Reimbursement - Getman, Schulthess & Steere
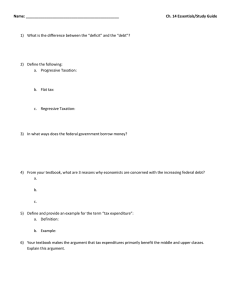
advertisement

PRESENTED BY: Tim Doherty SRS – Specialty Risk Services PO Box 5340 Manchester, New Hampshire 03108 (603) 222-9318 Elizabeth Hurley, Esq. GETMAN,SCHULTHESS & STEERE, P.A. Three Executive Park Drive – Suite 9 Bedford, New Hampshire 03101 (603) 634-4300 MEDICARE, MEDICAID & SCHIP EXTENSION ACT OF 2007 (MMSEA) Legislative Intent: Mandatory reporting requirements to aid in enforcement of Medicare Secondary Payer Act HISTORY OF MSP Enacted 1965 Clarified Secondary vs. Primary Payer Status Workers Compensation Cases – W/C – Primary Payer HISTORY OF MSP Amended in 1980 to Include Liability Policies Medicare Secondary to Liability Insurance Road Map for MMSEA Section 111 Identification: Did the Plaintiff receive Medicare benefits? Road Map for MMSEA Section 111 Notification: claim Medicare – we have a Road Map for MMSEA Section 111 Reimbursement: How much does Medicare get paid back? Road Map for MMSEA Section 111 Reporting: We have settlement or judgment – now what? MMSEA Applies to Primary Payers Primary Payers “any entity that is or was required or responsible to make payment with respect to an item or service (or any portion thereof) under a primary plan.” MMSEA Applies to Primary Payers Primary Payers Responsibility: Judgment Payment Pursuant to a Compromise Settlement Award Contractual Obligation Who Must Contact Medicare? Primary Payer = Responsible Reporting Entity (RRE) Liability Insurance Plan No Fault Insurer Workers Compensation Plan Self-Insurers Third-Party Administrators Group Health Plans IDENTIFICATION CMS QUERY SYSTEM Method by which RRE’s can determine claimant’s Medicare entitlement status RRE submits claimant’s name, SSN, date of birth & gender Confirms entitlement status only – not dates or basis of entitlement Written verification of entitlement status provided Submission of query alone does not satisfy reporting requirements http://www.cms.gov/MandatoryIns Rep/Downloads/NGHPregistration Alert.pdf Direct Data Entry option for occasional reporters, The registration and outline fully explain this reporting option, IDENTIFICATION HOW TO ACQUIRE THE NECESSARY INFORMATION AUTHORIZATION FOR RELEASE OF RECORDS DISCOVERY REQUESTS Notification Identification Send release as soon as claim is made Notification Mail Consent to Release to MSPRC at: MSPRC Auto/Liability [check address as it changes] P.O. Box 33828 Detroit, MI 48232-0998 Fax: (734) 957-0998 Identification SAMPLE INTERROGATORIES 1. Please provide the following information about yourself: (a) Date of birth; (b) Social Security Number or your health insurance claim number (“HICN”); (c) Gender. 2. Are you currently a Medicare beneficiary? If so, Please identify any and all amounts that have been paid by Medicare in satisfaction of medical expenses from any healthcare provider involved in the treatment of your injuries you are claiming in this lawsuit. Please outline any communications that you have had with Medicare and specifically any Medicare secondary payer contractor regarding their lien. 3. If you are not currently a Medicare beneficiary, do you anticipate becoming one during the pendency of this litigation either due to your age or applying for Social Security Benefits? If so, please be sure to supplement your discovery responses accordingly. The information outlined in the above interrogatories is necessary so that the defendant or any insurer of the defendant can comply with the Medicare regulations. See 42 U.S.C. 1395(y)(b)(8) otherwise known as Medicare, Medicaid and SCHIP Extension Act of 2007 (“MMSEA”), Section 111. Identification SAMPLE INTERROGATORIES WRONGFUL DEATH CASES: 1. Please provide the following information about the decedent: (a) Date of birth; (b) Social Security Number or their health insurance claim number (“HICN”); (c) Gender. 