Document 10149480
advertisement

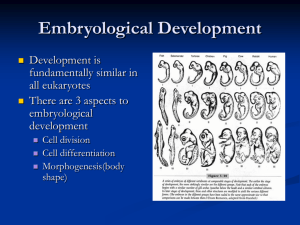
Lecture 3 ESS_2nd semester Embryology - definition, the object and significance of embryology Phases of the human ontogeny Gametes - their structure, physiology and origin (gametogenesis). Differences between spermatogenesis and oogenesis Transportation of gametes. Sperm capacitation and acrosome reaction Fertilization and cleavage, the morula and blastocyst Implantation development of plant as well as animal organisms begins when an ovum is fertilized and ends at the moment of the death of individual the time period from fertilization to death is called as the ontogeny (also as life cycle) in placental mammals, including the human, ontogeny divides 2 periods of different length: prenatal period (prenatal development) - from fertilization of an ovum to delivery of fetus postnatal period (postnatal development) - from the delivery to death of the individual in mammals, goal of embryology consists first of all in study and description of events occuring during the prenatal period (phase) of development similar goals and orientation has also medical embryology: to describe and explain events and processes from the fertilization to the birth of the human Significance of embryology the basic theoretical medical branch good knowledge of embryology is important in many medical disciplines: anatomy - knowledge of the human development helps to understand complicated relationships between many organs of the human body embryology shows more closely relationships and bounds to anatomy than to histology (reasons for teaching of embryology together with histology are rather practical then logical as study of the pre-embryonic and early embryonic stages needs to use and studied only with the use of histological slides) pathology - knowledge of embryology is explored namely in study of restorative (healing) processes and in description and classification of neoplasms (tumours) obstetrics, pediatrics and surgery - knowledge of normal development is essential to understanding the mechanisms, symptomatology and correction of congenital malformations a special medical line -prenatal medicine- was constituted in last years, it deals with diagnosis, treatment and prevention of congenital malformations Phases of prenatal development in the human pre-embryonic phase involves the first 3 weeks from fertilization of the ovum several well-defined stages are distinguished : - zygote (fertilized ovum) = the cell standing at the beginning of development of a human being; there is a result of a fusion of the male and female sex cells or gametes - morula (from latin morus – mulberry) = the solid ball consisting of 12 to 16 blastomeres blastomeres = cells that result in process of cleavage of the zygote, blastomeres are genetic equal and they do not substantially differ each other, prospective properties or developmental potency of blastomeres are the same, each of them can give rise to a new individuum - blastocyst = the stage with a cavity inside that is filled with fluid, 2 different cell populations differentiate at the first time in development: trophoblast cells + inner cell mass or embryoblast cells, during the day 5 - gastrula = the bilaminar pre-embryonic stage, in which the main body axis and polarity begin to become apparent, the bilaminar stage develops on day 7 and lasts to the end of the second week after fertilization embryonic phase lasts from the beginning of the 4th week to the end of the 8th week in the phase anlages of the all body organs are constituted by the end of it, the embryo is recognizable human in appearance and measures cca 2-3 cm from head to tail fetal phase it lasts from the 9 week to delivery of fetus; during the fetal phase, development of organs rapidly continue, some of them enter their function, the fetus grows quickly in length and increases its weight gain, in particular during the terminal months Phases of the postnatal development in the human infancy – from the birth to the end of the first year of the age (the first two weeks of infancy are called as the newborn or neonatal period) childhood - from 13 month until 12 to 13 years; the primary teeth appear and are replaced by the secondary or permanent teeth puberty - is the period between 12-15 years in girls and 13-16 years in boys, during which secondary sexual characteristics develop adolescence - follows the puberty and ends 3-4 years after it; the organism reaches sexual but also physical, mental and emotional maturity adulthood - a period in which developmental changes occur very slowly and are mostly characterized by selective loss of highly specialized cells and tissues postnatal development of the human is studied and treated with various medical branches Structure and origin of gametes gametes = generative (germ or sex) cells in comparison with somatic cells, gametes are highly specialized and contain only half the usual number of chromosomes the sperm or spermatozoon (the male germ cell) the ovum or egg cell (the female germ cell) human gametes similar to gametes of another species substantially differ each other in size, structure, motility, and viability The sperm, spermatozoon is a motile cell that is cca 60 m long a head, a neck (connecting piece) and a tail the head has a flattened pyriform shape , approximately 4 m in length, consists of the sperm plasma membrane, condensed nucleus and acrosomal cap covering the anterior two-thirds of the nucleus the acrosomal cap derives from the Golgi apparatus and contains hydrolytic enzymes (hyaluronidase, acrosin, neuraminidase) the neck (= connecting piece) is very short sperm section composed of segmented