document
advertisement
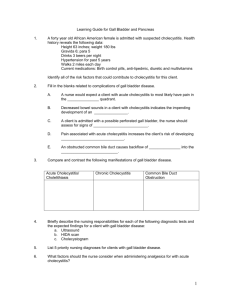
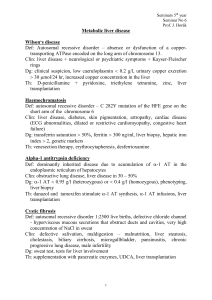
Cholecystitis :Introduction Background Cholecystitis is defined as inflammation of the gallbladder that occurs most commonly because of an obstruction of the cystic duct from cholelithiasis. Ninety percent of cases involve stones in the cystic duct (ie, calculous cholecystitis), with the other 10% of cases representing acalculous cholecystitis.1 Although bile cultures are positive for bacteria in 50-75% of cases, bacterial proliferation may be a result of cholecystitis and not the precipitating factor. Risk factors for cholecystitis mirror those for cholelithiasis and include increasing age, female sex, certain ethnic groups, obesity or rapid weight loss, drugs, and pregnancy. Acalculous cholecystitis is related to conditions associated with biliary stasis, including debilitation, major surgery, severe trauma, sepsis, long-term total parenteral nutrition (TPN), and prolonged fasting. Other causes of acalculous cholecystitis include cardiac events; sickle cell disease; Salmonella infections; diabetes mellitus; and cytomegalovirus, cryptosporidiosis, or microsporidiosis infections in patients with AIDS. Pathophysiology Acute calculous cholecystitis is caused by obstruction of the cystic duct, leading to distention of the gallbladder. As the gallbladder becomes distended, blood flow and lymphatic drainage are compromised, leading to mucosal ischemia and necrosis. A study by Cullen et al demonstrated the ability of endotoxin to cause necrosis, hemorrhage, areas of fibrin deposition, and extensive mucosal loss, consistent with an acute ischemic insult.2Endotoxin also abolished the contractile response to cholecystokinin (CCK), leading to gallbladder stasis. Although the exact mechanism of acalculous cholecystitis is unclear, a couple of theories exist. Injury may be the result of retained concentrated bile, an extremely noxious substance. In the presence of prolonged fasting, the gallbladder never receives a CCK stimulus to empty; thus, the concentrated bile remains stagnant in the lumen. Frequency International Cholelithiasis, the major risk factor for cholecystitis, has an increased prevalence among people of Scandinavian descent, Pima Indians, and Hispanic populations, whereas cholelithiasis is less common among individuals from subSaharan Africa and Asia.3,4 Mortality/Morbidity Most patients with acute cholecystitis have a complete remission within 1-4 days. However, 25-30% of patients either require surgery or develop some complication. Patients with acalculous cholecystitis have a mortality rate ranging from 10-50%, which far exceeds the expected 4% mortality rate observed in patients with calculous cholecystitis. Emphysematous cholecystitis has a mortality rate approaching 15%. Perforation occurs in 10-15% of cases. Race Populations at the lowest risk reside in sub-Saharan Africa and Asia. In the United States, white people have a higher prevalence than black people. Sex Gallstones are 2-3 times more frequent in females than in males, resulting in a higher incidence of calculous cholecystitis in females. Elevated progesterone levels during pregnancy may cause biliary stasis, resulting in higher rates of gallbladder disease in pregnant females. Acalculous cholecystitis is observed more often in elderly men. Age The incidence of cholecystitis increases with age. The physiologic explanation for the increasing incidence of gallstone disease in the elderly population is unclear. The increased incidence in elderly men has been linked to changing androgen-to-estrogen ratios. Clinical History 1. The most common presenting symptom of acute cholecystitis is upper abdominal pain, often radiating to the tip of the right scapula. Most patients with acute cholecystitis describe a history of biliary pain. Some patients may have documented gallstones. Acalculous biliary colic also occurs, most commonly in young–to–middle-aged females. The presentation is almost identical to calculous biliary colic with the exception of reference range laboratory values and no findings of cholelithiasis on ultrasound. Frequently, the pain begins in the epigastric region and then localizes to the right upper quadrant (RUQ). Although the pain may initially be described as colicky, it becomes constant in virtually all cases. Signs of peritoneal irritation may be present, and, in some patients, the pain may radiate to the right shoulder or scapula. 