Blunt Chest Tension Pneumothorax
advertisement

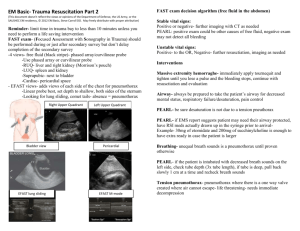
TENSION PNEUMOTHORAX Luke R. Scalcione, MS III Scott Q. Nguyen, M.D. Celia M. Divino, M.D. Mount Sinai School of Medicine Mrs. Greenwich 47 y/o female pedestrian struck is brought to the ER by EMS c/o SOB and Chest Pain History What other points of the history do you want to know? History, Mrs. Greenwich A-M-P-L-E TRAUMA HISTORY Allergies: NKDA Medications: • • • • 1- Sulfasalazine 500 mg bid 2- Methotrexate 7.5 mg qweek 3- Hydroxychloroquine 300 mg daily 4- Prednisolone 10 mg daily PMH: • RA (Dx: 1999) currently treated w/ DMARD therapy Last Meal: 1800 Events Surrounding Injury: • • • Time of injury: 2100 Mechanism of injury: Pedestrian struck crossing intersection of busy street. Pedestrian struck on right aspect of body. Patient rolled over hood of taxi and fell to ground. Estimated taxi velocity: 10 mph decelerating Characterization of Symptoms: Chest pain worsening on inspiration w/ localized thorax tenderness over ribs 6-7, visible right thorax abrasions, non radiating pain, dyspnea Temporal sequence • Abrupt onset SOB (3 minutes s/p accident). What is your Differential Diagnosis? Differential Diagnosis Based on History and Presentation Pneumothorax Musculoskeletal Pain Rib Fractures MI Acute Pulmonary Embolism Physical Examination What would you look for? Physical Examination, Mrs. Greenwich Vital Signs: Tc= 98.7 BP= 98/60 HR=115 RR= 26 Sat 89% RA PRIMARY SURVEY: • AIRWAY: − − − − No altered mental status No airway obstruction noted No maxillofacial fractures noted Gag reflex intact • BREATHING: − Tachypnea; RR=26 − Decreased breath sounds and hyper resonance over the entire R lung field − tracheal deviation to the L of midline − poor respiratory excursion − no flail movement of chest wall − local tenderness over R flank at ribs 6-7 − chest wall asymmetry − notable JVD 8cm above the sternal angle • CIRCULATION: ‾ No obvious signs of gross ‾ ‾ ‾ hemorrhage Hypotensive; BP= 98/60; MAP= 72.67 (1/3 systolic + 2/3 diastolic) Tachycardia; HR=115 cold/moist extremities w/ decreased pulse pressure capillary refill >5 sec ‾ SECONDARY SURVEY: • NOT ASSESSED AT THIS TIME – IMMEDIATE INTERVENTION NECESSARY Would you like to revise your Differential Diagnosis? Revised Differential Tension Pneumothorax Rib Fractures Laboratory What would you obtain? Laboratory NO LAB STUDIES AT THIS TIME IMMEDIATE INTERVENTION NECESSARY See Discussion Section for expected labs Interventions at this point? Interventions at this point Supplemental O2 Decompression Needle Thoracostomy Needle Thoracostomy, Discussion Procedure 1. 2. 3. 4. 5. 6. 7. Use a large bore needle w/ catheter (14-16 gauge) Identify 2nd intercostal space at midclavicular line (1-2 cm lateral to the sternal angle). This will minimize likelihood of IMA injury Prepare area with Betadine Insert needle directly superior to the 3rd rib. This prevents injury to neurovascular bundle located on the inferior aspect of each rib. Insert needle perpendicular to the chest wall, approximately 3-6 cm in depth Stop advancement of needle upon hearing opening hiss/pressure release of pleural space. Remove needle; leave catheter in place What next? What next? Tube Thoracostomy 1. 2. 3. 4. 5. 6. 7. 8. Identify and prepare the area w/ Betadine at ICS 4 or 5 along the mid-axillary or anterior axillary line Anesthetize the area (subcutaneous tissue, intercostal muscles) with Lidocaine. Some physicians use opioid analgesia or a combination of an opioid + Benzo. Make a 2 cm incision Insert a large blunt clamp over superior aspect of rib (preventing damage to the neurovascular bundle that lies on the inferior border of the rib). Apply gentle pressure until the parietal pleura is pierced. Open clamp to establish a tract for the chest tube. Bluntly dissect w/ finger. Clamp proximal end of tube tangentially w/ Clamp. Insert tube over superior aspect of rib into pleural space. Insert the chest tube past the last hole. Note the last hole disrupts the continuity of the radiopaque line—this facilitates radiographic placement confirmation. Suture chest tube w/ Silk sutures. What next? What next? Portable Chest X-Ray (confirm chest tube placement) Management All patient’s with tension pneumothorax must be admitted to an inpatient service. What should be done next? Management Monitor patient continuously with arterial O2 saturation— watch for sudden desaturations F/U CXR may be ordered to assess re-expansion of lung and resolution of pneumothorax. Important: re-expansion pulmonary edema may occur with rapid lung re-expansion s/p tube thoracostomy. This is a potential life threatening situation which can lead to cardiovascular collapse. Keep chest tube on water seal. Chest tube may be removed when indication for placing it has resolved. F/U CXR must be ordered immediately s/p chest tube removal and 24 hrs postremoval to assess for presence