- NHS West London Clinical Commissioning Group
advertisement

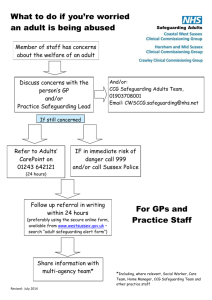
Annual General Meeting 7 July 2015 Dr Fiona Butler Chair Welcome This is our third annual general meeting 2014/15 was our second year as an authorised body Aim to ensure the highest quality care is delivered for our local population The patient is at the heart of all we do Continued to strengthen collaborative working with CCGs in North West London 2 Agenda Item Lead 1 Welcome, introductions and minutes of last meeting Dr Fiona Butler 2 Our achievements in 2014/15 Time 5.00pm 2.1 Patient and Public Engagement Dr Puvana Rajakulendran 5.15pm 2.2 Working in collaboration across North West London Clare Parker 5.25pm 2.3 Quality and safeguarding Jonathan Webster 5.35pm 2.4 Approval of annual report and accounts David Tomlinson 5.40pm 3.1 Our priorities for 2015/16 Louise Proctor 5.55pm 3.2 Making Whole Systems real Dr Richard Hooker 6.05pm 3 Looking forward to 2015/16 4 Questions from the public 5 Last thoughts and introduction to the stalls 6 Close 6.30pm 3 Introduction to the CCG A membership organisation of GP Practices We commission hospital care, community services, mental health services Governing Body of GPs, practice manager, patient representation, lay members and CCG officers Working with Westminster City Council and the Royal Borough of Kensington & Chelsea Developing Primary Care to support new ways of working for patients 4 Our priorities Local influence Transforming primary care Whole Systems Integrated Care Mental health Working in collaboration Local influence, local knowledge Patient representation Capturing patient experience St Charles GPs involved in decision making Patient & public engagement grants programme Transforming primary care: better care, closer to home More services available from your GP Diabetes Telephone consultations; online booking Seven day access to Primary Care Developing a West London Federation North and South Hubs Mental health Local mental health needs Primary Care Mental Health ‘Take time to talk’ Dementia services Integration with physical health Whole Systems Integrated Care Joined up care across organisations Closer to the patient Whole Systems (older people) launching this autumn Patient input at every stage of development Whole Systems long term mental health Local achievements: Patient and Public Engagement Dr Puvana Rajakulendran Clinical Lead for Patient and Public Engagement Our achievements PPE toolkit and deep dives Third sector engagement Primary Care Navigator Programme PPE Grants Patient Participation Groups Festivals and commissioned health road shows Patient representative training Stronger relationship with Healthwatch St Charles Health & Wellbeing Centre 11 St Charles Art Commission Project 12 Working in collaboration across NW London Clare Parker Chief Officer Collaborative working with neighbouring North West London CCGs Collaborative with Central London, Hammersmith & Fulham, Hounslow and Ealing CCGs Shaping a Healthier Future with 7 other CCGs in NW London Our vision of care Mental health – North West London Mental Health & Wellbeing transformation NWL Crisis Concordat Primary Care Acute psychiatric liaison services Dementia strategy and framework Acute reconfiguration – North West London A&E from Hammersmith and Central Middlesex Hospitals NW London Urgent Care Centres 24/7 Ealing Hospital maternity, neonatal & paediatric transition Implementation Business Case development 7 day services Engagement and communications Enabling priorities – North West London Addressing workforce challenges Engaging with member practices Consistent narrative for staff, members and patients Reducing bureaucracy; strengthening governance Quality and safeguarding Jonathan Webster Director of nursing, quality & safety Our achievements in quality and patient safety Safeguarding (Children & Adults) Medicines Management Quality Improvement Patient Experience & Equalities Strategy Development Quality Assurance 20 Annual reports and accounts David Tomlinson Chief Financial Officer Financial duties • Most of our income comes from the Department of Health (DH) • The majority of this is called the Revenue Resource allocation. In some situations we receive a Capital Resource allocation to purchase assets (usually IT) • Costs can be categorised as recurrent (on-going costs) or non recurrent (one-off costs) • We receive a separate allowance to pay for our running costs – such as CCG staff, premises, fees & expenses – This allowance was £25 per head of population in 14/15 and reduces to £22 in 15/16 • We have a statutory duty not to spend more than the income we receive. • We are not allowed to borrow money, go overdrawn or hold cash at year end 22 2014/15 Financial Position The Clinical Commissioning Group met or surpassed its statutory requirements in 2014/15 The CCG did not have a capital resource allocation for 2014/15 and spent no money on capital assets. 2014/15 financial summary Commissioning Area £000's Acute Services 148,390 Community Services 39,370 Prescribing 23,121 Mental Health Services 62,334 Continuing Care 13,315 Primary Care Other Services Total Programme Costs Running Costs Net Operating Expense 9,111 17,463 313,103 5,362 318,465 The table and chart above show how the CCG spent its money. The highest proportion of spend goes on acute services, at 47% of total expenditure. Underlying financial position West London CCG has a strong financial position: • At the end of March 15 our income exceeded our expenditure by £31.5m (our surplus). Within this, the recurrent element of our surplus is £20.7m. But: • There is a national formula that sets out how much funding each CCG should receive based on its population’s characteristics– its capitation target • At the end of 2014-15 our funding allocation was 33.8% higher than our capitation target and in 2015-16 it will be 31.5% higher. • This will correct itself over time as we receive below inflation levels of funding, but we don’t yet know how quickly we will move towards the capitation target. We are starting to see pressure on our recurrent surplus. 25 Financial strategy Our high level financial strategy is therefore: • Our 5 year planning model assumes 1.4% income growth in 2015/16 and beyond. • The CCG needs to generate sufficient QIPP savings to offset the growth in demand for services year on year, which typically exceed this value. • The CCG needs to strengthen its underlying financial position, by only committing non-recurrent funding where possible and pump priming new services that will lead to reduced costs in the longer term (i.e. investing to save). Whole Systems Integrated Care for over 65’s is a prime example. • Supporting the NWL Financial Strategy to enable the 8 CCGs across NW London to invest in out of hospital and primary care services, to deliver the Shaping a Healthier Future programme. Our priorities for 2015/16 Louise Proctor Managing Director The year ahead Primary Care Transformation Integrating services Improving Mental Health Services • Whole Systems • Planned Care • Urgent Care • South Hub estate development 28 Making Whole Systems Integrated Care (Older Adults) real Dr Richard Hooker GP Member Model of care What we have achieved so far… Next steps A model of healthcare delivery Working in partnership North Hub development South Hub development 32 Questions from the public Last thoughts Dr Fiona Butler Chair Introduction to the stalls Primary Care and Planned Care Mental Health Whole Systems (Older people and Mental Health) Patient and Public Engagement 35 Thank you Please send us your feedback Website: www.westlondonccg.nhs.uk Email: wlccg.team@inwl.nhs.uk