columns, proximal centriole, and a part of distal centriole that serves as basal body of the axoneme of tail the tail - cca 55 m in length middle piece – about 5 to 9 m in length, 1-2 m in diameter, consists of the axoneme that is inserted in the distal centriole located in the neck, is surrounded by 9 outer dense fibers (dense columns) and externally to them by a mitochondrial sheath principal piece - 40-45 m in length is narrower than the middle piece contains the axoneme, 9 outer dense fibers and fibrous sheath end piece cca 5-10 m in length, consists of the axoneme and associated cytoplasm only the neck and all pieces of the tail are covered with a membrane that is continuous with the plasma membrane of the head the semen (ejaculate) viscid fluid expelled from the urethra during the orgasm volume of one ejaculate is 3 - 6 ml it consists of the seminal plasma = secretions of accessory sex glands (seminal vesicles and prostate) formed elements: spermatozoa, exfoliated epithelial cells form genital and urinary passages, lymfocytes, prostatic concretions average sperm density 60 - 100 million/ml - normospermy (density lesser than 20 million/ml = infertility) average sperm velocity is 2 - 3 mm/min under alkaline pH spermatozoa retain ability to fertilize ovum not longer than 16 to 24 hours The ovum a large spherical nonmotile cell with diameter of over 100 m (130-150 m) eccentrically located large and pale nucleus with a well-developed nucleolus numerous free ribosomes and smaller mitochondria with arch-like oriented cristae voluminous Golgi apparatus located near the nucleus, lately near the cell surface few endoplasmic reticulum absence of centrioles cortical granules under cell membrane, contain material of mucopolysaccharide character (presence of granules is the sign of maturation of an ovum) during the sperm penetration into ovum, the content of cortical granules is released and prevents the polyspermia = basis of the cortical reaction yolk = cell inclusions chemically, yolk involves saccharides, especially of glycogen, lipids and proteins that mostly occur in the form of proteinaceous lattices amount of the yolk in human ova is low (oligolecithal ovum) is diffusely scattered throuhout the ooplasm (isolecithal ovum) greek lekithos =yolk surface of the ovum is limited by the cell membrane, from which short microvilli project into the zona pellucida the zona pellucida is a clear envelope 10 to 12 m thick it is composed of highly sulfated mucoproteins perivitelline space= space between the cell membrane and zona pellucida zona pellucida Gametogenesis process of formation and development of sex cells the aim is to prepare sex cells to their assimilation or fusion that is a basis of fertilization during gametogenesis, the chromosome number is reduced by half and shape of cells is altered Reduction of the chromosome number is achieved by special type of cell division called meiosis; there are two successive meiotic divisions: the first meiotic division: homologous chromosomes pair during prophase and separate during anaphase, with one representative of each pair going to the respective pole; by the end of the first meiotic division, each new cell formed contains the haploid chromosome number, i.e. half the original number of chromosomes of proceeding cell (homologous chromosomes go well together and two always form a "matched pair" whose members are derived from each parents) - the reduction division; disjunction of paired homologous chromosomes is the physical basis of segregation (the separation) of allelic genes. the second meiotic division: follows immediately the first division without DNA replication and without a normal interphase, each chromosome divides in two chromatids that are then drawn to opposite poles, the haploid number of chromosomes is retained, and daughter cells formed during the second division really contain reduced chromosome number, with one representative of every chromosome pair. Spermatogenesis = maturation process of male gametes; includes the series of events leading to transformation of spermatogonia into haploid spermatids; these then develop into ripe (mature) sperms by gradual process known as spermiogenesis (= histological differentiation of spermatids) 3 phases: spermatocytogenesis meiosis spermiogenesis the site where spermatozoa undergo their development and maturation are seminiferous tubules of the testis development from the spermatogonium to fully differentiated spermatozoon lasts 64 –74 days in avarrage spermatocytogenesis meiosis spermiogenesis spermiogenesis Oogenesis = maturation process of female gametes is bound to the ovary (ovarian cortex) - ovarian follicles 2 phases: oocytogenesis meiosis oocytogenesis - mitotic division of oogonia - begins during the fetal period the oogonia enlarge to form primary oocytes, they enter the first meiotic division that is stopped in the prophase, the cell nucleus is then transformed into the interphase form in which is to stay to the beginning of reproductive life of females meiosis the first meiotic division is completed shortly before the ovulation - the primary oocyte divides unequal and gives rise to large secondary oocyte and the first polar body (polar body is nonfunctional and soon degenerates) in time of ovulation the secondary oocyte enters the second meiotic division that progresses only to metaphase, in which division is arrested completion of the second meiotic division is closely connected with penetration of the sperm into the oocyte: the division becomes again to continue and developed daughter cells are the mature ovum and the secondary polar body Comparison of spermatogenesis and ogenesis number of