of a reoccurring pneumothorax. Discussion Etiology of Tension Pneumothorax Trauma (blunt or penetrating): disruption of the parietal or visceral pleura. Fractures: most prevalent as a result of rib fractures, however also seen in displaced thoracic spine fractures. Barotrauma: ventilator dependent patients on large volume PEEP may rupture peripheral alveoli sacs secondarily disrupting the visceral pleura. Index of suspicion is raised when larger peak airway pressures are needed to achieve a specific tidal volume. Iatrogenic: secondary to trauma induced by Bronchoscopy Chest compressions during CPR Central venous catheter placement Conversion of Simple Pneumothorax -> Tension Pneumothorax Discussion Pathophysiology of Simple Pneumothorax Air enters the pleural space during inspiration. The pleural space increases in volume thus compressing the ipsilateral lung. The ipsilateral lung collapses. During expiration intrathoracic pressure increases, the diaphragm relaxes, and air is pushed out of the pleural space. Note mediastinal structures remain relatively fixed. Discussion Pathophysiology of Tension Pneumothorax Disruption of the lung parenchyma or parietal pleura acts like a one way valve. During inspiration air is drawn into the pleural space. During expiration the tissue flap/valve prevents air from escaping. Subsequent inspirations additively draw more air into the pleural space. Increasing intrapleural pressures result in collapse of ipsilateral lung and deviation of mediastinal structures contralaterally Discussion Complications: Cardiovascular Collapse: the implications of a tension pneumothorax are profound. Displacement of mediastinal structures contralaterally causes kinking of the SVC and IVC. Venous return to the heart is severely compromised resulting in decreased cardiac output. Shock and hypoperfusion ensue. Lab Results, Mrs. Greenwich If Lab Tests were ordered at presentation the following are expected: ABG: 7.32/50/60/24/ 89 % RA 138 102 18 Chem 7 Cardiac Enzymes: 110 3.7 25 TnI: 0 TnT: 0 CKMB: 1.2 1.2 Lab Results, Discussion ABGs: Often seen in tension pneumothorax is a varying degree of acidemia, hypercarbia, and hypoxia. Note in acute respiratory acidosis increases in PaCO2 by 10mmHg will decrease pH by 0.08 (i.e. PaCO2 40->50 lowers pH 7.4>7.32). The reduction in PaO2 is caused by alveolar hypoperfusion secondary to atelectasis, low ventilation/perfusion ratios, and anatomic shunts. Chem 7: Principally used for the CO2 value. More accurate for calculations of compensated respiratory acidosis than HCO3- values in ABGs which represents an average of computed PaCO2 levels. Cardiac Enzymes: necessary to r/o acute MI and resulting cardiogenic shock, must have serial reading to accurately r/o acute MI Discussion If CXR was ordered at presentation the following are expected: Tension Pneumothorax Left Subpulmonic Pneumothorax Right SQ AIR Pulmonary Contusion Deep Chest Tube Persistant Subpulmonic Pneumothorax May not see mediastinal shift if pneumothorax is bilateral! Discussion Do not delay treatment of a Tension Pneumothorax. CXR can be taken for confirmatory measures after decompression needle thoracostomy or tube thoracostomy. The diagnosis of a Tension pneumothorax is made clinically when one has a high index of suspicion. Findings on CXR: Large radiodense lung field Absent lung markings on ipsilateral side Contralateral deviation of trachea and mediastinal structures If tension pneumothorax involves left lung the left hemidiaphragm may be depressed/flattened. The liver prevents this radiographic finding on the right side QUESTIONS ?????? Summary Tension Peumothorax is a life threatening condition which may quickly lead to cardiovascular collapse and shock. Immediate intervention must be initiated if there is a high clinical suspicion of a tension pneumothorax. Intervention includes decompression needle thoracostomy followed by chest tube thoracostomy, followed by a portable chest x-ray to confirm tube placement and re-expansion of collapsed lung fields. Laboratory and diagnostics may confirm the diagnosis of a tension pneumothorax (i.e. ABG, CXR) however the diagnosis lies predominantly on clinical presenting symptoms. References Check out these sites • Needle Thoracostomy photo courtesy of http://www.biodigital.org/voz2/slide8.htm • Tube Thoracostomy photos courtesy of http://www.vesalius.com • CXR w/ 2 Chest Tubes photo courtesy of http://www.trauma.org/imagebank/chest/images/chest0037.html • Pathophysiology of Pneumothorax photos courtesy of http://home.ewha.ac.kr/~chestsg/dong/poster/99/2.htm • CXR of tension pneumothorax courtesy of http://www.emedicine.com/med/topic2793.htm Acknowledgment The preceding educational materials were made available through the ASSOCIATION FOR SURGICAL EDUCATION In order to improve our educational materials we welcome your comments/ suggestions at: feedbackPPTM@surgicaleducation.com