2. Nausea and vomiting are generally present, and patients may report fever. 3. In elderly patients, pain and fever may be absent, and localized tenderness may be the only presenting sign. Patients with acalculous cholecystitis may present similarly to patients with calculous cholecystitis, but acalculous cholecystitis frequently occurs suddenly in severely ill patients without a prior history of biliary colic. Often, patients with acalculous cholecystitis may present with fever and sepsis alone, without history or physical examination findings consistent with acute cholecystitis. 4. Cholecystitis is differentiated from biliary colic by the persistence of constant severe pain for more than 6 hours. Physical 1. Physical examination may reveal fever, tachycardia, and tenderness in the RUQ or epigastric region, often with guarding or rebound. 2. A palpable gallbladder or fullness of the RUQ is present in 30-40% of cases. 3. Jaundice may be noted in approximately 15% of patients. 4. The absence of physical findings does not rule out the diagnosis of cholecystitis. Many patients present with diffuse epigastric pain without localization to the RUQ. Patients with chronic cholecystitis frequently do not have a palpable RUQ mass secondary to fibrosis involving the gallbladder. 5. Elderly patients and patients with diabetes frequently have atypical presentations, including absence of fever and localized tenderness with only vague symptoms. 6. Murphy sign, which is specific but not sensitive for cholecystitis, is described as tenderness and an inspiratory pause elicited during palpation of the RUQ. Causes 1. Risk factors for calculous cholecystitis mirror those for cholelithiasis and include the following: o Female sex o Certain ethnic groups (see Race) o Obesity or rapid weight loss o Drugs (especially hormonal therapy in women) o Pregnancy o Increasing age 2. Acalculous cholecystitis is related to conditions associated with biliary stasis, to include the following: o Critical illness o Major surgery or severe trauma/burns o Sepsis o Long-term TPN o Prolonged fasting 3. Other causes of acalculous cholecystitis include the following: Cardiac events, including myocardial infarction Sickle cell disease Salmonella infections Diabetes mellitus Patients with AIDS with cytomegalovirus, cryptosporidiosis, or microsporidiosis 4. Idiopathic cases exist. Differential Diagnoses Abdominal Aortic Aneurysm Gastroesophageal Reflux Disease Acute Mesenteric Ischemia Gastritis, Acute Amebic Hepatic Abscesses Hepatitis, Viral Appendicitis Myocardial Infarction Biliary Colic Nephrolithiasis Biliary Disease Pancreatitis, Acute Cholangiocarcinoma Peptic Ulcer Disease Cholangitis Pneumonia, Bacterial Choledocholithiasis Pregnancy and Urolithiasis Cholelithiasis Pyelonephritis, Acute Gallbladder Cancer Renal Disease and Pregnancy Gallbladder Mucocele Renal Vein Thrombosis Gallbladder Tumors Gastric Ulcers Workup Laboratory Studies 1. A retrospective study by Singer attempted to determine a set of clinical and laboratory parameters that could be used to predict the outcome of hepatobiliary scintigraphy (HBS) in all patients with suspected acute cholecystitis.5 The results of the study showed that, in 40 patients with pathologically confirmed acute cholecystitis, fever and leukocytosis were absent at the time of presentation in 36 (90%) and 16 (40%) of the patients, respectively. The study also found that no combination of laboratory or clinical values was useful in identifying patients at high risk for a positive HBS finding. 