Chemical Dependency
advertisement

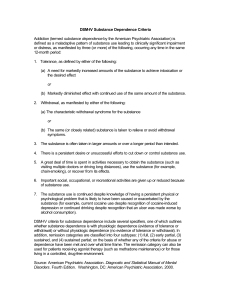
Disease Entities Alcoholism: A Prototype Disease Alcohol Dependence can be viewed as a prototype of chemical (substance) use and dependence. E.M. Jellinek, pioneer of the disease model, identified phases of abuse-to-dependence Jellinek’s Four Phases The individual with alcoholism progresses through these phases. The characteristics of the phases can assist clients, families and health care providers in understanding 1) the loss of control and 2) ethical deterioration characteristic of individuals with chronic chemical dependency (regardless of the chemical of choice). View chart of these phases at: http://www.in.gov/judiciary/ijlap/docs/jellinek.pdf Phase I: Pre-alcoholic Phase Chemical used to relieve stress Tolerance develops Phase II: Early Alcoholic Phase Begins with the first blackout The chemical is no longer associated with pleasure or relief The individual requires the chemical The individual is increasingly secretive; becomes preoccupied with chemical use and maintenance of supply Individual is increasingly reliant upon the defense mechanisms of denial and rationalization Use is associated with guilt and shame Phase III: Middle or Crucial Phase Individual demonstrates signs and symptoms of Physiological and Psychological dependence Binge use often occurs Interactions are characterized by anger and aggression Family dysfunction Individual demonstrates impairment in social and occupational functioning Phase IV: Late or Chronic Phase The individual is almost always intoxicated Ethical deterioration is apparent Impaired reality testing, especially paranoia, is evident Depression with suicidal ideation is common Life-threatening physical consequences are evident: Peripheral neuritis with LE numbness, pain Alcoholic myopathy Wernicke-Korsakoff syndrome Alcoholic cardiopathy Phase IV: Late or Chronic Phase, cont. Hepatitis Cirrhosis (complications include portal hypertension, ascites, esophageal varices and hepatic encephalopathy) Esophagitis and gastritis (ulcers, hemorrhage) Pancreatitis Leukopenia Thrombocytopenia Sexual dysfunction Substance Profiles ALCOHOL DEPENDENCE: Some Facts 5-7% of Americans are Alcoholics Every alcoholic touches lives of 5 people A leading cause of death: from medical complications, accidents and suicides Fetal alcohol syndrome most common cause of mental retardation in children Potentiates other CNS depressants Alcoholism underreported in women and older adults Alcohol: Intoxication Metabolism of alcohol is increased in heavy drinkers Women more easily intoxicated than men. Effects: CNS depression and Peripheral vasodilation Decreased muscle tension, lowered anxiety level, disinhibition, impaired judgment, sedation Toxic effects: stupor, unconsciousness (including blackouts), coma, death Alcohol Withdrawal Usually develops 4-12 hours after cessation or reduction of alcohol use Rebound phenomenon (CNS irritability) as drug effects wear off: increased anxiety, tension, psychomotor activity sweats, tremors, tachycardia, increased temp. and BP nausea, vomiting, diarrhea Alcohol Withdrawal, cont’d Withdrawal seizures may occur 7-48 hours after cessation or reduction Alcohol withdrawal delirium (also known as Delirium Tremens or DTs) may occur 48-72 hours following cessation or reduction- agitation, terror, hallucinations (A Belgian beer is named for this effect) Use of validated withdrawal assessment rating scale assists in objective description of withdrawal severity Validated withdrawal assessment scale: Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) Alcohol: Interventions Seizure precautions; anticonvulsants for DT’s Suicide assessment and precautions, if necessary Medications: for withdrawal Benzodiazepines e.g. chlordiazepoxide (Librium), oxazepam (Serax), diazepam (Valium). Administration may depend on withdrawal rating parameters. Medications to promote abstinence after detox. disulfiram (Antabuse) = Aversive Therapy; produces unpleasant or even harmful effects when alcohol is consumed or absorbed in any form (in foods, fluids, cosmetics, medications, etc.). naltrexone (ReVia) – opiate receptor