Ondansetron in Pediatric Gastroenterititis – Who Needs It?
advertisement

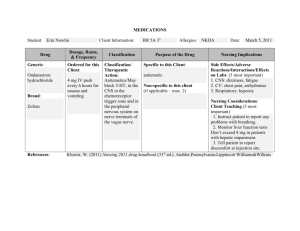
Gord McNeil MD, FRCPC Current recommendation for antiemetics in pediatric acute gastroenteritis (AGE). Use of oral replacement therapy in pediatric AGE. Why is ondansetron different? Review of literature on ondansetron use in AGE. Review side effects and costs of ondansetron. Should there be a new consensus statement on ondansetron in pediatric AGE? Bottom line 5 year old boy, previous well with vomiting X 3, diarrhea X 2 in last 24 hours. Clinically looks well with minimal dehydration. 3 yr old female with vomiting X 7 and diarrhea X 8 in last 24 hours who “vomits every time we give her anything”. Mild to moderate dehydration. 18 month old boy with profuse watery diarrhea, greater then 30 times with vomit X 10, lethargy and hemodynamic instability. They have adopted the recommendations from the CDC: Managing Acute Gastroenteritis Among Children.1 Recommend supportive care using oral replacement therapy for mild-moderate dehydration but no pharmacologic treatment for vomiting. “Reliance on pharmacologic agents shifts the therapeutic focus away from appropriate fluid, electrolyte, and nutritional therapy, can result in adverse events, and can add unnecessarily to the economic cost of illness.”1 “ORT is as effective as, if not better than, intravenous fluid therapy for rehydration of moderately dehydrated children and this has been confirmed by two recent meta-analyses.”2 “ORT is associated with significantly fewer major adverse events and a shorter hospital stay compared with intravenous therapy, and is successful in most children. As such, ORT should be the treatment of choice in children with mild or moderate dehydration.”2 Although ORT is successful in over 95% of cases, there are certain contraindications to the use of ORT. These include: Protracted vomiting despite small, frequent feeding. Severe dehydration with a shock-like state. Impaired consciousness. Paralytic ileus and monosaccharide malabsorption. 2 Should anti-emetics be used in the pediatric AGE population? Most anti-emetics in pediatrics are considered to have too many side effects and are not recommended in the pediatric population: Side effects of metoclopermide, prochlorperazine, diphenhydarmine can include significant sedation and extrapyramidal effects.3 “Studies of anti-emetics agents other than ondansetron had small sample sizes, were of low methodological quality and produced inconsistent results. Based on the available literature, antiemetic agents other than ondansetron should not be used for outpatients with gastroenteritis “3 While physiologic pathways leading to emesis are complex and not fully understood, evidence has shown that one pathway entails serotonin release in the stomach and small intestine to trigger the emetic response. Ondansetron is a serotonin 5HT3 receptor antagonist with no dopmaine antagonist activity and therefore it is unlikely to cause extrapyramidal symptoms. Proven safety for kids older than 1 month Easy to administer -iv, oral, disintegrating tablets. If ondansetron is really the only antiemetic for the pediatric population, does it work for pediatric acute gastroenteritis (AGE)? Review of 3 meta-analysis Antiemetics for reducing Vomiting Related To Acute Gastroenteritis in Children and Adolescents(Review)4 Reviewed 3 papers Paper 1Cubeddu LX. Antiemetic activity of ondansetron in Acute Gastroenteritis. Alimentary Pharmacology and Therapeutics, 1997;11;185-915 ▪ Treatment failures (more than 2 episodes of vomiting in 90 minutes within 4 hours of drug admission) ▪ 17% in ondansetron vs. 42% with metoclopermide ▪ 67% ondansetron had diarrhea, 83% in maxeran and 16.7% in placebo Paper 2 Ramsook C. A Randomized clinical trial comparing oral ondansetron with Placebo. Annals Emergency Medicine 2002:39:397-4036 Compared ondansetron vs. placebo in ED for 2 days. Fewer emetic episodes and more did not vomit at all in ED (87% vs. 65% p-0.04). No statistical difference at 48 hours. Fewer admissions and shorter length of hospital stays, but had a higher rate of return visits for either persistent vomiting or persistent diarrhea and higher mean incidence of diarrhea. Paper 3 Oral Ondansetron for Gastroenteritis in a Pediatric Emergency Department, Freedman et