2. Was your decedent a Medicare beneficiary? If so, please identify any and all amounts paid by Medicare in satisfaction of medical expenses for any healthcare provider involved in the treatment of your decedent for which are being claimed in conjunction with this lawsuit. The information outlined in the above interrogatories is necessary so that the defendant or any insurer of the defendant can comply with the Medicare regulations. See 42 U.S.C. 1395(y)(b)(8) otherwise known as Medicare, Medicaid and SCHIP Extension Act of 2007 (“MMSEA”), Section 111. Identification Sample Request for Admissions: REQUEST FOR ADMISSION NO. 1: Admit that on ____________ [here insert the date of the accident in question] you were not a Medicare beneficiary and not entitled to Medicare. ADMIT OR DENY: REQUEST FOR ADMISSION NO. 2: Admit that since___________ [here insert the date of the accident in question] you have not become a Medicare beneficiary and are not presently entitled to receive benefits from Medicare. ADMIT OR DENY: Identification SAMPLE REQUEST FOR PRODUCTION Please produce copies of any and all medical expenses or bills that you are claiming in this case with an outline of the specific amounts that have been paid by Medicare. Please also produce any conditional payment summary that you have been provided through Medicare or the Medicare secondary payer contractor. If you do not have this document, please complete and return the attached CMS/MSPRC Consent to Release Authorization. Identification CMS QUERY SYSTEM RREs can Query 1 x Month Each Query can have Multiple Claimants Identification CMS QUERY SYSTEM – Pros & Cons Insurer (RRE) no longer has to rely on opposing counsel to determine claimant/plaintiff’s Medicare status Insurer (RRE) is now directly responsible for determining Medicare eligibility status by submitting inquiry to CMS Notification Medicare’s Coordination of Benefits Contractor (COBC) 1-800-999-1118 Date of Birth Health Insurance Claim Number (HICN) Type of Insurance (liability, no-fault, workers’ comp) Date of Incident Plaintiff’s Full Name, Address and Telephone No. Opposing Counsel’s Name, Address and Telephone No. RRE’s address, Telephone No., Agent and Policy No. List of all Claims using ICD-9 categories Notification COBC opens a potential recovery case and refers matter to second contractor – the MSP Recovery Contractor (MSPRC) MSPRC issues a “MSP Rights and Responsibilities Letter” New Rules: MSPRC might not work directly with RREs or their counsel Reimbursement How Much Does Medicare Get Paid Back? Medicare sends conditional payment letter from CMS/MSPRC This is Initial Demand Reimbursement NEGOTOATING THE LIEN: Write letter to plaintiff’s counsel to send to CMS re: why treatment is not related. Provide IME Reports. Outline pre-existing conditions with copies of selected key records. Reimbursement NEGOTIATING THE LIEN: Procurement Cost – 42 C.F.R 411.37 provides for the reduction based on “procurement costs” or plaintiff’s attorney fees and costs. costs are incurred because the claim is disputed; and costs are borne by the party against which CMS seeks to recover. Reimbursement An Example Calculation of a Recovery Situation with Represented Medicare Claimant in a Liability Case Facts: Settlement of $20,000.00. Attorney’s contingency arrangement of 30% with actual cost of $500. Medicare is asserting a lien of $5,000.00 Attorney’s fees are $6,000.00 ($20,000 x 30%) plus $500.00 provides for total “Cost of Procurement” of $6,500.00 Reimbursement $6,500.00 divided by $20,000.00 = .325, which is the proportional share of the fees and costs. .325 x $5,000.00 Medicare Lien = $1,625.00, which is Medicare’s proportional amount of procurement costs. Subtract $1,625.00 from Medicare’s original lien amount of $5,000.00; which equals $3,375.00. Medicare’s recovery is $3,375.00 from the settlement proceeds of $20,000.00 Reimbursement NEGOTIATING THE LIEN: “Hardship Exceptions” waiver of lien § 1870(c) The plaintiff has the opportunity to apply for a hardship waiver. Medicare can issue a full or partial waiver, or deny the waiver completely Reimbursement Hardship Waiver 50.6.5.1 – Examples of Financial Hardship (Rev. 1, 10-01-03) The demonstrated beneficiary income and resources are at a poverty level standard, such as being in an SSI pay status. Unforeseen severe financial circumstance existing at the time Medicare’s claim comes into existence so long as and no other financial resources to meet this legal obligation. Reimbursement 50.6.5.2 – Recovery Would Be Against Equity and