Radiographic Assessment - Respiratory Therapy Files
advertisement

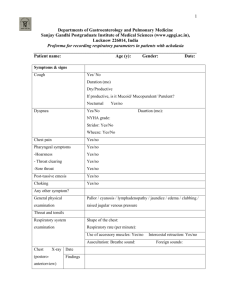
Chapter 8 Radiographic Assessment Introduction • Bedside CXR’s are most common (as opposed to taking the baby to the X-ray dept) • Viewed using picture-archiving and communication system (PACS); useful for quick assessment without radiologist interpretation • AP Frontal and lateral views most common Indications • Identifying position of lines and tubes (OG, UVC, UAC, ETT…) • Visualizing lung fields; correlated with physical assessment • Post intubation, post surfactant delivery, sudden distress… • FBAO Indications • • • • • • • • Air Leaks Pneumothorax Pneumomediastinum Pneumopericardium Pneumoperitoneum Subcutaneous emphysema Pulmonary Interstitial Emphysema (PIE) Air embolism Causes of Air Leaks • • • • • • Over-vigorous resuscitation Intubation/IPPV/NCPAP ‘Fighting’ ventilator High PIP Long I.T MAS; RDS; Pneumonia; Pulmonary hypoplasia; BPD; tachypnea Radiographic Technique • • • • • • • • Frontal Lateral Posteroanterior Anteroposterior Lateral decubitus Forced expiratory-FBAO Oblique Fluoroscopy Frontal AP Right and Left Lateral Lateral Decubitus Lateral Decubitus • Useful in determining mobile pleural fluid and also to better identify a pneumothorax Normal Chest Anatomy • Bone and metallic orthopedic hardwear appear bright white due to greater absorption of light • Air little absorption, less exposure on film, appears black • Soft tissue organs and fluid appear as shades of gray • Incorrect exposure alters normal gray scale, appear whiter if under exposed Reading a CXR • An accurately positioned chest x-ray will demonstrate the lung apices, lung bases, medial and lateral lung fields, and the costophrenic angle of each lung. An air filled trachea is seen superimposed in the midline of the upper thoracic vertebrae. The heart silhouette should be seen without rotation and the lower thoracic vertebral bodies slightly transparent through the mediastinum. •Right clavicle (A) •Right scapula (B), •Right fourth anterior rib (C), right eighth rib (D), •Right costophrenic angle (E), •Left lung apex (F), •Aortic arch (G), hilum (H), heart (I), •left lung base (J), Right hemidiaphragm (white arrow). Reading a CXR • The PA or AP chest radiograph displays a wide range of structures with many superimpositions having various radiographic densities. Furthermore, overlying mediastinal or bony structures may obscure portions of the lungs. Therefore, it is important that image quality be optimal and positioning accurate for diagnosis of subtle abnormalities. Reading a CXR • Heart is composed of soft tissue of waterlike density, clearly demarcated by a distinct edge from adjacent air-filled lung • If the lung becomes waterlike from loss of air, atelectasis, filled with fluid/puss/PNA… the heart edge is no longer seen • Called a silhouette sign- two normal structures lose their distinct edge and blend together PNA- Heart edge missing Normal CXR good heart edge •ANATOMY Location Size & Placement •Lungs •Heart •Thymus •Vessels •Chest wall •H •E •A •R •Half the lateral diameter •Plumper in newborns •T •T H Y M U S •C •H •E •S •T Reading a CXR • AP view accentuates heart size • Pulmonary artery and veins form confluent areas on either side of the heart called the hila • Enlargement of the hila= increased pulmonary vessels or enlarged lymph nodes • Aortic Knob also seen • Mediastinum= heart, aorta, pulmonary branches, great vessels, thymus, vena cava • Close up of upper thorax in a patient with Coarctation of the Aorta. The red arrows point to rib notching caused by the dilated intercostal arteries. The yellow arrow points to the aortic knob, the blue arrow to the actual coarctation and the green arrow to the post-stenotic dilation of the descending aorta . Normal CXR good heart edge Good Technique • This is a good radiograph of the infant chest. Notice that the exposure technique adequately penetrates the thoracic vertebrae. • The head is straight so that the clavicles are not rotated. When performing a pediatric chest x-ray, it is important that the chest is not rotated. Structures such as the trachea should appear over the cervical and upper thoracic vertebrae. This is because the heart must be presented anatomically and its border with the thymus seen. • Good alignment can help identify abnormal anatomical shifts due to congenital disorders (e.g. tetrology of fallot, dextrocardia, etc). • Proper collimation was applied vertically to include the nasogastric tube (blue arrow) and umbilical catheter (red arrow). Overall, this is an excellently positioned and exposed chest x-ray. I would suggest that the proximal portion of the NG tube be moved upward in the future and chest lead moved from the lower lung field. Critique? • At first glance this radiograph may appear to be acceptable; however it is not. • The main reason this radiograph should be repeated is motion artifact and quantum mottling. grainy image appearance (termed quantum mottling) • Notice that the vascular lung marking are ill defined and the bronchi are not aerated. This is because the exposure was taken on expiration. Generally, pediatric radiographers know to watch the inspiration indicator on the ventilator rather than the patient so that exposure is made on full inspiration. • When an infant is not on a ventilator the abdomen rises with inspiration and falls with expiration. The other issue is that the head is not in anatomic position, which causes a misrepresentation of the location of the tip of the endotrachael tube. Critique Continued Alignment of the part is lacking in all directions. While this critique does not normally reference the absence of a position marker it should be noted that this is a serious breach when imaging infants. Congenital variations such as dextrocardia, situs inversus, and others such as transposition syndromes are diagnosed because position markers alert the physician. • • Obviously there is mild chest rotation, wire artifact, and poor vertical collimation of the chest. These three radiographs show why it is important to carefully evaluate ventilated pediatric