Drug interaction
advertisement

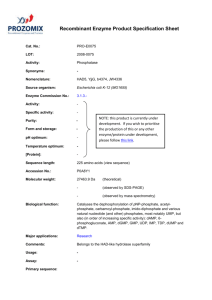
INTERAKSI OBAT Drug interaction Drug interaction can be defined as the modifications of the effects of one drug by the prior or concomitant of another drug (poly-pharmacy) 6.5% of adverse drug reactions in USA were attributed to drug interactions (0.2% of these patients may have life-treatening interactions) The potential drug interactions has been observed to be 17% in surgical patients, 22% in patients in medical wards, 23% in out patients clinics. Increasing risk of death 1 in 10 7 1 in 10 6 5 1 in 10 4 1 in 10 1 in 103 2 1 in 10 Lightning Plane crash Murder Auto-cash Fatal, unexpected drug reaction Drug-Drug interaction may alter drug effect by Additive effect : 1 + 1 =2 Synergistic effect : 1 +1 > 2 Potentiation effect : 1 + 0 =2 Antagonism : 1-1 = 0 Mechanism of drug interaction Pharmacokinetic interactions – – – – Absorption Distribution Biotransformation*** Excretion Pharmacodynamic interactions – – – – Receptor interaction Receptor sensitivity Neurotransmitter release/Drug transportation Electrolyte balance Physiological interactions Pharmaceutical interactions Drug metabolism interaction Enzyme inducers : increase metabolism of concomitant drug therefor increase drug elimination and decrease drug effect Barbiturate, Rifampin, Phenytoin Enzyme inhibitors : decresae metabolism of concomitant drug therefor decrease drug excretion and increase drug effect Cimetidine, Ketoconazole, Erythromycin, Clarithromycin, Chloramphenicol, Quinidine, Sulphaphenazole Pharmacodynamic interactions Receptor interaction – Competitive – Non-competitive Sensitivity of receptor – Number of receptor – Affinity of receptor Alter neurotransmitter release /drug transportation Alter water/electrolyte balance Digoxin (0.25 mg) ½ tab od pc Furosemide (20 mg) 1 tab po od pc Answer Increase digitalis effect due to diuretic induce hypokalemia therefor increase sensitivity of myocardium to digitalis Physiological interactions Drug A and Drug B bind to different receptors on the same tissue but give opposite or similar effect Aspirin (anti-platelet) +Warfarin/Coumarin (anticoagulant) Increase bleeding Pharmaceutical interactions Chemical or physiological interactions – Vitamin C + amphotericin B – Pennicilin + Vitamin C Drug-Food interactions Grapefruit juice and Terfenadine Grapefruit juice and cyclosporin Grapefruit juice and felodipine Grapefruit contains : furanocoumarin compounds that can selectively inhibit CYP3A4 Drug-Herb interactions Ginko biloba St. John’s wort: CYP3A4 inducer Drug features associated with potential interactions Narrow therapeutic index : – Phenytoin – Cyclosporine – Theophylline Sharp response curve: – Phenytoin – Aminoglycoside – Vancomycin Dose dependent (Michaelis-Menten) kinetic –Phenytoin List of drug the most common interacting drug •Antacids •Cimetidine •Digoxin •Warfarin •Theophylline •Ketoconazole Problem in medical practice same complaints same finding same diagnosis same treatment but differential effect ???? •Possible reasons • Physiological factors • Pathological factors • Food •Drug interaction •Genetic Pharmacogenetics Pharmacogenomics Pharmacology + Genetics/Genomics • The study of how individual’s genetic inheritance affects the body’s response to drugs (efficacy & toxicity) • The use of genetic content of humans for drug discovery Drug tablet Sources of drug variability Release Pharmacokinetics Drug in gut Absorption Drug in blood Distribution Drug metabolites Pharmacodynamics Desired response Drug in tissues Drug in urine/bile Drug at receptor No response Unwanted response Genetic variations in drug response and drug toxicity may result from •Variation in drug metabolizing enzymes • Cytochromes P450 •Variation in drug transporters • P-glycoprotien • Thiopurine S-methyltransferase •Variation in drug targets • Beta2-adrenergic receptor • ACE • Dopamine receptor • Variation in disease modifying genes • Apolipoprotein (APOE) DNA polymorphism Changes in the DNA sequence such as – Nucleotide mutation • The most frequent DNA variation found in the human genome is single nucleotide polymorphism (SNP) – Nucleotide deletion – Nucleotide insertion – Gene deletion – Gene duplication Plasma drug concentration Need to keep concentration of drug within the therapeutic range MTC MEC Time Common genetic polymorphism of human drug metabolizing enzymes Enzyme PM incidence CYP2D6 Caucasians 5-10% Asians 1% CYP2C19 CYP2C9 Thiopurine Smethyltransferase Caucasians 2-5% Asians 7-23% Caucasians < 1% Caucasians & Asians 0.3% Drug substrates Dextromethrophan