Stillbirth: Prevention | Risk assessment, Decreased
advertisement

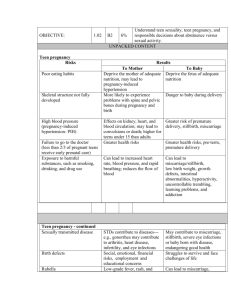
Stillbirth: Prevention Lets talk! Risk assessment Decreased fetal movement Ruth C Fretts MD, MPH Assistant Professor Harvard Medical School HVMA RFetts@vmed.org Objectives Put stillbirth on your radar Learn the risk factors for late stillbirth What are possible strategies for prevention, focus on decreased fetal movement and the risk assessment strategies “HOW COME NO ONE EVEN MENTIONED THE POSSIBILITY OF A STILLBIRTH UNTIL WE HAD ONE! Infant deaths by week of death West Midlands 1997 to 2003 Number of deaths 2500 2000 Early neonatal (N=1729, 58%) 1500 1000 500 Gardosi et al Late neonatal (N=404, 14%) Post neonatal (N=824, 28%) 0 Week 1 Week 4 Week 52 Stillbirths and infant deaths by week of death West Midlands 1997 to 2003 Number of deaths 2500 Stillbirth (N=2256, 43%) 2000 Early neonatal (N=1729, 33%) 1500 1000 500 Late neonatal (N=404, 8%) Post neonatal (N=824, 16%) Gardosi et al 0 Week 1 Week 4 Week 52 Born “Still Forever”Lifelong impact on family Stillbirth is common >1/200 in US Frame this risk against other life changing events Focus on Risk Assessment Management of decreased fetal movement Case 1 33 yr old G2 P0 (sab11 weeks) Japanese women history of infertility but conceived spontaneously Received BCG as a child, neg Chest XR Case 1 Noted at 29w size < dates (SFH 27), “watch for growth” 31 2/7 no complaints (SFH 29) 35 3/7 no complaints (SFH 32), plan US following week, discussed FM NST done because of low baseline, reactive 36 2/7 (SFH 31) US fetal weight 10-25% BPP 8/8 37 5/7 reported decreases FM for 4 days (SFH 33) plan bi weekly NST Case 1 38 1/7 (SFH 33) NST reactive, reviewed kick counting 38 4/7 (SFH 34) NST reactive 39 2/7 Reactive NST (SFH 36) US 9% nl fluid normal doppler 39 4/7 Fetal distress on labor APGAR 0, 0, 3 baby (5 lb 12 oz) 3% for growth, c-section under general Baby had severe hypoxic encephalopathy, seizures (MRI showed severe hypoxic encephalopathy) Case 1 Poor outcome, worsening placental dysfunction not recognized in spite of normal testing (falling off the growth curve) Growth restriction and decreased fetal movement at term- beware that antepartum testing is falsely reassuring Case 43 yr old IVF pregnancy presents at 40 4/7 weeks with decreased FM for 2 days. Advised that the baby had less room to drink a cold drink and if still concerned to make her way to the hospital NST was performed which was reactive Seen at 40 6/7 weeks still reported DFM Returned later that evening no FH. DFM at TERM Out-come based on if the person on call believes that DFM maters No standard protocol Typical NST>Home Missed opportunity to review other potential risks We know multiple consultations is associated with increased risk* LETS TALK… Alex Heazell in press Elliot’ Dad Worried about Down’s, normal nuchal scan, so relieved Comments to Nicki “You don’t look 43!” Noted DFM 40 +3, and 40 +4, NST normal, seen by the midwife, OB gave the “all clear” on the phone, trying to get away Friday evening. 40 6/7 seen Still DFM thought they were being paranoid because the NST was normal, went for a walk around the pond, told to eat something and then return. Returned IUFD, unexplained. Faster Trial your first obstetric visit 1. 2. 3. 4. 5. 6. 