2. Although laboratory criteria are not reliable in identifying all patients with cholecystitis, the following findings may be useful in arriving at the diagnosis: Leukocytosis with a left shift may be observed in cholecystitis. Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels are used to evaluate the presence of hepatitis and may be elevated in cholecystitis or with common bile duct obstruction. Bilirubin and alkaline phosphatase assays are used to evaluate evidence of common duct obstruction. Amylase/lipase assays are used to evaluate the presence of pancreatitis. Amylase may also be elevated mildly in cholecystitis. An elevated alkaline phosphatase level is observed in 25% of patients with cholecystitis. Urinalysis is used to rule out pyelonephritis and renal calculi. All females of childbearing age should have pregnancy testing. Imaging Studies 1. Radiography (without contrast) Gallstones may be visualized in 10-15% of cases. This finding only indicates cholelithiasis, with or without active cholecystitis. Subdiaphragmatic free air cannot originate in the biliary tract, and, if present, it indicates another disease process. Gas limited to the gallbladder wall or lumen represents emphysematous cholecystitis, usually because of gas-forming bacteria, such as Escherichia coli and clostridial and anaerobic streptococci species. Emphysematous cholecystitis is associated with an 2. 3. 4. increased mortality rate and occurs most commonly in males with diabetes and with acalculous cholecystitis. A diffusely calcified gallbladder (ie, porcelainized) most commonly is associated with carcinoma, although one retrospective study by Towfigh found no association between partial calcification of the gallbladder and carcinoma.6 Other findings may include renal calculi, intestinal obstruction, or pneumonia. Ultrasonography Ultrasonography provides greater than 95% sensitivity and specificity for the diagnosis of gallstones more than 2 mm in diameter. Ultrasonography is 90-95% sensitive for cholecystitis and is 78-80% specific. Studies indicate that emergency clinicians require minimal training in order to use right upper quadrant ultrasonography in their practice. Ultrasonographic findings that are suggestive of acute cholecystitis include the following: pericholecystic fluid, gallbladder wall thickening greater than 4 mm, and sonographic Murphy sign. The presence of gallstones also helps to confirm the diagnosis. Ultrasonography is performed best following a fast of at least 8 hours because gallstones are visualized best in a distended bile-filled gallbladder. Hepatobiliary scintigraphy (hepatoiminodiacetic acid [HIDA]/diisopropyl iminodiacetic acid [DISIDA]) HBS has been found to be up to 95% accurate in diagnosing acute cholecystitis. The reported sensitivities and specificities of biliary scintigraphy are in the range of 90-100% and 85-95%. (See the following 2 images.) In a typical study, the gallbladder, common bile duct, and small bowel fill within 30-45 minutes. If the gallbladder is not visualized, intravenous morphine administration can improve the accuracy of HBS by increasing resistance to flow through the sphincter of Oddi, resulting in filling of the gallbladder if the cystic duct is patent. The addition of morphine also reduces the number of false-positive scan results observed in patients who are critically ill and immobilized with viscous bile. CT scan and MRI The sensitivity and specificity of CT scan and MRI for predicting acute cholecystitis have been reported to be greater than 95%.7 Spiral CT scan and MRI (unlike endoscopic retrograde cholangiopancreatography [ERCP]) have the advantage of being noninvasive, but they have no therapeutic potential and are most appropriate in cases where stones are unlikely. Findings suggestive of cholecystitis include wall thickening (>4 mm), pericholecystic fluid, subserosal edema (in the absence of ascites), intramural gas, and sloughed mucosa. CT scan and MRI are also useful for viewing surrounding structures if the diagnosis is uncertain. Procedures 1. Endoscopic retrograde cholangiopancreatography ERCP may be useful in patients at high risk for common duct gallstones if signs of common bile duct obstruction are present. A study performed by Sahai et al found that ERCP was preferred over endoscopic ultrasound and intraoperative cholangiography for patients at high risk for common duct stones undergoing laparoscopic cholecystectomy.8 ERCP allows visualization of the anatomy and may be therapeutic by removing stones from the common bile duct. Disadvantages include the need for a skilled operator, high cost, and complications such as pancreatitis, which occurs in 3-5% of cases. 