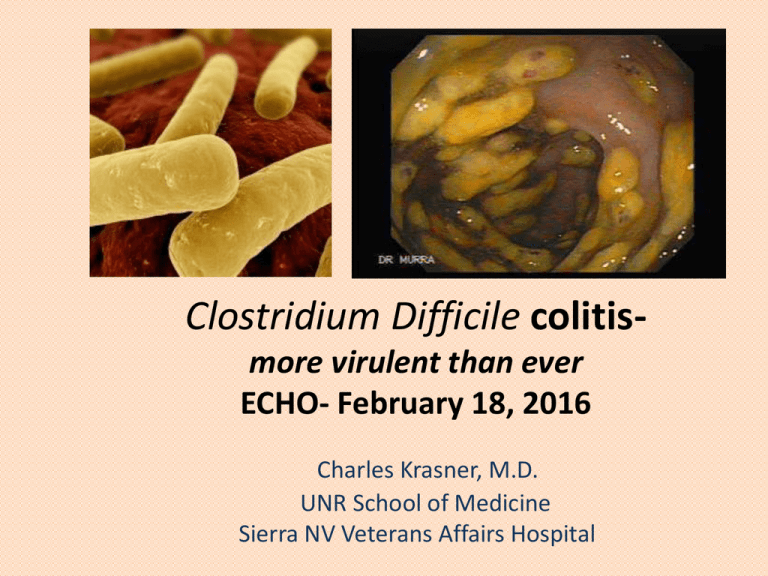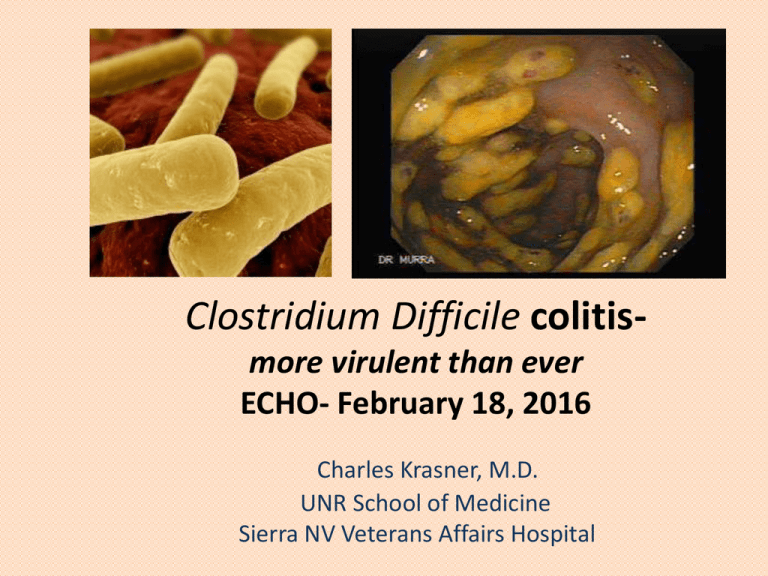
Clostridium Difficile colitismore virulent than ever
ECHO- February 18, 2016
Charles Krasner, M.D.
UNR School of Medicine
Sierra NV Veterans Affairs Hospital
Growing problem of pseudomembranous colitis
• MMWR- “…incidence, deaths, and excess health care
costs are at historic highs” +/- 1 billion dollars/yr
• 3x increase in decade- now 500,000 infections and
29,000 deaths per year. More deaths than even MRSA
infections.
• #1 cause of increase- over use of antibiotics
• #2 cause – appearance of a more virulent C.diff strain
associated with risk of greater mortality
• #3 cause- increased relapse rate – 20% of cases have
at least one relapse- difficult to treat
• #4 cause- overdiagnosis???
Asymptomatic C. diff Carriers
•
•
•
60% of stool carriers in one study also
had it on their skin and their surrounding
environment
Spores on the skin of these carriers were
easily transferred to others
Non-poopers are important sources of
potential infection to others- everyone
should wash with soap and water!
Hospitals started seeing very severe cases of
C.diff colitis with high mortality
The C. difficile had now become resistant to common
antibiotics and flourished in the hospital
NAP-1 C. diff strain- nasty super bug now seen
throughout Nevada and USA.
• Approx. 1/2 of all cases in NV are NAP-1 positive!!!
• resistant to common antibiotics overused in hospital,
particularly fluoroquinolones
• A genetic mutation allows 10 to 20x more toxin A and B
to be secreted, plus it has its own unique binary toxin
• More likely to progress to fulminant disease and death
• Increased rate of spore germination to active disease
increases likelihood of relapse
• If your micro lab does a PCR test , they are already
testing for NAP-1, but you may need to request results
C. Diff Lab Diagnosis
• Direct culture- not used - $$$/slow turn around time
• ELISA- Is the C. diff producing toxin? – detect toxin A
+/- toxin B. Detects the toxin, but misses some cases –
about 70% sensitive. Is that important?
• C. diff PCR- positive test tells you C. difficile carrying
the toxin gene is present in the stool. 100% sensitive,
but DOES NOT differentiate between asymptomatic
carriers and toxin producers. Do not order as a test of
cure!