al,NEJM 2006;354;1698-7057 Less likely to vomit: 14% vs. 35%, NNT= 5 Vomited less: 0.18 vs. 0.65 Less likely to get IVF: 14% vs. 31%, NNT = 6 Rates of hospitalization and return visits to the ED were the same. “The small number of included trials provided some, abeilt weak and unreliable evidence which appear to favour the use of ondansetron and metoclopermide over the placebo to reduce the number of episodes of vomiting due to gastroenteritis.”4 “The increased incidence of diarrhea noted both ondansetron and metoclopermide was considered to be as a result of retention of fluids and toxins that would otherwise have been eliminated through the process of vomiting.”4 Four RCTs - Cochrane paper plus Reeves et al Ondansetron decreased vomiting ▪ RR: 1.3, 95% confidence interval (CI): 1.2–1.5, ▪ Number needed to treat (NNT): 5, 95% CI: 4–8, This effect was not observed at 24 h ▪ (RR 1.2, 95% CI: 0.9–1.7). Ondansetron significantly reduced the risk of intravenous rehydration. ▪ (RR 0.4, 95% CI: 0.3–0.7, NNT 7, 95% CI: 5–14). No change in rates of hospitalization and return emergency department visits. Despite some clinical benefits, there is insufficient evidence to recommend the routine use of ondansetron. Meta- analysis of 11 studies - looking at different antiemetics including 6 papers on ondansetron in AGE of which 5 were conducted in the ED. Include 2 of the 3 papers from the Cochrane review (removed the Cubeddu paper ) and added 3 more Reeves et al (up to 22 years of age) Roslund et al Stork et al All studies were completed with assistance from the pharmaceutical company who makes ondansetron. They came to some different conclusions…. Cessation of Vomiting: AR 16.9% vs 37.8% (95% CI 0.33 -0.62) NNT was 5 (95%CI, 4-7) Intravenous Fluid Administration: Decrease in IVF 13.9% vs. 33.9% (RR0.41 95%CI= 0.28-0.62) NNT to prevent IVF was 5 (95% CI 4-8) Hospital Admission: Decrease in risk of hospital admission at time of ED visit. 7.5% vs. 14.6% (RR=0.52 CI 0.27-0.95) NNT - 14 children would need to be treated with ondansetron to prevent 1 child from being admitted to the hospital at their visit to ED. (95%CI, 9-44) Return visit: 5 studies 612 patients No difference between the ondansetron and placebo (RR 1.34 95% CI 0.77-2.35) Overall hospital admission rates: 4 studies reported whether children discharged from the ED were admitted during follow-up. The RR of admission at any point during the illness, not just at initial presentation to the ED was not significantly different between either group. Adverse effects: Diarrhea- Most studies found increase in diarrhea within the first 48 hours after administration. No other adverse event was systematically evaluated and no other adverse effects were common across studies, but data was to variable to be pooled to investigate. “Less likely to have ongoing vomiting, to be prescribed IVF and to be admitted to the hospital from the ED.”3 “The symptomatic relief and avoidance of invasive therapies are important outcomes that suggest a benefit of ondansetron treatment in moderately ill children with gastroenteritis”3 “The results cannot be applied reliably to clinicians in other settings and those caring for children with milder disease.”3 “ Although there is currently no evidence that children with mild gastroenteritis benefit from treatment with ondansetron, government agencies and professional societies should strongly consider amending current gastroenteritis treatment guidelines to incorporate the use of ondansetron for certain children with gastroenteritis.”3 Why doesn’t the overall return visits or admission rate decline? “The included studies demonstrate variability in the effect of ondanestron to reduce the risk of hospital admission and the compiled data demonstrate that the ability of single dose ondansetron in the ED to reduces admission wanes across time. “3 “A possible explanation is that the overall clinical course and severity of gastroenteritis are largely determined by the underlying disease or child host and are not necessarily altered by short term relief of symptoms. In addition, an increase in diarrhea due to ondansetron may contribute to later dehydration.”3 Attitude to illness ? Take a pill – everything is better and go home. “Oh no, the vomiting started again or the diarrhea increased. Better go back to the ED.” OR “They really didn’t do anything for me except teach me about ORT and I can do that at home so I won’t go back.” 1. Vomiting from AGE is a distressing symptom for children and parents. I should do something and give them some ondansetron. 