2. Endoscopic ultrasound-guided transmural cholecystostomy: Studies indicate that this procedure may be safe as initial, interim, or definitive treatment of patients with severe acute cholecystitis who are at high operative risk for immediate cholecystectomy.9 3. Mutignani et al investigated the efficacy of endoscopic gallbladder drainage as a treatment for acute cholecystitis.10 The authors, who conducted the study on 35 patients with the condition and with no residual common bile duct obstruction, found that endoscopic gallbladder drainage was technically successful in 29 patients and, after a median period of 3 days, clinically successful in 24 of them. Four patients died within 3 days after the procedure as a result of septic complications, while a fifth patient accidentally removed a nasocholecystic drain 24 hours after the operation. At follow-up (on 21 patients, after a median period of 17 months), the investigators found that 4 patients had suffered a relapse of either acute cholecystitis (2 patients) or biliary pain (2 patients). Mutignani et al concluded that endoscopic gallbladder drainage appears to be an effective, but temporary, means of resolving acute cholecystitis. Histologic Findings Edema and venous congestion are early acute changes. Acute cholecystitis is usually superimposed on a histologic picture of chronic cholecystitis. Specific findings include fibrosis, flattening of the mucosa, and chronic inflammatory cells. Mucosal herniations known as Rokitansky-Aschoff sinuses are related to increased hydrostatic pressure and are present in 56% of cases. Focal necrosis and an influx of neutrophils may also be present. Advanced cases may show gangrene or perforation. Treatment Medical Care For acute cholecystitis, initial treatment includes bowel rest, intravenous hydration, analgesia, and intravenous antibiotics. For mild cases of acute cholecystitis, antibiotic therapy with a single broad-spectrum antibiotic is adequate. Some options include the following: 1. The current Sanford guide recommendations include piperacillin/tazobactam (Zosyn, 3.375 g IV q6h or 4.5 g IV q8h), ampicillin/sulbactam (Unasyn, 3 g IV q6h), or meropenem (Merrem, 1 g IV q8h). In severe lifethreatening cases, the Sanford Guide recommends imipenem (500 mg IV q6h). 2. Alternative regimens include a third-generation cephalosporin plus Flagyl (1 g IV loading dose followed by 500 mg IV q6h). 3. Bacteria that are commonly associated with cholecystitis include E coli and Bacteroides fragilis and Klebsiella, Enterococcus, and Pseudomonas species. 4. Emesis can be treated with antiemetics and nasogastric suction. 5. Because of the rapid progression of acute acalculous cholecystitis to gangrene and perforation, early recognition and intervention are required. 6. Supportive medical care should include restoration of hemodynamic stability and antibiotic coverage for gramnegative enteric flora and anaerobes if biliary tract infection is suspected. 