produced gametes – 4 spermatids vs 1 ovum (polar bodies are nonfunctional cells that degenerate) course of process – continuous vs cyclic and limited only on period of sexual maturity (400 ova) motility of gametes – motile with only small amount of the cytoplasm vs immotile, the cytoplasm is abundat and contains stored material for the first week of development Transportation of gametes the site of fertilisation is the uterine tube – its dilated part termed the ampula nearly to the ovary Oocyte transport: to release the secondary oocyte from the graaphian follicle occurs during the ovulation the oocyte surrounded by some granulosa cells is expelled from the follicle and is directed via stream of follicular fluid under contraction of fimbriae (finger-like processes of the tube) into the lumen of the infudibulum the oocyte then passes into the ampulla by waves of peristalsis of muscle cells in the wall of oviduct it is supposed that oocyte reaches the fertilization site in cca 25 min Sperm transport: after cohabitation, the spermatozoa deposited against the cervix and the posterior fornix of the vagina, pass by movements of their tails through the cervical canal into the uterus and subsequently in the respective uterine tube the ascent is caused by contractions of smooth muscle cells in the wall of the uterus and uterine tube fresh spermatozoa, upon arrival in the female genital tract, are not capable to fertilize the oocyte because they must undergo capacitation and the acrosome reaction Capacitation of sperm an activation process of sperms that takes about 7 hours during this process, a glycoprotein coat and seminal plasma proteins are removed from the plasma membrane over the acrosome the process does not connect with morphological aterations spermatozoa undergo their capacitation in the uterus or uterine tube by influence of substances secreted by these parts Important: sperms must be capacitated also in cases of in vitro fertilization (as capacitation media are used gamma-globulin, free serum, serum dialysate, follicular fluid, albumin, dextran etc. - artifitial capacitation media) The acrosome reaction it follows the capacitation involves a series of events that are induced by penetration of spermatozoa through the corona radiata in comparison with capacitation, the process is accompanied by structural alterations - by multiple point fusions of plasma membrane and the outer acrosomal membrane the fused membranes then rupture to produce multiple perforations through them enzymes contained within the acrosome escape (hyaluronidase, trypsin-like substance, acrosin) Fertilization is a process of fusion of male and female gametes in average, it needs several hours ( 24 hours) fertilization site - the ampulla of the uterine tube - is the widest segment of the tube germ cell viability – spermatozoa can stay alive in the female reproductive tract for 24 hours (there is suggestive evidence that some sperms may fertilize an ovum for as long as three days after insemination) if the ovum (the secondary oocyte) was not fertilized, it degenerates 12 to 24 hours after ovulation phases of fertilization: penetration of corona radiata penetration of zona pellucida fusion of oocyte and sperm cell membranes constitution of the male pronucleus fusion of the pronuclei 1. Penetration of corona radiata the corona radiata is envelope from follicular cells that encloses the ovulated oocyte the main goal of this phase is dispersal of corona radiata cells by enzyme hyaluronidase released from the acrosomal caps of spermatozoa 2. Penetration of zona pellucida is facilitated by the action of enzymes released from the acrosome primary role plays acrosin, enzyme causes lysis of the zone (inhibition of acrosin prevents passage of sperms through the zona pellucida) once the first sperm passes through the zona pellucida, so-called a zona reaction starts, during which the zona pellucida becomes impermeable to further spermatozoa is supposed that the zona reaction is mediated by cortical granules of the secondary oocyte 3. Fusion of oocyte-sperm cell membranes this phase is characterised by actual fusion of the oocyte membrane and membrane covering the posterior region of the sperm head, the head and tail of the sperm enter the cytoplasm of the oocyte after fusion of membranes, the secondary oocyte can complete the second meiotic division to give rise to the mature ovum with haploid number of chromosomes and the second polar body chromosomes in the egg nucleus decondense to form the female pronucleus 4. Constitution of the male pronucleus the penetrated sperm moves in close vicinity to the female pronucleus its nucleus becomes rapidly swollen and forms the male pronucleus (the tail of the sperm degenerates) 5. Fusion of the pronuclei the male and female pronuclei approach each other in the centre of the ovum and come into contact they lose then their nuclear membranes and maternal and paternal chromosomes intermingle (mix together) and they organize in an equatorial plane the first mitotic division of the zygote starts /cleavage of the zygote/ Results of fertilization: restoration of diploid number of chromosomes (half from the mother and half from the father) determination of the sex of the new individual (XX -female, XY-male) initiation of cleavage (not fertilized oocyte degenerates in 12-24 hours after ovulation) Cleavage of the zygote the phase of development characterized by mitotic divisions of the zygote resulting in formation of the blastocyst cells are called blastomeres and become smaller with each division the cleavage takes place partly in the uterine tube (during the first three days), partly in the uterus (from