7. Triple screen Quad screen NT PAPP-A, free Bets-hCG Integrated NT PAPP-A, free Bets-hCG, plus Quad screen Serum Integrated PAPP-A plus Quad Step wise Sequential Contingent sequential combined first. Faster Trial 38,033 women Cost per Down’s syndrome detected was between $690,427 and $719,675 Ball et al Obstet Gynecol 2007 Management and Perception of Risk Maternal Age at Risk of Delivery Trisomy 21 20 30 35-39 1/1667 1/952 1/378 40+ 1/106 Risk of Any Chromosoma l abnormality 1/526 1/385 1/192 1/66 Hook EB. JAMA 1983:249 and Hook EB. Obstet Gynecol 1981, and adapted from Reddy et al 2006 Am J Obstet Gynecol *data only given for those less than 35. Management and Perception of Risk Maternal Age at Delivery Risk of Trisomy 21 Risk of Any Chromosomal abnormality Risk of Stillbirth after 37 weeks Multipara Risk of Stillbirth after 37 weeks Primipara 20 1/1667 1/526 1/775* 1/269* 30 1/952 1/385 1/775* 1/269* 35-39 1/378 1/192 1/502 1/156 40+ 1/106 1/66 1/304 1/116 Hook EB. JAMA 1983:249 and Hook EB. Obstet Gynecol 1981, and adapted from Reddy et al 2006 Am J Obstet Gynecol *data only given for those less than 35. US Data 2005 CDC AIDS Deaths (all) 12,543 Deaths from Hepatitis 5,529 SIDS 2,230 Infant Deaths due to congenital anomalies Cases of Salmonella related illness to peanut butter Number of fatal listeria cases (7 were in elderly) 5,552 Stillbirths (20+ weeks) 600 9 25,655 Lets Talk The First Step to Prevention Risk Assessment for Stillbirth Overweight / obesity Hytertension Diabetes AMA (35 -39) AMA 40+ Smoking Low education/ socioecon. status Primiparity and multiparity IUGR Macrosomia Reduced fetal movements OR 2 - 3 OR 1.5-4 OR 1.5-3 OR 1.5-2.2 OR 2.4-5.0 OR 2 - 4 OR 2 - 7 OR 2 – 3 OR 3 – 7 OR 2 - 3 OR 4 - 12 Stillbirth Risks: Preterm OR <3rd 7.2 th 3-10 2.0 Non-white Ns AMA Ns >BMI 1.4 Ruptured Ns Uterus PAR 51.9 9.8 Ns Ns 4.4 Ns Froen Gardosi Acta Scan 2004 Term OR 6.4 2.4 2.3 1.5 2.0 8.1 PAR 19.7 11.1 12.8 6.3 9.1 0.4 Stillbirths Non SGA [cust] & Non-SGA [pop]: => OR 1 6.1 5.1 1.2 5.0-7.5 4.3-5.9 0.8-1.9 SGA [cust] SGA [both] SGA [pop] 8887 = 29% 21931 8884 = 29% OR 95% C.I. Diabetic Pregnancies 8 7 6 Weekly Rate of of Fetal Death per 1000 5 4 3 2 1 Rouse et al 1995 0 26 27 28 29 30 31 32 33 34 35 36 37 38 39 Weeks of Gestation Gestational Age and Risk of Unexplained Stillbirth Yudkin et al Lancet 1987 Rate/1000 undelivered 2 1.8 1.6 1.4 1.2 1 0.8 0.6 0.4 0.2 0 other Unexplained 29 31 33 35 37 39 41 Obesity Timing of Stillbirth related To pre-pregnancy obesity Danish National Cohort Aagaard Nohr Obstet Gynecol 2005 Reddy et al AJOG 2006 National Collaborative Perinatal Project: The Risk of Stillbirth by Race Per 1000 Ongoing Pregnancy 20 18 16 14 12 10 8 6 4 2 0 White Black 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 Gestational Age C-Section Rates by Parity and Induction Status BWH and BIDMC Heffner et al 2004 Percent 40 Prim, indu Prim, spon Multip, indu multip, spon 30 20 10 0 36 37 38 39 40 Gestational Age 41 42 NICU cs rate CS rate Tear Low 5min Induction of Labor Compared to Expectant Management in Nulliparous IND 38 39 40 41 15.6% 18.6% 22.5% 29.3% EXP OR 17.6% 19.9% 24.3% 33.1% 1.9 (1.3to2.9) 1.5 (1.1 to 2.1) 1.6 (1.2 to 2.2) 1.3 (1.0 to 1.8) Spont 9.0% 11.6% 15.2% 19.3% .M. Nicholson, L.C. Kellar and G.M. Kellar, The impact of the interaction between increasing gestational age and obstetrical risk on birth outcomes: evidence of a varying optimal time of delivery, J Perinatol 26 (2006), pp. 392–402 Optimal Timing of Delivery Low risk37 1/7 - 41 0/7 HT 39 2/7- 40 1/7 AMA 38 5/7- 