7. Daily stimulation of gallbladder contraction with intravenous CCK has been shown by some to effectively prevent the formation of gallbladder sludge in patients receiving TPN. Surgical Care Laparoscopic cholecystectomy is the standard of care for the surgical treatment of cholecystitis. Studies have indicated that early laparoscopic cholecystectomy resulted in shorter total hospital stays with no significant difference in conversion rates or complications.11 Wilson et al used decision tree analytic modeling to compare the costeffectiveness and quality-adjusted life years (QALYs) of early laparoscopic cholecystectomy (ELC) and delayed laparoscopic cholecystectomy (DLC) and found that, on average, ELC is less expensive and results in better quality of life (+0.05 QALYs per patient) than DLC.12 For elective laparoscopic cholecystectomy, the rate of conversion from a laparoscopic procedure to an open surgical procedure is approximately 5%. The conversion rate for emergency cholecystectomy where perforation or gangrene is present may be as high as 30%. Some considerations regarding cholecystectomy include the following: 1. Immediate cholecystectomy or cholecystotomy is usually reserved for complicated cases in which the patient has gangrene or perforation. 2. Early operation within 72 hours of admission has both medical and socioeconomic benefits and is the preferred approach for patients treated by surgeons with adequate experience in laparoscopic cholecystectomy.13 3. For patients at high surgical risk, placement of a sonographically guided, percutaneous, transhepatic cholecystostomy drainage tube coupled with the administration of antibiotics may provide definitive therapy.14 4. Results of studies suggest that most patients with acute acalculous cholecystitis can be treated with percutaneous drainage alone.10 5. Contraindications for laparoscopic cholecystectomy include the following: High risk for general anesthesia Morbid obesity Signs of gallbladder perforation, such as abscess, peritonitis, or fistula Giant gallstones or suspected malignancy End-stage liver disease with portal hypertension and severe coagulopathy Consultations Definitive therapy involves cholecystectomy or placement of a drainage device; therefore, consultation with a surgeon is warranted. Consultation with a gastroenterologist for consideration of ERCP may also be appropriate if concern exists of choledocholithiasis. Diet Patients admitted for cholecystitis should receive nothing by mouth (NPO) because of expectant surgery. However, in uncomplicated cholecystitis, a liquid or low-fat diet may be appropriate until the time of surgery. Medication The goals of pharmacotherapy are to reduce morbidity and to prevent complications. Antiemetics Patients with cholecystitis frequently experience associated nausea and vomiting. Antiemetics can help to make the patient more comfortable and can prevent fluid and electrolyte abnormalities. Promethazine (Phenergan, Prorex, Anergan) For symptomatic treatment of nausea in vestibular dysfunction. Antidopaminergic agent effective in treating emesis. Blocks postsynaptic mesolimbic dopaminergic receptors in brain and reduces stimuli to brainstem reticular system. Adult: 12.5-25 mg PO/IV/IM/PR q4h prn Pediatric: <2 years: Contraindicated >2 years: 0.25-1 mg/kg PO/IV/IM/PR q4-6h prn Prochlorperazine (Compazine) May relieve nausea and vomiting by blocking postsynaptic mesolimbic dopamine receptors through anticholinergic effects and depressing reticular activating system. In addition to antiemetic effects, it has the advantage of augmenting hypoxic ventilatory response, acting as a respiratory stimulant at high altitude. Adult: 5-10 mg PO/IM tid/qid; not to exceed 40 mg/d 2.5-10 mg IV q3-4h prn; not to exceed 10 mg/dose or 40 mg/d 25 mg PR bid Pediatric: 2.5 mg PO/PR q8h or 5 mg q12h prn; not to exceed 15 mg/d IV dosing is not recommended for children 0.1-0.15 mg/kg/dose IM; change to PO as soon as possible Analgesics Pain is a prominent feature of cholecystitis. Classic teaching is that morphine is not the agent of choice because of the possibility of increasing tone at the sphincter of Oddi. Meperidine has been shown to provide adequate analgesia without affecting the sphincter of Oddi and, therefore, is the DOC. Meperidine (Demerol) DOC. Analgesic with multiple actions similar to those of morphine. May produce less constipation, smooth muscle spasm, and depression of cough reflex than similar analgesic doses of morphine. Adult: 50-150 mg PO/IV/IM/SC q3-4h prn Pediatric: 1-1.8 mg/kg (0.5-0.8 mg/lb) PO/IV/IM/SC q3-4h prn; not