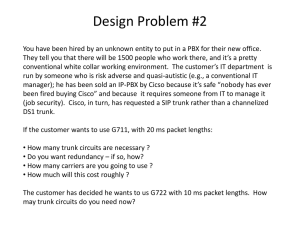
Dermatology Board Review
advertisement

Tiny, whitish-yellow, firm papules Face of neonates Small epithelial-lined cysts Arise from hair follicles Persistent May resolve after months to years Timing Neonates Older children after skin injury Cause: obstruction of eccrine sweat ducts Description: multiple 2-3mm sweat retention vescicles Easily rupture Location Infants: Head, neck, upper trunk Older Children: areas of desquamating sunburn Aka “Prickly Heat” Cause: sweat duct obstruction in deeper layers Results from use of thick lubricants or tight-fitting clothing in hot, humid weather Description: erythematous papulopustular eruption Locationface, upper trunk, intertriginous areas of neck Etiology unknown Course: wax/wanes Crops over hands/feet Resolve over 10-21 days Recur within few wks Resolves by age 3y/o Description Pinpoint erythematous papules Evolve to papulopustules or vesiculopustules Pruritic Treatment Topical steroids Antihistamines (itching) Location Hair-bearing and intertriginous areas “Cradle cap” … infants Scalp, eyebrows, eyelashes, perinasal, presternal, postauricular, neck, axillae, groin May become generalized Description Red, scaling eruption Nonpruritic, mild Pathogenesis Unknown Pityrosporum and Candida Treatment May resolve spontaneously Antifungal cream Low-potency topical steroid Antiseborrheic shampoos Multiple factors Urine and stool Ammonia formation Occlusion by plastic diapers Soaps and detergents Spares intertriginous areas Treatment Frequent changes Gentle cleansing Application of barrier pastes Topical steroids may be helpful Description Bright red eruption, sharp borders, pinpoint satellite papules and pustules Intertriginous areas KOH: Budding yeast and pseudohyphae May have oral thrush Treatment Topical antifungals May require brief course oral treatment Description Thin-walled pustules on erythematous base Larger than cadida pustules Rupture and dry: collarette of scaling around denuded base Treatment Oral and topical abx Description Salmon-colored lesions w yellow scale Prominent in intertriginous areas No satellite lesions Seb derm of scalp, face, postauricular areas seen May have concurrent infxn with Candida or Pityrosporum Description Recalcitrant scaly eruption with elevated or “active” scaly border Scales can be scraped and demonstrated on KOH Treated with topical antifungals Do NOT use topical steroids A scraping of the skin lesions that appeared 24h after birth in the otherwise healthy neonate shown will likely reveal A. Mulitnucleated giant cells B. Neutrophils C. Mastocytes D. Eosinophils E. Gram-positive bacteria Description Flat, slate-gray to bluish-black, poorly circumscribed macules Location Lumbosacral and buttocks Can appear anywhere Size 1-10cm Single or Multiple Ethnicity 90% AA 80% Asian 10% Caucasian Path Accumulations of melanocytes deep within dermis Fade by age 7 Benign, self-limited Incidence 50% full-term infants Timing 24-48h after birth Up to 10th day Description Intense erythema with a central papule or pustule Few to several hundred Size Pustule is 2-3mm Location Back, face, chest, extremities Palms and soles spared Smear Eosinophils May have a concurrent circulating eosinophilia Course Fades in 5-7d Timing Present at birth Description 1-2mm vesicopustules Ruptured pustules in 24-48h Pigmented macules with a collarette of scale Location Neck, forehead, lower back, legs Can occur anywhere Smear Neutrophils Course Hyperpigmentation fades in 3wks to 3 months Common Description Multiple 1-2cm yellowish- white papules Location Nose and cheeks Cause Normal physiologic response to maternal androgen stimulation Course Resolve by 4-6 months Description Papules and papulopustules Location Face, neck and trunk Cause Hormonal stimulation of sebaceous glands Overgrowth of yeast Course Benign and self-limited Topical antifungals Description Transient, netlike, reddish- blue mottling of the skin Cause Variable vascular constriction and dilatation Location Symmetrically over the trunk and extremities No treatment Normal response to chilling Abates by 6 months EB simplex AD Description Superficial blisters or just above basal cell layer of epidermis Mild to severe blistering Location Widespread Pressure bearing areas After intense physical activity Timing Later infancy, childhood or adolescence Course No scarring Secondary infections Some with atrophy Junctional Epidermolysis Bullosa AR Description Presents at birth Generalized bullae and erosions Junction of epidermis and dermis Course Severe variant Fatal within first year Mild variant Resembles generalized EB Dystrophic Epidermolysis Bullosa Dominant and Recessive Description Deep within the upper dermis Scarring with milia Course Dominant Localized (feet) Recessive Growth and development retardation Severe oral blisters Loss of nails Syndactyly For all types Diagnosis Skin biopsy Prenatal gene testing Treatment Symptomatic Supportive X-linked dominant Seen mostly in females Lethal in most males 3 phases (may present in any phase) First phase Inflammatory vesicles or bullae Trunk and extremities First 2 weeks of life New blisters Next 3 months Biopsy Inflammation with intraepidermal eosinophils and necrotic keratinocytes 3 phases Second phase Irregular, warty papules Resolves spontaneously within several months Third phase Swirling or streaking pattern (Blaschkoid distribution) of brown to bluish-gray pigmentation on the trunk or extremities Lasts many years but gradually fades Leaves subtle, streaky, hypopigmented scars Systemic manifestations 30% CNS Seizures MR Spasticity 35% Ophthalmic Strabismus Cataracts Blindness Microphthalmia 65% Pegged teeth Delayed dentition Treatment None The parents of this newborn infant pictured are inquiring about treatment for the lesion shown. What do you tell them? The infant is at a high risk for cancer with this lesion and needs referral to surgery for excision B. This is a normal variant and the lesion will fade over the first year of life. No treatment is necessary C. The infant should be referred to dermatology for pulsed laser therapy D. While the lesion will not change with time, treatment should be delayed for at least a year E. An oral course of steroids is necessary to help resolve the lesion A.