Good Conscience (Rev. 1, 10-01-03) The degree to which the beneficiary contributed to causing the overpayment; Reimbursement The degree to which Medicare and/or its contractors contributed to causing the overpayment; Reimbursement The degree to which recovery or adjustment would cause undue hardship for the beneficiary; Reimbursement Whether the beneficiary would be unjustly enriched by a waiver or adjustment of recovery; and Reimbursement Whether the beneficiary changed their position to their material detriment as a result of receiving the overpayment or as a result of relying on erroneous information supplied to the beneficiary by Medicare. Hadden v. U.S. Slip Copy, 2009 WL 2423114 W.D.Ky.,2009 Plaintiff filed suit to have lien amount reduced. Suit Dismissed. Reimbursement Final Demand Letter This is the actual amount of the lien “We have determined that you are required to repay the Medicare Program $XXX.xx.” Reimbursement Funds Distribution Strategies Await final conditional payment statement, then issue a separate check directly to Medicare, with the balance to the plaintiff. Hold the funds in trust until the Medicare issue can be resolved Reimbursement Almost Final Letter will State: “We have received check number XXXX in the amount of $XXX.xx Reimbursement Final Letter will State: “The amount has been applied to outstanding debt due Medicare. The principal amount of the debt and interest (if applicable) has been reduced to zero and our file is being closed.” Reimbursement MEDICARE SET-ASIDE (“MSA”) ALLOCATION May be needed when settling future medical benefits for individuals who are or will become entitled to Medicare Applies when there is foreseeable, ongoing medical treatment related to settled claim Future Medicare entitlement cannot be waived by claimant Not needed if medicals are left open, i.e. workers comp. Reimbursement CALCULATING AMOUNT OF MSA Amount based on reasonable projection of future medical costs related to injury that would otherwise be covered by Medicare Based on amount that Medicare would ordinarily pay (considering deductibles & co-pays) Based on life expectancy & rated age of beneficiary Reimbursement MSA OPTIONS Self-Administered Accounts – For small amounts – Plaintiff administers following same accounting rules as a professional administrator Custodial Accounts – Larger Amounts – Administered by a professional custodian for a fee Medicare Set Aside Trust – Plaintiff receiving means-tested public benefits (SSDI, Food Stamps, Veterans Benefits or Section 8 Housing. – A formal trust with a trustee Pooled Trust – Plaintiff receives means-tested public benefits – Operated by a non-profit – Pools with other funds for investment purposes. Structured Settlements Reimbursement Medicare Set-Asides & Future Medicals Payment of future medicals and approval of Medicare SetAsides (MSA) are required for workers’ comp claims: Total Payment Obligation to Claimant (TPOC) Section 111 does not specifically require non-WC liability carriers to provide for ORMs or establish MSAs Medicare expects attorneys to disclose future medicals to CMS and may require MSAs in future and can seek claw backs Proposed Release / Settlement Agreement Language acknowledges and stipulates that claimant has consulted with physician and avows that there are no expected future medical expenses associated with this accident. Reimbursement parties have made reasonable efforts to recognize and protect the interests of Medicare pertaining to its conditional payments and possible future payments of medical expenses Reimbursement agrees to indemnify, defend and hold defendant, carrier and their attorneys harmless from any future medical, Social Security, Medicaid, Medicare or contract government health insurance fund claims Reimbursement agree that the amount of the final Medicare lien as stated in the Final Demand Letter, which shall be provided to the defense, will be paid in full out of the proceeds of this settlement and the remainder of the settlement funds paid in accordance with the instructions of counsel. Reimbursement The defense shall then be provided with a copy of Medicare’s Final Discharge Letter Reimbursement Proposed Release Language SIMPLE MSA Same