to exceed adult dose Hydrocodone and acetaminophen (Vicodin, Lortab 5/500, Lorcet-HD) Drug combination indicated for moderate to severe pain. Each tab/cap contains 5 mg hydrocodone and 500 mg acetaminophen. Adult: 1-2 tab/cap PO q4-6h prn Pediatric: <12 years: 10-15 mg/kg/dose acetaminophen PO q4-6h prn; not to exceed 2.6 g/d acetaminophen >12 years: 750 mg acetaminophen PO q4h; not to exceed 10 mg hydrocodone bitartrate/dose or 5 doses/24 h Oxycodone and acetaminophen (Percocet, Tylox, Roxicet) Drug combination indicated for relief of moderate to severe pain. Each tab/cap contains 5 mg oxycodone and 325 mg acetaminophen. Adult: 1-2 tab/cap PO q4-6h prn Pediatric: 0.05-0.15 mg/kg/dose oxycodone PO; not to exceed 5 mg/dose of oxycodone PO q4-6h prn Antibiotics Treatment of cholecystitis with antibiotics should provide coverage against the most common organisms, includingE coli, B.fragilis, and Klebsiella, Pseudomonas, and Enterococcu s species. Current Sanford guide recommendations for the treatment of cholecystitis include Unasyn, Zosyn for non–lifethreatening cases of cholecystitis. In life-threatening cases, Sanford recommends Primaxin or meropenem. Alternatives include metronidazole plus a third-generation cephalosporin or Cipro or Aztreonam. Ciprofloxacin (Cipro) Fluoroquinolone that inhibits bacterial DNA synthesis and, consequently, growth, by inhibiting DNA gyrase and topoisomerases, which are required for replication, transcription, and translation of genetic material. Quinolones have broad activity against gram-positive and gram-negative aerobic organisms. Has no activity against anaerobes. Continue treatment for at least 2 d (7-14 d typical) after signs and symptoms have disappeared. Adult: 400 mg IV q12h Pediatric: <18 years: Not recommended >18 years: Administer as in adults Meropenem (Merrem) Bactericidal broad-spectrum carbapenem antibiotic that inhibits cell-wall synthesis. Effective against most grampositive and gram-negative bacteria. Has slightly increased activity against gram-negatives and slightly decreased activity against staphylococci and streptococci compared to imipenem. Adult: 1 g IV q8h Pediatric: 60 mg/kg/d IV divided q8h Imipenem and cilastatin (Primaxin) For treatment of multiple organism infections in which other agents do not have wide spectrum coverage or are contraindicated due to potential for toxicity. Adult: Base initial dose on severity of infection, and administer in equally divided doses; dose may range from 250 to 500 mg q6h IV for a maximum of 3-4 g/d Alternatively, 500-750 mg IM q12h or intra-abdominally Pediatric: Infants >3 months and children <12 years: 15-25 mg/kg/dose IV q6h Fully susceptible organisms: Not to exceed 2 g/d Infections with moderately susceptible organisms: Not to exceed 4 g/d >12 years: Administer as in adults Piperacillin and tazobactam (Zosyn) Antipseudomonal penicillin plus beta-lactamase inhibitor. Inhibits biosynthesis of cell wall mucopeptide and is effective during stage of active multiplication. Adult: 3/0.375 g (piperacillin 3 g and tazobactam 0.375 g) IV q6h Pediatric: 75 mg/kg of piperacillin component IV q6h Ampicillin and sulbactam (Unasyn) Drug combination of beta-lactamase inhibitor with ampicillin. Covers epidermal and enteric flora and anaerobes. Not ideal for nosocomial pathogens. Adult: 1.5 g (1 g ampicillin plus 0.5 g sulbactam) to 3 g (2 g ampicillin plus 1 g sulbactam) IV/IM q6-8h; not to exceed 4 g/d sulbactam or 8 g/d ampicillin Pediatric: <3 months: Not established 3 months to 12 years: 100-200 mg ampicillin/kg/d (150-300 mg Unasyn) IV divided q6h >12 years: Administer as in adults Metronidazole (Flagyl) Imidazole ring-based antibiotic active against various anaerobic bacteria and protozoa. Used in combination with other antimicrobial agents (except Clostridium difficile enterocolitis). Adult: Loading dose: 15 mg/kg or 1 g for 70-kg adult IV 1 h Maintenance dose: 6 h following loading dose, infuse 7.5 mg/kg or 500 mg for 70-kg adult over 1 h q6-8h; not to exceed 4 g/d Pediatric: Administer as in adults