2. Pediatric gastroenteritis is most commonly a benign self-limited disease that can be treated with ORT and time. Anti- emetics have a limited role. Side effects: CV: possible prolongation of the QT interval GI: Constipation or diarrhea, abdominal pain CNS: Headache -mild, lightheadedness Hepatic: Transient increases of AST and ALT (not dose or time related) Miscellaneous:- rash, bronchospasm, urticaria, angioedema (rare), blurred vision: associated with infusions of 30 mg in less than 15 minutes Contraindications: -Hypersensitivity to ondansetron 8-15kg = 2mg 15-30 kg =4mg >30 kg =8mg Or 0.15mg -0.3mg/kg/ q8h Ondansetron (generic) – out patient: 4mg tabs po – 10 tabs – $93 8mg tabs po– 10 tabs - $132 Zofran dissolving tabs (not generic) – out patient: 4mg tabs – 10 tabs - $155 8mg tabs – 10 tabs - $235 IV ondansetron (generic) – ACH pharmacy 4mg - $2.30 - $5.25 8mg - $4.58 – 10.50 5 year old boy, previous well with vomiting X 3, diarrhea X 2 in last 24 hours. Clinically looks well with minimal dehydration. 3 yr old female with vomiting X 7 and diarrhea X 8 in last 24 hours who “vomits every time we give her anything”. Mild to moderate dehydration. 18 month old boy with profuse watery diarrhea, greater then 30 times with vomit X 10, lethargy and hemodynamic instability. Safe with few side effects and few contraindications for patients >1 month and older. Effectively reduces ongoing vomiting in pediatric AGE. May reduced IVF and admissions to hospital from the ED. There is not sufficient evidence to recommend the use of ondanestron for pediatric GE in outpatient settings or among children with mild disease. Ondansetron works, but it is easily over utilized. It should never replace teaching parents how to manage ORT. Fewer lines and drugs, more teaching. Severe dehydration – IV saline, ondansetron and admit. Moderate dehydration – Adequate trial of ORT. If failure, then ondansetron and potential for admission/close follow-up. Mild dehydration – education of pediatric AGE, the role of ORT and signs of severe dehydration. ? ??? ?? ? ?? ? ?? ? ? ?? ?? ?? 1. Managing Acute Gastroenteritis Among Children. Oral Rehydration, Maintenance, and Nutritional Therapy . MMWR Recommendations and Reports November 21, 2003 / 52(RR16);1-16 2. Oral rehydration therapy and early refeeding in the management of childhood gastroenteritis. Nutrition Committee, Canadian Paediatric Society (CPS).Paediatr Child Health 2006;11(8):527-31 3. Use of Antiemetic Agents in Acute Gastroenteritis. Decamp L,Arch Pediatr Adolesc Med 2008;163(9):858-865 4. Antiemetics For Reducing Vomiting Related to Acute Gastroenteritis in Children and Adolescents. (Review) Alhashimi D,Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD005506. DOI: 10.1002/14651858.CD005506.pub3. 5. Cubeddu LX, Trujillo LM, Talmaciu I; et al. Antiemetic activity of ondansetron in acute gastroenteritis. Aliment Pharmacol Ther. 1997;11(1):185-191. 6. Ramsook C, Sahagun-Carreon I, Kozinetz CA, Moro-Sutherland D. A randomized clinical trial comparing oral ondansetron with placebo in children with vomiting from acute gastroenteritis. Ann Emerg Med. 2002;39(4):397-403. 7. Freedman SB, Adler M, Seshadri R, Powell EC. Oral ondansetron for gastroenteritis in a pediatric emergency department. N Engl J Med. 2006;354(16):1698-1705. 8. Szajewska H, Gieruszczak-Bialek D, Dylag M. Meta-analysis: ondansetron for vomiting in acute gastroenteritis in children. Aliment Pharmacol Ther. 2007;25(4):393-400. Stork CM, Brown KM, Reilly TH, Secreti L, Brown LH. Emergency department treatment of viral gastritis using intravenous ondansetron or dexamethasone in children. Acad Emerg Med. 2006;13(10):1027-1033. Reeves JJ, Shannon MW, Fleisher GR. Ondansetron decreases vomiting associated with acute gastroenteritis: a randomized, controlled trial. Pediatrics. 2002;109(4) Roslund G, Hepps TS, McQuillen KK. The role of oral ondansetron in children with vomiting as a result of acute gastritis/gastroenteritis who have failed oral rehydration therapy: a randomized controlled trial Ann Emerg Med. doi:10.1016/j.annemergmed.2007.09.010