Document
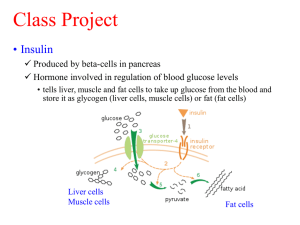
advertisement

بسم هللا الرحمن الرحيم Metabolic syndrome By Dr Amr Abdelmonem,MD. Assistant professor of cardiothoracic anesthesia ,surgical intensive care and clinical nutrition in faculty of medicine, Cairo university Member of North American Association For The Study Of Obesity What is metabolic syndrome? • Metabolic syndrome is a collection of health risks that increase the chance of developing heart disease, stroke, and diabetes. • The condition is also known by other names including Syndrome X, insulin resistance syndrome, and dysmetabolic syndrome. What are these health risks? ATP III Guidelines WHO Guidelines Abdominal Obesity Waist Circumference Men > 40 inches (102 CM) Women > 35 inches (88 CM) Other Variables Triglycerides 150 mg/dL HDL-Cholesterol Men < 40 mg/dL Women < 50 mg/dL Blood Pressure 130/ 85 mm Hg Fasting Glucose 110 mg/dL Waist/Hip Ratio >0.90 >0.85 150 mg/dL <35 mg/dL <39 mg/dL >140/>90 mm Hg 110 mg/dL WHO guidelines also include microalbuminuria (>20 µg/min or albumin:creatinine ratio >30 mg/g). The Pathogenesis of metabolic syndrome Environmental lifestyle-related factors: When we eat ,our bodies break down the food into its basic components ( proteincarbohydrates- fat), and absorbs them into blood stream rise in blood sugar pancreas will release insulin moves sugar into cells either burned for energy or stored away as fat in fat cells or glycogen in liver and muscles Years of dietery abuse in susceptible patients malfunctioning of insulin sensors hyperinsulinemia Continued dietery abuse insulin sensors to sluggish insulin resistance Markers of insulin resistance : Hypertriglyceridemia HDL Hypertension Hyperinsulinemia (>15µu/ml) Marc C,et al. Obes Res.2005;13:703 Abdominal obesity Hyperglycemia Marjo etal , proven liver fat accumulation as an important marker Obes Res 2002; 10: 859 It is now clear that an individual could be insulin-resistant from one of two main reasons 1. he/she could be genetically resistant (like Reaven’s group) or 2. Could acquire the resistance by becoming obese Obesity Lets walk through the fat metabolism pathway and follow the flow of fat molecules: Fat travels in the form of triglycerides at cells ezymatic breakdowen fatty acids enter the cells mitochondria breakdowen fat in order to enter mitochondria ,fats need carnitine insulin inhibits Fat- carnitine shuttle system fats move back into blood Glucagon accelerates this shuttle system Muscle ,liver, kidney, lung, heart and other cells break down fat Fat cells merely store the fat molecules ! Two enzyme systems on the surface of fat cells regulated by insulin and glucagon Insulin stimulates lipoprotein lipase that transports fatty acid into fat cells Glucagon stimulates hormone sensitive lipase that releases the fat from fat cells into the blood Although we cannot control lipoprotein lipase directly, we can control It indirectly by cotrolling the metabolic hormones ,insulin and glucagon DYSLIPIDEMIA Where does cholesterol come from? 80 % comes from the body itself , every cell in the body is capable of making its own cholesterol , most don’t and rely instead on that made in the liver and skin. Cholesterol and triglycerides are insoluble in blood Lipoproteins are envelops that enclose cholesterol and triglycerides Making them soluble in blood,so that they can be transported to tissues Sequence of events in the life of lipoproteins Liver Makes and release VLDL HDL Released to tissues Deposited in coronary arteries TRIGLYCERIDES WITH CHOLESTEROL Removed by liver CholesteroL rich VLDL TRI AND CHOLES LDL More triglycerides release Scavenges cholesterl From tissues carries Through blood Hands it off to Cholesterol Bulk +tri LDL MATURE VLDL Triglycerides Released to blood And tissues When the level of cholesterol inside the cells falls LDL receptors Attach to the surfaces of the hepatic cells invaginate LDL cholesterol By endocytosis Obese patients with insulin resistance have LDL receptors dysfunction