A Prairie Encounter with Analbuminemia
advertisement

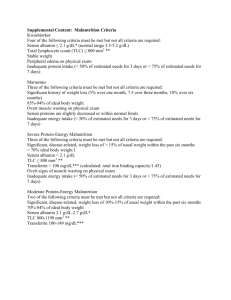
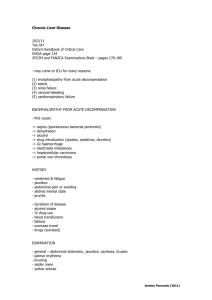
Life without Albumin Encounters with Analbuminemia Andrew W. Lyon, PhD FCACB, DABCC. Department of Pathology and Laboratory Medicine, University of Calgary & Calgary Laboratory Services Boras, Sweden. May 2007 Objectives: Review the pathophysiology of serum albumin Review clinical laboratory methods of albumin determination Describe Analbuminemia and four cases found in Saskatoon Depict how common laboratory method of serum albumin measurement confound the diagnosis of analbuminemia. The History of ‘albumin’ 400 Hippocrates: Foam on urine with renal failure. 1500 Paracelus: precipitated protein from urine with acid 1894 Kander: Crystallized horse albumin 1896 Starling: Suggests role of albumen in maintaining circulation. 1926 Svedberg: Measures mass by ultracentrifugation 1937 Tiselius: Separated serum by electrophoresis 1947 Klotz: Studies how dyes bind to albumin 1950 Peters: Biosynthesis of albumin in liver slices 1954 Benhold: First report of analbuminemia, 2 cases. 1957 Knedel: Report of the genetic cause of bisalbuminemia The History of ‘albumin’ 1970 1975 1979 1981 1986 King: Studied tryptic fragments of albumin Brown / Meloun: Amino acid sequence BSA & HAS Sargent: Isolated the HAS gene Lawn: Genetic sequence of HAS cDNA Dugaiczyk: Complete HAS gene sequence Mutation studies Crystallization studies Parenteral albumin utilization studies Physiological Roles of Albumin Circulatory Role……….80% oncontic pressure Transport of metabolites Sequestration of toxins… delivery to the liver Bilirubin, calcium, fatty acids, bile acids, drugs Low affinity reservoir for thyroxine, vitamin D Bilirubin, carcinogens. Metabolic Effects: enhances lipoprotein lipase Miscellaneous Effects: limits fibrin fiber thickness Clinical Utility of Serum Albumin Levels Assess protein malnutrition Renal disease… nephrotic syndrome G.I. pathology Liver disease… impaired synthesis Hypoalbuminemia, intestinal edema, diarrhea Methods of albumin quantification Turbidometry: following acid or salt precipitation Dye-binding methods Protein-error of pH indicating dyes Protein electrophoresis Immunoassay Dye-binding Methods High pH causes a colour change: High pH Dye-H Dye- + H+ Add albumin at Constant pH Albumin Dye-H Dye--Albumin Applications: Urine dipstick, routine clinical chemistry. Dye-binding Methods Urine Dipsticks: Urine Protein detection Largely measures urine albumin False positive colour at high pH Poor detection of Bence Jones proteins/ light chains … as they don’t bind the dyes. Serum Albumin Bromcresol Green , Bromcresol Purple Short incubation times to improve specificity Serum Protein Electrophoresis Albumin (65%) Globulins (35%) o o o o o o o Transthyretin / Prealbumin Antitrypsin, Acid Glycoprotein Haptoglobin, Macroglobulin, Transferrin, C3 Lipoproteins (VLDL, LDL, HDL) Missing: “Fibrinogen” Immunoglobulins ( IgG, IgA, IgM, IgD, IgE) LIVER From: Immunofixation. Killingsworth & Warren Calgary Laboratory Services Serum Protein Electrophoresis Bisalbuminemia Not particularly rare in Canada! Often seen in aboriginal peoples > 50 known Albumin mutations. Bisalbuminemia results from two copies of different albumin genes, resulting in different charges. Albumin Immunoassay Method usually reserved for urine or CSF albumin determination: “microalbumin” Various immunoassay methods: rate nephelometry, nephelometry, turbidometry, radial immunodiffusion. Objectives: Review the pathophysiology of serum albumin Review clinical laboratory methods of albumin determination Describe Analbuminemia and four cases found in Saskatoon, SK, Canada. Depict how common laboratory method of serum albumin measurement confound the diagnosis of analbuminemia. Our first case… Paul Meinert (pediatric resident) complains “why are serum albumin levels in your lab fluctuating so much?” “What do you mean by fluctuating?” Variable levels of serum albumin over 6 months, (7 month old infant) 18 Method_1 Method_2 Method_3 16 14 12 g/L <10 10 8 6 4 2 0 a b c d e f g Impact of low albumin?? Bilirubin-Alb Fatty Acids - Alb Adipose Tissue T4 - Alb Calcium - Alb Alb for Oncotic Pressure, to avoid edema Patient #1 Admitted to NICU as a newborn for hypoglycemia and perinatal asphyxia, mild tubular necrosis & brain edema. Low serum albumin noted: 17 g/L Normal 24 hr urine protein level. Three admissions during first 6 months related to respiratory distress and wheezing. Nutritional status: Good. Gaining weight, growing, apparently normal liver function. Patient #1 At 6 months of age, still no explanation for the low serum albumin (13 – 18 g/L, routine chem). Serum albumin was still lower by electrophoresis (3-5 g/L). Tc99-labelled albumin scan: negative for protein loosing enteropathy. Clinical Biochemistry consult to review the results. Analbuminemia Albumin (Dye-binding) : 10 – 17 g/L Albumin (electrophoresis): 2 – 3 g/L Albumin (Immunoassay) : <0.01 g/L Consistent with: Analbuminemia A genetic lack of albumin What is analbuminemia and what is the prognosis ? Why did our routine laboratory methods detect 17g/L of albumin is there was NONE? Analbuminemia Serum albumin test results: very low. Apparently a benign, recessive inherited disorder: elevated lipids and globulins, 30% have lipodystrophy below waist, 30% mild ankle edema, low capillary blood pressure. VERY RARE (approx. 42 reported cases) Lipodystrophy in Analbuminemia Patient #1 continued Paul Meinert and I met with the staff pediatric GI specialist in Saskatoon: Garth Bruce. “ I thought it was analbuminemia. I saw another child like this a few years ago.” Analbuminemia Patient #2 Admitted at 2 days of age with cellulitis Admitted 3 times during the first 6 months for respiratory distress / infection. Mild hyperbilirubinemia, mild ALP elevation and low serum albumin: 10 – 15 g/L. Nutritional status, weight gain & growth were normal. Albumin by electrophoresis: 2 g/L Patient #3 Admitted at 6 weeks of age with tetany and prolonged diarrhea. Infant had low serum calcium and magnesium levels. Tetany resolved on magnesium administration. Low albumin levels were detected < 10 g/L i.v. albumin was administered prior to conducting serum electrophoresis. Analbuminemia A genetic lack of albumin Why did our routine laboratory methods detect 17g/L of albumin is there was NONE? Re-evaluation of Dye-binding Serum Albumin Methods Roche Diagnostics: BCG method (rapid) Ortho Diagnostics: BCG method (slow) BCG: bromcresol green Linearity of albumin methods with diluted serum (constant albumin : globulin ratio) Linearity of albumin methods with 100% human IgG or 100% human albumin. Comparison of serum albumin methods with diluted serum Observed Albumin g/L 30 25 Roche 20 Ortho 15 10 5 0 0 10 20 30 Target Serum Albumin g/L 40 70 Roche Serum Albumin g/L Ortho Serum Albumin g/L Assay response to pure human Albumin 60 50 Ortho 40 30 20 10 0 0 20 40 60 100% Human Albumin g/L 80 70 60 50 Roche 40 30 20 10 0 0 20 40 60 100% Human Albumin g/L 80 12 Roche Serum Albumin g/L Ortho Serum Albumin g/L Assay response to pure human Ig G Ortho 10 8 6 4 2 0 0 20 40 100% Human Ig G g/L 60 1 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 Roche 0 20 40 100% Human Ig G g/L 60 Why did our assays report the presence of albumin in patients with analbuminemia ? Ortho Diagnostics Assay: Reacts with globulins Gives a positive result in the absence of albumin. The assay did not report that albumin was below the reportable limit. Roche Diagnostics Assay: Assay reported < 10 g/L in analbuminemia Assay had no globulin interference. Serum Protein Electrophoresis