Fluid - Komion
advertisement

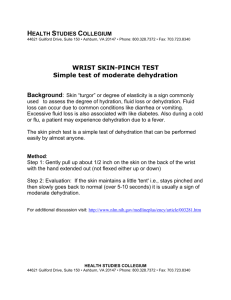
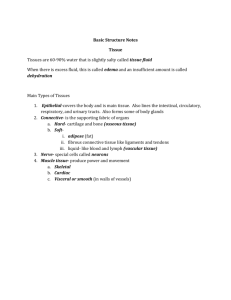
The problem Worldwide, dehydration is probably the most common cause of death in childhood. In the UK, dehydration and iatrogenic overhydration are key issues in clinical practice. A child suffering 10-15% dehydration will die or suffer permanent brain damage unless managed urgently and capably. Why nurses? Nurses administer the fluids Nurses are responsible for ensuring that the fluids given are safe in type and amount Nurses must recognise an unsafe prescription Under and over treatment with fluids (water and or electrolytes) may cause severe morbidity or mortality Fluid content as % of body weight Water contributes to a higher percentage of body weight in child. Fluid balance is relatively more important and fluid imbalance causes more morbidity and mortality Willock J, Jewkes F (). Making sense of fluid balance in children. Paediatric Nursing. 12 (7) 37-42 Body compartments Willock J, Jewkes F (). Making sense of fluid balance in children. Paediatric Nursing. 12 (7) 37-42 Fluid distribution according to age Younger children have a higher proportion of extra-cellular fluid. In some forms of fluid loss, an important volume of fluid can be lost from the extra-cellular (mostly interstitial) compartment. Isotonic fluid is given IV to reach this compartment. Willock J, Jewkes F (). Making sense of fluid balance in children. Paediatric Nursing. 12 (7) 37-42 Fluid distribution Young children have a greater proportion of water in their interstitial compartment Willock J, Jewkes F (). Making sense of fluid balance in children. Paediatric Nursing. 12 (7) 37-42 Osmotic pressure What we put into the vascular compartment affects what is in the other compartments Normally the osmotic pressure in the different body compartments is equal. Differentials in osmotic pressure between two body compartments will cause fluid to move between compartments. This can be a serious problem during the acute phase of treatment. Therefore – electrolytes MUST be monitored during and (especially) after treatment. Blood Volume Neonate 90 ml / kg Infants and children 80 ml / kg Adults 65 ml / kg Willock J, Jewkes F (). Making sense of fluid balance in children. Paediatric Nursing. 12 (7) 37-42 Electrolytes Learn the plasma values for these electrolytes Water What is acquired from: Drinking IV fluids etc. Oxidation of nutrients (carbohydrate) Note that we make our own water Water is lost through Renals Lungs Skin GI Tract Note the avenues of insensible loss Insensible loss Water is normally lost via: Renals (not insensible) Lungs Skin GI Tract Obligatory loss of fluid from the skin etc. Is influenced by: Surface area Environmental temperature Humidity Respiratory rate (lungs) Non obligatory loss controlled by ADH (posterior pituitary). ADH causes the reabsorption of water from the renal collecting ducts. Insensible loss To calculate Body Surface Area Insensible loss is 300ml / M2 / day so use this formula (left) Willock J, Jewkes F (). Making sense of fluid balance in children. Paediatric Nursing. 12 (7) 37-42 Homeostasis Osmo-receptors in the hypothalamus and elsewhere Hypothalamus and posterior pituitary responsible for sensation of thirst (mid hypothalamus) and releases of antidiuretic hormone Volume receptors (baroreceptors) in the atria and elswhere Homeostasis The renal collective ducts re-absorb water The absorption of fluid from the gut is a passive response to the active transport of sodium (failure results in diarrhoea) Normal Oral Fluid (Feed) Requirements Pre-Term Term Adult • Pre-term baby needs approximately 200ml / kg / day • Term babies need approximately 150ml / kg / day • Adults need approximately 70ml / kg / day Normal oral fluid requirements (adapted from Behrman RE (1992)). Age Av. Weight (kg) mL per kg per day 3/7 10/7 3/12 6/12 9/12 1 yr 2 yr 4 yr 6 yr 10 yr 14 yr 18 yr 3.0 3.2 5.4 7.3 8.6 9.5 11.8 16.2 20.0 28.7 45.0 54.0 80-100 125-150 140-160 130-155 125-145 120-135 115-125 100-110 90-100 70-85 50-60 40-50 Subdivision of total fluids Fraction of Total Function Amount Type 1st fifth Insensible loss One fifth Insensible losses only 2nd fifth Essential urine output Two fifths Severe fluid restriction 3rd to 5th fifths Maintenance of urine output Three fifths Moderate fluid restriction Four to five fifths Adequate fluids Six to ten fifths Induced diuresis Maintenance IV requirements First 10kg Second 10kg Each additional kg • 100 ml / kg / day for the first 10kg body weight (4ml / kg / hour) • 50ml / kg / day for the second 10kg body weight (2ml / kg / hour) • 20ml / kg / day for each additional kg body weight (1ml / kg / hour) A 15kg child requires 1000ml plus 250ml =1250ml daily Note that oral fluid requirements are higher than IV requirements. Glasper , McEwing and Richardson (2007). Oxford handbook of children’s and young people’s nursing. Oxford University Press. Types of IV Fluid Fluid losses (children) Willock J, Jewkes F (). Making sense of fluid balance in children. Paediatric Nursing. 