day 4 to 6) the first division resulting in 2-cell stage needs about 24 to 30 hours, subsequent divisions follow in shorter intervals because blastomeres become progressively smaller TEM: SEM: after the eight-cell stage (three mitotic divisions), the morula stage develops the morula - a solid ball consisting of 12 to 16 cells that lay on tightly each other (it shows resemblance to the fruit of mulberry tree) the morula enters the uterine cavity where is transformed into the blastocyst Formation of the blastocyst shortly after the morula enters the uterus (on day 4), fluid passes from the uterine cavity through the zona pellucida to form a single fluid-filled space – blastocystic cavity (primitive chorionic cavity or blastocoele) Consequently, the morula cells separate into two cell lines: an outer cell layer, the trophoblast (greek trophé = nutrition) - gives rise to chorion and finally fetal part of the placenta a group of centrally located cells, called as the inner cell mass or embryoblast - gives rise to the embryo the blastocyst is enclosed with the zona pellucida and lies free in the uterus cavity during the day 6, the zona pellucida becomes to digest by enzymes contained in the uterine fluid and soon disappears the denuded blastocyst then expands up to diameter of 400 m or more and is prepared to start the implantation Early blastocyst (with the zona) Late (mature) blastocyst (denuded) Implantation an adaptive process, during which the blastocyst establishes very close contact with the uterine mucosa (endometrium) of the maternal organism main goal is to provide nutrition of the embryoblast because yolk material has been completely utilized during cleavage and blastocyst formation the implantation begins on day 7 and ends on day 13 the trophoblast cells play key role in this proces, they differentiate in the cytotrophoblast and the syncytiotrophoblast invading the uterine mucosa Staging of the implantation: Attaching of the blastocyst to the endometrial epithelium Invasion of the trophoblast cells in the endometrium Reparation of implantation defect in endometrium Formation of uteroplacental circulation Manifestation of decidual reaction 1. Attaching of the blastocyst to the endometrial epithelium – it follows the zona pellucida lysis; the blastocyst attaches to the endometrium with embryonic pole (the pole, by which the embryoblast is placed) 2. Invasion of the trophoblast cells in the endometrium follows as a result of contact of trophoblast with the endometrium trophoblast cells proliferate and differentiate into 2 populations: the syncytiotrophoblast located peripherally – invades and erodes quickly the endometrial stroma and uterine glands it forms around the blastocyst a large, thick and multinucleated mass without obvious cell boundaries the erosion of the uterine mucosa is caused by proteolytic enzymes produced by syncytiotrophoblast cells the cytotrophoblast (secondary trophoblast) that gradually replaces the original trophoblast the cytotrophoblast cells are mitotic active and form new cell generations - migrate into the blastocyst cavity where give rise to the extraembryonic mesoderm or migrate externally to complete masses of the syncytiotrophoblast the trophoblast cell differentiation of the entire blastocyst needs about 3 days, i.e. on day 10 a conceptus is usually embedded within the endometrial stroma 3. Reparation of implantation defect in endometrium after penetration of the blastocyst, the defect in the epithelium is filled with a closing plug (operculum) – a blood clot and cellular debris by day 12, the site of implanted conceptus appears as a minute elevation of the endometrial surface and is covered with regenerated epithelium 4. Formation of uteroplacental circulation around day 9, isolated spaces (cavities) called lacunae are formed in the syncytiotrophoblast they become filled with nutrition secretions from eroded endometrial glands and with maternal blood from ruptured maternal capillaries – histiotroph later, between day 11 and 13, adjacent lacunae fuse to form lacunar network in which maternal vessels open and through which maternal blood flows 5. Manifestation of decidual reaction the conceptus evokes reaction of the entire endometrium consists in endometrial stromal cell changes that enlarge and accumulate glycogen and lipid droplets, in vascular alterations (capillary network around the conceptus becomes denser), and glandular alterations – uterine glands increase their activity changes are referred to as the decidual reaction and the decidual transformed endometrium to as the decidua The decidua involves 4 distinct regions as follows: basal decidua - under the conceptus marginal decidua - at the side of the conceptus capsular decidua - above the conceptus parietal decidua - has no contact with the conceptus Implantation sites of the blastocyst Intrauterine sites: normally, the blastocyst implants on the posterior wall of the midportion of the uterus body important: nidation near the internal ostium – the developing placenta covers the internal ostium as placenta previa it causes severe bleeding during pregnancy (it usually occurs in the 28th week) or during the labor Extrauterine sites: if blastocyst achieves the mature blastocyst stage (without zona pellucida), it starts to implant in the site where is just - implantation in the uterine tube (ectopic tubal pregnancy) - is represents about 90 % ectopic pregnancies; tubal pregnancy usually results in rupture of the uterine tube and hemorrhage during the first 8 weeks, followed by death of the embryo - implantation in the ovary (ectopic ovarian pregnancy) ectopic pregnancies are connected with profuse hemorrhage