Cholesterol synthesis inside the cells depends on an enzyme named 3- hydroxy-3 methyl-glutaryl-coenzyme A reductase Couple of hormones affect the activity of the rate limiting enzymeHMG-CoA reductase INSULIN AND GLUCAGON Hypertension Data from NHANES III show that the (age – adjusted prevalence) Of high blood pressure increases progressively with higher levels Of BMI in men and women High blood pressure is defined as SBP 140 mm Hg or MBP 90 mm Hg or currently taking antihypertensives What is the etiology that connects obesity and hypertension? Hyperinsulinemia and Insulin resistance Mechanism 1. Increased sodium retention 2. Increased sympathetic nervous system activity 3. Alteration in the mechanics of blood vessels Recently Type II Diabetes mellitus •The cells become resistant to insulin that even large amounts cant adequately move the sugar into cells •Resistin is a protein secreted by fat cells as a signal from adipose tissue linking obesity to insulin resistance and type II diabetes Liese et al, Eur J Nutr.2001;40:282 •Increased White blood cell count is correlated with insulin resistance in diabetic obese females Pannacciulli et al,Obes Res.2003;11:1232 Coronary artery disease • Observational studies have shown that overweight,obesity, and VAT are directly related to cardiovascular risk factors ( cholesterol , LDL, triglycerides, hypertension, fibrinogen,hyperinsulinemia , HDL, plasminogen activator inhibitor ) The term "Syndrome X" refers to a heart condition where chest pain and electrocardiographic changes that suggest ischemic heart disease are present, but where there are no angiographic findings of coronary disease. RECENTLY Complement 3 and acute phase proteins is the immunological link between central obesity and CHD Obesity and cardiac dysrhythmias (prolonged Q-T interval) • Q-T interval is usually measured in lead II , and is corrected for heart rate . • Q-Tc= measured Q-T square root of R-R interval • Prolonged Q-T interval reflects prolonged repolarization of the ventricle • Proposed mechanism is increased SNS activity • Recent study had found that Prolonged Q-T interval is associated with abnormal WHR ,higher levels of FFA and hyperinsulinemia in obese women . • Wight loss leads to normalization of Q-Tc with attenuation of hyperinsulinemia Esposito et al,Obes Res.2003;11:653-659 Oxidant Stress Imbalance Between Formation Of Reactive oxygen/nitrogen species (ROS/RNS) And Antioxidants Pathologic stress (TNF Induces monocytes to release mediators and interleukins 1-6-8) Activates PMNs Release ROS(superoxide (O2·-), hydrogen peroxide, hypochlorite, nitric oxide (NO), hydroxyl radical Induce tissue injury by: 1. 2. 3. • • damaging DNA Cross linking cellular proteins Peroxidation of membrane lipids Diminishing membrane fluidity Increasing membrane permeability Oxidant Stress and Obesity •Adipocytes and preadipocytes have been identified as sources of inflammatory cytokines: including TNF , interleukin (IL)1-ß, and IL-6. •Stimuli capable of inducing cytokine release from adipocytes may include: lipopolysaccharides, intracellular triglycerides, and catecholamines We could predict that: •The accumulation of intracellular triglycerides or tissue adiposity promotes increased oxidant stress •Therefore reduction of total body fat through diet and/or exercise may be an effective means of reducing systemic inflammation and oxidant stress. Consistent with this prediction Reductions in plasma markers of oxidant stress and in ROS generation by isolated leukocytes have been observed after 4 weeks of energy restriction and weight loss. Dandona et al. J Clin Endocrinol Metab,2001; 86:355-363 Good news Physical activity •Decreases adipose derived inflammatory mediators •Activates signaling pathways that lead to increased synthesis of intracellular antioxidants and antioxidant enzymes and decreased ROS production Miyazaki et al, Eur Appl Physiol.2001; 84:1-6 Pischon et al, Obes Res.2003;11:1055 A novel pathway to the manifestations of metabolic syndrome(2004)