39 6/7 model did not work for DM because most of babies were admitted to the NICU to observe glucose levels Hmmmm Until with have randomized controlled trials assessing the risk and benefit of expectant verses active management all we can do is discuss what we know – – – – DFM AMA RACE Obesity Stillbirths Births Stillbirths Rate OR Total 13,133 62 4.6 Reference DFM 476 (Femina) Chart DFM 8 16.9 4.1 (1.8-9.06) 15 29.4 8.0 (4.2-15.3) Femina Cases 1* 2 3 4 5 6 7 8 9 GA 39 5/7 41 3/7 36 6/7 37 4/7 36.5/7 34.0 32 2/7 30 4/7 28 2/7* Wt 2673 4533 2470 2693 3167 1424 1830 1021 1221 % 3% 97% 4% 19% 90% <1% 32% <1% 19% DFM 4+ days 12 hrs 2 days 1 day 12 hrs 2 days 9 hours 17 days 15 days Evaluation COD NST 2d prior Placental* BPP 2d prior Unexp/infection No IUGR No Unexplained No Cord No IUGR/Cord No Cord No IUGR NST 2d prior Unexplained Case 1 APGAR 0, 0, 3 permanent severe disability DFM by Medical Chart Review 10 11 12 13 14 15 16 GA 38 6/7 39 28 30 39 4/7 30 2/7 37 6/7 Wt 3500 4000 510 710 3284 850 3080 % 77% 98% <1% <1% 43% <1% 58% DFM 18 hours 1day 1day 14 days 2 days 3 days 12 hr Eval No No No No BPP 2 wks None None COD Unexp Cord IUGR IUGR Cord IUGR/PET Abruption Gestational Age and Percentile Growth for Stillbirths with a History of DFM Percentile Growth 120 100 80 60 40 20 0 25 27 29 31 33 35 Gestational Age 37 39 41 43 What are the useful tools Norway? ... the peers’ experience of 2,930 cases of DFM ... Tools needed to detect pathology: Test Usage Proved When useful path. NST Ultrasound Doppler 97.5% 3.2% 23.4% 94.0% 11.6% 86.2% 47.3% 1.9% 14.1% Only When finding path. 1.2% 8.7% 0.2% 9.9% 71.3% 1.7% Growth Restriction 44% of the stillbirths were growth restricted (<4%) Normal pregnancy Froen et al N=305 Pregnancy in non-smoking mother, younger than 35 years, with BMI < 25, leading to a vaginal delivery at term of a healthy baby between the 10th and 90th birth weight centile. Mean time to count to ten is 00:09:14. Pregnancy while smoking Froen et al The 2 h ”alarm” occurs in 9.1% of these pregnancies Fewer FM towards term N=33 Pregnancy in smoking women. Mean time to count to ten is 00:12:44. Pregnancy in obesity Froen et al The 2 h ”alarm” occurs in 9.0% of these pregnancies Fewer FM towards term Fewer FM throughout pregnancy N=111 Pregnancy in obese women (BMI > 30). Mean time to count to ten is 00:15:28. Pregnancy ending in emergency Cesarean section The 2 h ”alarm” occurs in 9.9% of these pregnancies Fewer FM throughout pregnancy Fewer FM towards term N=81 Pregnancy leading to delivery by an emergency Cesarean section. Mean time to count to ten is 00:13:37. Pregnancy ending in preterm delivery The 2 h ”alarm” occurs in 13.5% of these pregnancies Specificity 97.6% Fewer FM towards time of delivery N=37 Pregnancy leading to a preterm delivery. Mean time to count to ten is 00:12:32. Undetected IUGR in stillbirths Only between 11- 20 % of pregnancies that end in a stillbirth in a severely growth restricted baby are detected prior to the stillbirth Prevention Early prenatal care Black women and immigrants Screen for congenital anomalies Optimize health, smoking, weight gain Reduce multiples Improve awareness and management of decreased fetal movement Individualize risk assessment late in pregnancy, include race, age, obesity, parity on treating a women when she is “post-dates” Photogram published on AP taken By Erin Fogarty, her husband and Claire after she was stillborn at term.