chest x-rays for motion artifact. On the left is the radiograph being evaluated. The middle radiograph shows the same chest x-ray in black bone window or what is called a positive image (black and whites are reversed). Notice that the lung markings are not seen on the middle radiograph. Compare this to the lung markings seen on the right radiograph. Observe how the lung markings and the heart are well defined on this radiograph. Also observe how motion artifact produces a faint heart shadow and lack of clear lung markings (middle radiograph). Now back to the original radiograph, which is a negative. Does motion artifact now stand out to you? When this radiograph is repeated turn the head to anatomical position, collimate vertically, and make the exposure at peak ventilator inspiration. Case Study • A toddler was brought to the emergency department for increasing respiratory distress over the past few days. He has also had fevers, and was started on antibiotics by his family doctor with no improvement. • In the emergency department he had SaO2 of 89% and was treated with oxygen. Prominent wheeze, with decreased air entry and occasional crackles were noted, predominantly on the right-side of his chest. He showed no response to repeatedly nebulized bronchodilators. • Given this lack of response to therapy, chest radiographs were ordered: •A foreign body in the right main bronchus. There is atelectasis (collapse) predominantly affecting the right lower lobe (note the distinct right heart border on the AP film, and patchy opacities below the foreign body on the lateral film). •Round-shaped foods are the most frequently aspirated objects: •Peanuts, grapes, raisins, and hot dogs… •Nonfood objects include all sorts of items — such as metal dowels from Swedish furniture. Conformable objects are the most difficult to manage and remove. Balloons are the objects most likely to result in death. FBAO • Large objects tend to lodge in the upper airway and trachea (about 20% of airway foreign bodies). They are likely to cause obvious and dramatic signs of upper airway obstruction such as dyspnea, drooling, stridor, and cyanosis — which may ultimately cause death unless expeditiously removed. • More common are smaller objects that pass through the subglottic space. They will usually lodge in a bronchus — usually the right main bronchus — or in a more terminal part of the airway. FBAO Symptoms From the history: • Coughing or choking episodes while eating solid foods (classically nuts), or while sucking a small plastic toy or similar object. This history should never be dismissed — a foreign body is almost always present in the symptomatic child. • Persistent coughing and wheezing. • Delayed presentations may shows symptoms of infection due to secondary tracheitis, bronchitis, atelectasis or pneumonia. • If foreign body ingestion was unwitnessed, there may be no history of aspiration (about 15% of cases). On examination there may be: • no physical signs • reduced breath sounds over all or part of one lung • Wheeze: beware of the sudden onset of a first wheezing episode in a toddler in whom there is no history of allergy, especially if it follows a choking episode. • Features of a secondary tracheitis, bronchitis, atelectasis or pneumonia if presentation is delayed FBAO • • • • • • • • Chest radiographs may show: radio-opaque foreign bodies obstructive hyperinflation (asymmetric) collapse/ atelectasis normal (15% of lower airway foreign body aspirations) Some clinicians prefer full inspiration and full expiration films to check for hyperinflation (impossible in the uncooperative toddler). An alternative is to perform lateral decubitus films, looking for the absence of of decreased lung volume when the obstructed side is dependent. The films should include the nasopharynx to the chest. A normal chest radiograph does not exclude the presence of a foreign body Bronchoscopy is indicated for all patients with a suspected inhaled foreign body, even if the chest radiograph is ‘normal’ — unless the child is completely asymptomatic with a normal physical and radiographic examination. Peanut Rule • rule -- children cannot eat peanuts if they are unable to touch their opposite ear by reaching over their head. Corresponds to about their fifth birthday Silhouette Sign Evaluating Normal Structure Normal Thymus Evaluating the Lungs • Lungs – Lobes – Fissures • Inspiration • Trachea and mainstem bronchi Positioning of Lines and Tubes • Endotracheal tubes – Between thoracic inlet and carina • Vascular catheters Airway Obstruction Airway Obstruction (cont.) Airway Obstruction (cont.) Respiratory Distress Syndrome Pneumothorax Incidence of Pneumothorax • • • • • • • 1-1.5% of all newborns Affects 5-14% of babies admitted to NICUs Males > Females Terms = Pre-terms Spontaneous pneumothorax : 10/15,000 Bilateral in 10-21% Mortality 20% Clinical Presentation • Signs of respiratory distress: grunting, ↑RR, cyanosis/desaturation/respiratory acidosis • Apnea, bradycardia, ↓BP (obstructed shock) • Displaced apex beat • Change in breath sounds • ↑Ventilatory requirements • All occur suddenly Diagnosis • • • • Patient Assessment Tansillumination CXR: Lateral decubitis, AP Direct needle aspiration Treatment • • • • • • • Conservative therapy +/- 100% oxygen If no underlying lung disease No complicating therapy No distress No continuous air-leaks Resolve in 24-48 hrs OXYHOOD, or NC at 100% Treatment Needle aspiration • Equipment • 21-23 G butterfly needle • Cleaning solution • Syringe & 3-way tap • Procedure • Clean skin • Insert needle 2nd/3rd ICS MCL • End of tubing under water & watch for bubbles or • Apply continuous suction to syringe until rapid flow of air • http://www.capefearvalley.com/outreach/outreach/modul es/airleaks/pages/Procedures.htm •http://www.youtube.com/ watch?v=rls9R8iFuck Pneumomediastinum Pulmonary Interstitial Emphysema Meconium Aspiration Syndrome Group B Streptococcal Pneumonia Diaphragmatic Hernia Atelectasis Pneumonia Cystic Fibrosis Acute Respiratory Distress Syndrome Chest Trauma CDH Hour long video on interpetation • http://www.youtube.com/watch?v=H9wbwQrX7c