Baseline disturbances during densitometry lead to reports of 2-3 g/L albumin. Our three patients with analbuminemia all appeared to have albumin present, according to the dyebinding albumin methods. What was the serum albumin concentration reported in the reported cases of analbuminemia? It depends on the albumin methods that were used 28 Cases of Analbuminemia: Levels of Albumin ‘detected’ A: Dye-binding methods B: Salt Precipitation method C: Protein Electrophoresis D: Albumin Immunoassay Awkward conclusions: Clinicians should consider a diagnosis of analbuminemia (a genetic lack of albumin) even when the clinical laboratory detects serum albumin up to 17 g/L. Albumin immunoassays and serum protein electrophoreses are capable of detecting analbuminemia, but routine serum albumin assays are NOT. Patient #3 Diagnosis following i.v. albumin infusion. Establish a partnership with Monica Galliano and Lorenzo Minchiotti, Univ. Pavia. Isolation of genomic DNA 14 exons were amplified by PCR Single-strand conformation polymorphism (SSCP) and heteroduplex analysis. Sequencing Exon #3 SSCP 1 Control 2 Mother 3 Patient 4 Control 5 Analb Codogno Exon #3 Heteroduplex Analysis 6 Control 7 Mother 8 Patient 9 Control 10 Analb. Codogno ‘ ‘ ‘ ‘ A: Control B: Patient AT deletion “Kayseri albumin” ‘ ‘ ‘AT’ deletion frameshift results in a stop condon and analbuminemia. Three cases of analbuminemia…. Was this a coincidence? Dr. David Meyer, Dept Anthropology, Univ. Saskatchewan, Doctoral Thesis: Red Earth Crees 1860 – 1960 Ethnogeographic and historical work Near-complete pedigrees 1860 – 1970 Study of the Deme Deme: a marriage isolate or universe Red Earth and Shoal Lake reservations had a common and stable deme 1860 – 1960. Evacuation Photo: April 2007 Red Earth Reserve Evacutation of Red Earth Reserve, April 2007 Red Earth and Shoal Lake Population Date Population 1781 -1782 In group marriage 1850 0 smallpox epidemic 6 men 1870 – 1900 187 60% 1900 – 1930 220 85% 1930 – 1960 391 85% 2007 1500 ? 1971 Third Generation 75 Couples (married, widows/widowers). 8 marriages between first cousins. 23 marriages between second cousins. 35 marriages between relatives, > 2nd cousin. 9 insufficient to establish kinship. There is likely a ‘founder effect’ responsible for the local incidence of analbuminemia at the Red Earth and Shoal Lake reserves. Future Investigations?? September 2003: Patient #4 •29 year old native female from Red Earth, SK – referred because of lower limb edema. •History of presenting illness: –admitted to Nipawin hospital for pneumonia (July 2002) and right calf cellulitis –upon discharge the patient noticed that her legs were swollen –the family doctors consult note from June 2002 implies she has had a low albumin, large legs and lower extremities and an abnormal body habitus And so the story continues… Life without Albumin Acknowledgments Garth Bruce, Paul Meinert, Robin Casey, Pat Blakely: Pediatrics, Jill Newstead, Sharon Card: Medicine. Univ. Saskatchewan. Mark Salkie, Victor Laxdal Pathology, Univ. Saskatchewan. David Meyer, Anthropology, Univ. Saskatchewan. Lorenzo Minchiotti, Monica Galliano & Lab, Univ. Pavia. References Lyon AW, Meinert P, Bruce GA, Laxdal VA, Salkie ML. Influence of methodology on the detection and diagnosis of congenital analbuminemia. Clin. Chem. 1998; 44: 2365-7. Galliano M, Campagnoli M, Rossi A, Wirsing von Konig CH, Lyon AW, Cefle K, Yildiz A, Palanduz S, Ozturk S, Minchiotti L. Molecular diagnosis of analbuminemia: a novel mutation identified in two Amerindian and two Turkish families. Clin Chem. 2002 ;48:844-9. Newstead J, Card S, Lyon AW. Low serum albumin and abnormal body shape in a young Canadian First Nations woman. Lab Med Volume 35, Number 6 / June 2004. For more details on analbuminemia, visit the Albumin Website: http://www.albumin.org