antagonist-blocks the “high” acamprosate (Campral) – reduces cravings SEDATIVES, HYPNOTICS AND ANXIOLYTICS BARBITURATES BENZODIAZEPINES • Are CNS depressants • Commonly prescribed for sleep, anxiety, muscle spasms, etc. • Also used illicitly, including • reducing effects of amphetamine abuse • if other narcotics not available • by sexual predators Sedative, Hypnotic, or Anxiolytic Abuse and Dependence Potentiate each other and alcohol Produce physiological dependence Produce psychological dependence Cross-tolerance and cross-dependence between CNS depressants Withdrawal sx.: anxiety, insomnia, nausea, seizures Overdose and Fatal effects: respiratory depression, coma, death Interventions for Sedative W/D Quiet, calm environment Monitor vital signs Taper dose gradually; may take weeks or months Seizure precautions INHALANTS: Abuse and Dependence Generally act as CNS depressants Dangerous due to inability to control amount inhaled Use is associated with CNS damage Respiratory irritation, distress and depression GI distress Mouth ulcers Renal and hepatic damage Death from asphyxiation or suffocation OPIOIDS OPIUM and HEROIN MORPHINE CODEINE SYNTHETIC MORPHINE DERIVATIVES, e.g: OXYCODONE (OxyContin) HYDROMORPHONE ((Dilaudid) HYDROCODONE (Vicodin) MEPERIDINE (Demerol) OPIOID Abuse and Dependence Activate endorphins, reduce pain and anxiety Many routes of use: po, subcut., IM, IV, inhaled IV use is associated with infection, including HIV and Hepatitis, bacterial endocarditis, and abscesses May be prescribed or illicitly obtained Heroin--highest abuse and dependence potential CNS effects, including respiratory depression GI effects Opioid Intoxication Initial euphoria Followed by apathy, dysphoria, psychomotor agitation or retardation, impaired judgment Pupillary constriction Drowsiness (“nodding”), slurred speech Impaired memory and concentration Opioid Overdose Pinpoint pupils Clammy skin Respiratory depression Coma (pupils will dilate secondary to anoxia) Death rapidly follows coma Narcotic antagonist used to reverse overdose: naloxone (Narcan) Opioid Withdrawal Symptoms very uncomfortable but rarely dangerous: • Dysphoria, anxiety, cravings • Sweating and chills • Lacrimation, rhinorrhea • GI distress (anorexia, n/v, cramping, diarrhea) • Muscle aches, bone pain • Restlessness • Tremors • Sleep disturbances • Yawning Treatment for Opioid Withdrawal Primarily supportive care Treat symptomatically Specific pharmacotherapy: clonidine-for n/v/diarrhea buprenorphine (Buprenex) –reduces pain and discomfort Example of clinical assessment tool for opiate withdrawal (COWS) Opioid Dependence: Interventions Promoting Abstinence Maintenance Pharmacotherapy to reduce cravings and block the “high” : naltrexone (Trexan, ReVia) methadone –requires enrollment in maintenance program (federally controlled supervision) CNS STIMULANTS: Abuse and Dependence Cocaine Amphetamines: prescribed or illicit Non-amphetamine stimulants Caffeine Nicotine STIMULANTS: Cocaine Intoxication and Dependence Cocaine –Blocks dopamine reuptake esp. in nucleus accumbens (pleasure center) IV or intranasal route; Crack (dilute) form is smoked Rapid Effects and Rapidly metabolized: Intense euphoria Increased mental alertness Increased motor and cardiac activity Increased muscle strength Psychological dependence is even more severe than physical dependence; cravings are intense Amphetamines: Intoxication and Dependence Often are prescribed, widely abused Methamphetamine: Slower metabolic effects, often mixed with cocaine (cheaper) Routes: IV, intranasal, po, smoked Immediate intense pleasure, lasting high “Crash” occurs as drug effects wear off Intense cravings promote frequent, repetitive use Neglect of nutrition and dental care STIMULANTS: Complications Toxic effects: Hallucinations and paranoid delusions Severe hypertension, cardiac ischemia Withdrawal: severe agitation, anxiety, depression Death from cardiac arrhythmias, seizures, suicide, respiratory collapse, stroke Treatment of Overdose: Induce vomiting, diuretics, administer IM antipsychotic for druginduced psychosis/agitation (There are no medications that can treat stimulant dependence) Comparison Chart