Follow-up Further Inpatient Care Objectives during inpatient stay include the following: Correction of fluid and electrolyte abnormalities Antibiotics for complicating infections Performing imaging studies as appropriate (eg, ultrasound, HBS) Cholecystectomy once the patient is stable or percutaneous transhepatic cholecystostomy drainage in unstable high-risk surgical patients Further Outpatient Care In cases of uncomplicated cholecystitis, outpatient treatment may be appropriate. If a patient can be treated as an outpatient, discharge with antibiotics, appropriate analgesics, and definitive follow-up care. Criteria for outpatient treatment include the following: Afebrile with stable vital signs No evidence of obstruction by laboratory values No evidence of common bile duct obstruction on ultrasound No underlying medical problems, advanced age, pregnancy, or immunocompromised condition Adequate analgesia Reliable patient with transportation and easy access to a medical facility Prompt follow-up care Inpatient & Outpatient Medications For outpatient treatment of uncomplicated cholecystitis, the following medicines may be appropriate: Prophylactic antibiotic coverage with Levaquin (500 mg PO qd) and Flagyl (500 mg PO bid), which should provide coverage against the most common organisms Antiemetics, such as oral/rectal Phenergan or Compazine, to control nausea and to prevent fluid and electrolyte disorders Analgesics, such as oral Percocet or Vicodin Transfer Consider patient transfer if the following conditions apply: Appropriate diagnostic resources are not available. Higher level of care is required. Surgeons and/or specialists are unavailable. Deterrence/Prevention 1. Prevention of cholecystitis requires cholecystectomy. 2. In patients who are unstable, percutaneous transhepatic cholecystostomy drainage may be appropriate. 3. Some studies have shown that daily CCK administration may help prevent acalculous cholecystitis in patients at risk. Complications 1. Bacterial proliferation within the obstructed gallbladder results in empyema of the organ. Patients with empyema may have a toxic reaction and may have more marked fever and leukocytosis. The presence of empyema frequently requires conversion from laparoscopic to open cholecystectomy. 2. In rare instances, a large gallstone may erode through the gallbladder wall into an adjacent viscus, usually the duodenum. Subsequently, the stone may become impacted in the terminal ileum or in the duodenal bulb and/or pylorus, causing a gallstone ileus. 3. Emphysematous cholecystitis occurs in approximately 1% of cases and is noted by the presence of gas in the gallbladder wall from the invasion of gas-producing organisms, such as E coli, Clostridia perfringens,and Klebsiella species. This complication is more common in patients with diabetes, has a male predominance, and is acalculous in 28% of cases. Because of a high incidence of gangrene and perforation, emergency cholecystectomy is recommended. 4. Sepsis 5. Pancreatitis 6. Perforation occurs in up to 15% of patients. Prognosis 1. For uncomplicated cholecystitis, the prognosis is excellent, with a very low mortality rate. 2. In patients who are critically ill with cholecystitis, the mortality rate approaches 50-60%, especially in the setting of gangrene or empyema. 3. Once complications such as perforation/gangrene develop, the prognosis becomes less favorable. In patients who are critically ill with acalculous cholecystitis and perforation or gangrene, the mortality rate can be as high as 50-60%. Patient Education 1. Patients diagnosed with cholecystitis must be educated regarding causes of their disease, complications if left untreated, and medical/surgical options to treat cholecystitis. Miscellaneous Medicolegal Pitfalls Delays in making the diagnosis of acute cholecystitis result in a higher incidence of morbidity and mortality. This is especially true for ICU patients who develop acalculous cholecystitis. The diagnosis should be considered and investigated promptly in order to prevent poor outcomes.