beta-blockers Antiarrythmics Antidepressants Neuroleptics Mephenytoin Mephobarbital Hexobarbital Diazepam Omeprazole Lansoprasole Tolbutamide (S)-Warfarin Phenytoin NSAIDs Azathioprine 6-Mercaptopurine 6-Thioguanine •A 9-yr old boy was prescribed Prozac (Fluoxetine) to help control emotional outbursts. •Child died suddenly ; toxicology tests show massive overdose of fluoxetine •Adoptive parents investigated for homicide. •Psychiatrist notices unusually high levels of Prozac indicatiing CYP2D6 deficiency. •Subsequent genetic testing showed that child had CYP2D6 gene defect “After Michael died, we found out that there were tests to spot enzyme deficiencies that can cause adverse drug reactions. I felt devastated when I heard that. It should be the norm that the tests are used whenever there are concerns about possible side effects." Morphine Codeine O-demethylation CYP2D6 CYP2D6 PM fail to generate active metabolite No analgesic effect Life-threatening complication after cough suppression therapy with codeine •62 yr man with pneumonia treated with codeine (25 mg tid) for cough •4 days after drug administration , the pt’s consciousness rapidly deteriorated, and he became unresponsive. •At the time of the pt’s coma, • plasma morphine was 80 μg/L (normal 1-4 μg/L) • morphine-3-glucuronide was 580 μg/L (normal 8-70 μg/L) • morphine-6-glucuronide was 136 μg/L (normal 1-13 μg/L ) • CYP2D6 genotyping : ultra rapid metabolism N Engl J Med 2004;351:2827-31 Overactive metabolism can cause adverse events “Normal” Activity Morphine Pro-Drug (Codeine) Enzyme Morphine Morphine Pro-Drug (Codeine) Enzyme Morphine Enzyme Morphine Enzyme Morphine “Ultra-rapid” Activity Thiopurine S-methyltransferase (TPMT) polymorphism Cytosolic phase II enzyme involved in the metabolism of thiopurine and thioguanine anticancer drugs Azathioprine 6-Mercaptopurine 6-Thioguanine exhibits genetic polymorphism Common TPMT alleles TPMT*1 wild type Active enzyme TPMT*2 Inactive enzyme G238C (Ala 80Pro) TPMT*3A Inactive enzyme TPMT*3B G460A (Ala154Thr) A719G (Tyr 240 Cys) Inactive enzyme TPMT*3C Inactive enzyme G460A (Ala154Thr) A719G (Tyr 240 Cys) Azathioprine 6-Thiouric acid XO 6-Mercaptopurine HGPRT Thioguanine nucleotides (TGN) Inhibit DNA & RNA synthesis TPMT 6-Methylmercaptopurine • TPMT is the only detoxifying enzyme of 6-MP in hematopoietic cells • TPMT deficiency lead to hematopoietic toxicity Hematopoietic toxicity of azathioprine in a renal transplant patient carried heterozygous TPMT*3C 14 400 White blood count Platelet count 300 10 GI hemorrhage Opportunistic Infection 8 6 200 100 4 Azathioprine treatment 100 mg/day 2 0 0 0 2 4 6 8 10 12 14 16 18 Days after transplantation Tassaneeyakul et al. Transplantation; 76: 265-266, 2003 20 22 24 Platelet count (109/L) 9 White blood count (10 /L) 12 Discovery of Herceptin for treatment of breast cancer •Beast tumors that are Her2 over expressing •Metastasis faster •Poorly response to chemotherapy and poor prognosis •Approximately 30% of breast cancer are Her2 positive •Her2 receptor plays important role in normal cell growth by signaling the cell to divide and multiply Herceptin TM - Anti-HER2 antibody - Breast cancer patients with poor prognosis : over expression of HER2 - Anti-HER2 antibody bind to HER2 and inhibit HER2 function : slowing tumor growth Prior to prescription of Herceptin, the patient need to be diagnosed whether there is an over expression of HER2 Cost : About 28,000 bths/wk, In clinical trials, the median time on Herceptin was 36 wks, total cost 1,000,000 bths Fluorescence in situ hybridization Immunohistochemical chromogenic in situ hybridization US-FDA Labeling Regulations If evidence is available to support the safety and effectiveness of the drug only in selected subgroup of the larger population with a disease, the labeling shall describe the evidence and identify specific tests needed for selection and monitoring of patients who need the drug -21 CFR 201.57 6-Mercaptopurine Labeling Information for Patients Atomoxetine (Stratterra R) product information Information for Patients AmpliChip CYP450 Test Use for routine diagnosis of CYP2C9 and CYP2D6 gene Targeted prescription of medicine: applied pharmacogenomics Today empirical prescription “One drug fit all” Drug A Drug B Drug D Future Rational prescription “individualized” Patient genetic’s profiles Drug A Drug B Drug C Drug C Individual physician experience Cost: time, money & well-being Drug D Informed physician diagnosis Saving : time, money & patient’s life Base on your genetic profile you should take Drug A instead of Drug B