues isolated the gene responsible for HD in a small community in Venezuela with the highest incidence of HD in the world. • made a genetic test for the gene possible – can determine whether you will develop HD. Parkinson’s and Huntington’s Disease Tourette’s syndrome • named after French neurologist Georges Gilles de la Tourette. • primary symptoms are vocal and motor “tics”. • involuntary, repetitive often compulsive movements. • begins in childhood (≈ 11 years old). • face and head are typically affected, although in more severe forms the limbs and whole body can be involved. Tourette’s syndrome • complex movements (e.g., touching) can also be evident. • echolalia – the repetition of what has just been heard. • coprolalia – obscene utterances. Tourette’s syndrome • associated with a gene on chromosome 18 – possible sex-linked trait expressed higher in males. • also associated with OCD (25% manifest full symptoms of OCD) – tics often have a compulsive element to them. • treatment involves dopamine antagonists (anti-dopamine). • not generally associated with major cognitive impairment. • tics may subside somewhat with age with severity of childhood tics not predictive of recovery. Cortical movement disorders • hemiplegia – paralysis arising from motor strip lesions. • apraxia – impaired sequential and gestural movement control arising from left inferior parietal lesions. • optic ataxia – poor control of movements in the periphery arising from bilateral superior parietal injury. • alien hand syndrome – anarchic control of contralateral hand. Alien (anarchic) Hand • “la main étrangerè”. • patient feels their hand behaves in a foreign or uncooperative manner. • unco-operative movements are nevertheless purposeful. • related to intermanual conflict in which hands behave at cross purposes to one another. • arises from medial frontal cortex (SMA) and anterior corpus callosotomies. Anarchic hand is almost always unilateral usually left hand in right handers and can occur for feet as well! Apraxia a = without praxis = action • impairment of learned actions (e.g., gestures, tool use, skilled, purposeful movements) and sequencing of movements that can not be explained by a loss of muscle tone, weakness, somatosensation, comprehension. • like many neuropsychological disorders apraxia is diagnosed by exclusion. • term apraxia introduced by Hugo Karl Liepmann (1863 – 1925). Apraxia • typically arises from left inferior parietal lesions. • bilateral – both hands are apraxic. • often co-occurs with aphasia – so comprehension must be distinguished from poor execution of motor commands. Apraxia Ideomotor apraxia – inability to carry out a simple motor activity in response to a verbal command (can’t mime the use either). Ideational apraxia – inability to carry out a sequence of actions that are components of a behavioural script. • anatomy is very complex (most strokes cause some degree of apraxia. • may involve disconnection of motor cortical areas from the rest of cortex. Brain areas involved in motor control Review Questions 1 ) A primary symptom of Huntington's disease is A) akinesia. B) dystonias. C) tremor at rest. D) difficulty initiating movement. E) uncontrollable movements. 2 ) Apraxia is characterized by A) the inability to perform properly a learned, skilled movement B) an impairment in learning a skilled movement C) muscle weakness D) motor paralysis E) an impairment in motor coordination 3) The slowness of movement noted in Parkinson’s disease reflects A) damage to frontal cortex neurons that plan motor movements B) damage to the primary motor cortex C) loss of inhibition to the motor cortex D) damage to dopamine neurons that normally facilitate motor movements E) loss of inhibition of the ventromedial system from the GPi. Review Questions 4 ) The aim of pallidotomy is to damage the ________ in order to ________ . A) external division of the globus pallidus; remove inhibition of the motor cortex B) nigrostriatal bundle; balance the inputs to the globus pallidus C) internal division of the globus pallidus; increase the inhibition of the motor cortex D) internal division of the globus pallidus; remove inhibition of the motor cortex E) external division of the globus pallidus; increase excitation of the motor cortex 5 ) An impairment of the ability to execute a learned movement is termed A) paralysis. B) Parkinsonism. C) apraxia. D) coordination deficit. E) a learning deficit.