From: Overdiagnosis of Clostridium difficile Infection in the Molecular Test Era
JAMA Intern Med. 2015;175(11):1792-1801. doi:10.1001/jamainternmed.2015.4114
Figure Legend:
Kaplan-Meier Curves of Time to Resolution of Diarrhea by Clostridium difficile Test GroupThe median duration of diarrhea for
patients with at least 1 day was 3 days (interquartile range, 1-6 days) for Tox+/PCR+ (121 of 131), 2 days (interquartile range, 1-4
days) for Tox−/PCR+, and 2 days (interquartile range, 1-3 days) for Tox−/PCR− (927 of 1123) (P < .001). Log-rank P values are
P < .001 for all groups, P = .003 for Tox+/PCR+ vs Tox−/PCR+, (143 of 162) P < .001 for Tox+/PCR+ vs Tox−/PCR−, and P < .001
for Tox−/PCR+ vs Tox−/PCR−. Tox+/PCR+ indicates
C difficile
immunoassay
Copyright
© 2016toxin
American
Medical positive and polymerase chain reaction positive;
Date
of download:
2/17/2016
Tox−/PCR+,
C difficile
toxin immunoassay negative
and
polymerase
chain
reaction positive; Tox−/PCR−, C difficile toxin
Association. All rights reserved.
immunoassay negative and polymerase chain reaction negative.
Are we over-diagnosing C. diff infection?
• Careful patient selection is vital
• Up to 50% of tested patients don’t have significant
diarrhea
• Up to 40% are on a laxative regimen when tested
• The PCR test may be 100% sensitive, but only a 45%
positive predictive value for CDI
• There is no difference in length of diarrhea or
mortality in toxin-/PCR+ or toxin -/pcr- patients !
Negative consequences of over-treating CDI
• Contact precautions adversely effect the patient- anxiety,
depression, isolation
• Receive unnecessary antibiotics that can paradoxically
increase risk of actual CDI and select for VRE etc
• Expense of isolation, need for single room
• Adversely effect hospital infection incidence rate
Human beings as ecosystems- not just an individual,
but a collaborative effort between commensal bacteria
and their host
Original Article
Duodenal Infusion of Donor Feces for Recurrent
Clostridium difficile
Els van Nood, M.D., Anne Vrieze, M.D., Max Nieuwdorp, M.D., Ph.D.,
Susana Fuentes, Ph.D., Erwin G. Zoetendal, Ph.D., Willem M. de Vos, Ph.D.,
Caroline E. Visser, M.D., Ph.D., Ed J. Kuijper, M.D., Ph.D., Joep F.W.M.
Bartelsman, M.D., Jan G.P. Tijssen, Ph.D., Peter Speelman, M.D., Ph.D.,
Marcel G.W. Dijkgraaf, Ph.D., and Josbert J. Keller, M.D., Ph.D.
N Engl J Med
Volume 368(5):407-415
January 31, 2013
Rates of Cure without Relapse for Recurrent Clostridium difficile Infection.
van Nood E et al. N Engl J Med 2013;368:407-415.
Some new C. diff Developments
• The Beagle “Sniff” test as a near perfect diagnostic test
• Tigecycline looks to be an effective antibiotic in fulminant
C.diff combined with oral vanco and iv metronidazole
• Enthusiasm for stool transplant, now available in (Jelly Belly
Diarrhea Flavored ?) gelatin capsules!
New surgical approach for fulminant colitis- less
invasive, better mortality
Traditional – total colectomy
Double-barrel ileostomy –
preserves colon, much lower
mortality
Test time!
I. Which fact is incorrect about C. diff?
• Causes 500,000 cases per year
• Severity of illness has increased last few years
• Majority of C. diff cases are community
acquired
• Relapses are major problem with C. diff and
may respond to stool transplant
II. Which of the following is incorrect regarding
medical management of C. diff?
• Oral metronidazole is recommended for mild
C. diff
• Oral vancomycin is preferred for moderate or
severe C.diff
• Patients with fulminant C. diff with ileus
should receive intravenous vancomycin
III. Manifestations of fulminant C. diff include all
the following except:
•
•
•
•
•
•
Severe abd pain and worsening diarrhea
Hypotension requiring vasopressors
Dropping WBCs
Respiratory failure requiring intubation
Elevated lactate levels
Renal failure
IV. Increased virulence of NAP-1 strain is a result of
which of the following ?
• Lower rates of germination
• Higher resistance to anti-fungal agents
• Gene mutation leading to reduced toxin
production
• Ability to produce large amounts of toxin A
and B that overwhelm treatment attempts
V. New approaches to C. diff infection include all
of the following except:
• PCR testing for quicker and more sensitive
diagnosis – but may result in over-treatment
of a carrier state
• Stool transplant for recurrent disease
• Less invasive surgical techniques to improve
outcome and allow for earlier intervention
• Fidaxomicin as an inexpensive and effective
oral therapy for NAP-1 strain infections