12 (7) 37-42 Dehydration a problem because children have: Higher proportion of water Higher metabolic rate (children exchange up to 50% of the body fluid daily (adult 17%) Higher metabolic rate (more water produced and excreted) Higher metabolic rate = greater propensity to dehydration Greater surface area in proportion to weight Greater proportion of extracellular fluid Neonates relative inability to concentrate urine on dehydration: Neonatal Glomerular filtration Rate is 30ml/min/1.73 m2 At 9/12 GFR is 100ml / min / 1.73 m2 Note that circulatory failure (shock) can be highly compensated and so vital signs may mask underlying pathology. Consequently hypotension may be a late sign of hypovolaemia. A child is a small vessel with a large spout An adult is a large vessel with a small spout Therefore – children lose fluid FASTER Dehydration Clinical signs of dehydration Clinical signs Mild (<5%) Severe (>10%) Comments Loss of fluid = loss of weight ? the most important sign of severity Measure it from the beginning Dry mouth Not as obvious in babies, feel inside their cheek Decreased skin turgor Most obvious on abdomen Sunken eyes Ask parents Tachypnoea Late sign Tachycardia Late sign Hypotension Pre terminal sign Only for the experienced Decreased weight Moderate (510%) Drowsiness Decreased urine output Sunken fontanelle Means of estimating clinical dehydration Capillary refill time (should be < 2 seconds) Central – peripheral temperature gap (should be < 2 degrees centigrade) Tissue turgur (abdomen or inside of thigh) 3-5% weight (fluid) loss skin remains raised for seconds Severe malnutrition can cause reduced skin turgur Obesity can cause skin turgur to appear normal Hypernatraemic dehydration associated with firm ‘thick-feeling’ skin Oedema Dry mucosa (inside cheek) Oligurea – Normal urine output is at least 1ml/kg/hour Weight change (1ml water weighs 1 gram). Equation for dehydration Treatment for fluid loss (dehydration) Less than 5% dehydration – treat with Oral rehydration solution (ORS), e.g. dioralyte Treatment of shock – initial Rx Admission to 2 hours post admission Weigh child Estimate degree of dehydration Measure urine output Give 20 ml / kg Normal saline or Colloid over 1-2 hours Repeat if shock not reversed Do electrolyte levels Allow IV potassium only in the presence of adequate renal function. Treatment of shock 2-24 hours Give maintenance fluids plus 2/3 deficit and minus volume already administered (20ml / kg) Example Weight on admission Dehydration estimated at fluid deficit is Deficit X 0.66 is Maintenance requirement Subtract fluid administered Volume required over 22 hours is 9kg 10% 900ml (10% of 9kg) 594ml 900ml (100ml/kg) 180ml (20ml/kg) 1314ml Monitor – be vigilant Lab Serum Values Monitor electrolytes after infusion and at intervals Correct major electrolyte imbalances SLOWLY Monitor systemic perfusion Monitor urine output Monitor neurological status Underhydration is SAFER than overhydration Potassium 3.5-7mmol/l Sodium 136-146mmol/l Types of dehydration Normonatraemic Isotonic pressure of intravascular compartment is the same as that in the extravascular compartment [normal] Hypernatraemic The vascular compartment is hypertonic Hyponatraemic The vascular compartment is hypotonic Na = sodium, aemia = blood, ‘Na’traemic syn. ‘blood sodium’ Normonatraemic dehydration Normonatraemic Most common in UK No significant shift of fluid between intra-cellular and extracellular compartment Normal serum sodium is 130-150mmol/L Hypernatraemic dehydration Relatively uncommon in the UK Serum sodium > 150mmol/L Can be caused by high levels of water loss with retention of sodium or iatrogenically Possible causes include High levels of insensible fluid loss Diabetes incipidus Extra-cellular fluid is well maintained at the expense of intracellular fluid Clinical features underestimate the actual level of dehydration Hyponatraemic dehydration Caused by the loss of fluid high in sodium Fluid passes into the cells Results in convulsions and shock which is more severe than the level of dehydration would indicate Shock – the three stages Compensated shock Uncompensated Irreversible Compensated shock Normal BP Oligurea Pallor, coldness, clamminess Tachycardia Increased capillary refill time Anxious, agitated and confused Uncompensated shock Insufficient oxygenation of tissues Insufficient provision of glucose to tissues Failure of normal metabolism Build up of lactic acid and carbonic acid (acidosis) Reduced cardiac output Platelet aggregation is small blood vessels (bleeding) Increased capillary permeability ( fluid moves from capillaries into interstitial space) Irreversible shock Damage to the renals and brain is such that even if dehydration (hypovolaemia) is corrected and fluid balance is restored, death will still take place Oxygen free radicals are released (or have been released) and have cause irreversible major organ damage