language as above PLUS: - avows that claimant has consulted with her health care providers relative to the need for future care and treatment for injuries related to the incident and the expected costs for same Reimbursement - avows that he will establish a selfadministered Medicare Set-Aside account funded by proceeds from this settlement in the amount of $x,xxx, which is a reasonable amount for payment of certain future medical expenses related to the incident. Reimbursement - avows that this amount will be used exclusively for payments that Medicare might otherwise be called upon to pay in the absence of a Medicare Set-Aside. Reimbursement - avows that the defendant and its carrier have relied in good faith on the representations of claimant and his counsel as to his agreement to honor the obligations herein and adhere to the provisions of The Medicare Secondary Payer Act, 42 U.S.C. sec. 1395y. Reimbursement SUBSTANTIAL MSA Same language as above PLUS: (a) (b) (c) Claimant will establish a dedicated account in which settlement funds in that amount shall be deposited; Claimant has attempted, through a Certified Medicare SetAside Consultant or otherwise, to seek review and approval of that amount and account, and to apprise the defense of any decision, or none, of Medicare regarding the Medicare Set-Aside plan set forth or referenced herein; Medicare Set-Aside Account will be funded by the defense Reimbursement The Medicare Set Aside Account must have restrictions in place such that withdrawals can only be made for purposes of medical care that would have otherwise been paid for by Medicare. AND/OR A strict accounting requirement must be in place in case of future action by Medicare. Reporting Reporting – When to Report… Section 111 Requires “reporting” of Settlements, Judgments, Awards, or other Payments by RREs Reporting Triggering Event “Payment” = Obligation to repay lien arises when payment to claimant has been made. “TPOC” Claimant = Total Payment Obligations to Reporting Date Reporting Requirement Commenced 0ctober 1, 2010 Reporting THRESHOLDS: There are thresholds for Reporting General Liability Claims under Section 111 that impact when a settlement is required to be reported. No need to Report if: -Less than $5,000.00 between January 1, 2011 and December 31, 2011 -Less than $2,000 between January 1, 2012 and December 31, 2012; –Less than $600.00 between January 1, 2013 and December 31, 2013; Reporting After January 1, 2014, EVERY payment made to a Medicare beneficiary concerning a general liability claim must be reported whether the payment is made as a result of settlement, judgment, or for any other reason whether a release is obtained or not. Reporting Section 111 of the Medicare, Medicaid & SCHIP Extension Act – These thresholds do not apply or otherwise relieve a RRE from any obligations under the Medicare Secondary Payer Act to protect Medicare’s interest. In other words….. Still Must Pay the Lien and Protect Medicare from paying for future related treatment. Reporting Final Reporting RRE must “report” using CMS website using “Claim Input File” This can only be done by the RRE Penalties REIMBURSEMENT TO MEDICARE Medicare must be reimbursed within 60 days of receipt of payment by Medicare beneficiary If a liability insurance settlement is made and Medicare is not reimbursed, the third party payer must reimburse Medicare even if it has already paid the beneficiary! Applies regardless of how amounts are designated in settlement (i.e. pain & suffering) Penalties CMS’ STATUTORY RIGHTS TO RECOVERY UNDER MSP Interest if not paid within 60 days of notification – 42 U.S.C. 1395y(b)(2)(B)(ii) Double damages if US must bring action to recover against primary payers – 42 U.S.C. 1395y(b)(2)(B)(iii) Subrogation rights – 42 U.S.C. 1395y(b)(2)(B)(iv) Penalties Fines and Penalties Associated with Section III Any “entity” which fails to comply with the reporting requirements mandated by 42 U.S.C. 1395y(b)(8), which is the codification of Section 111, is subject to a $1,000.00 a day fine, per claim, for noncompliance. Penalties PENALTIES FOR NONCOMPLIANCE Penalties for noncompliance with reporting requirements are $1,000 per day!!! Penalties U.S. v. Harris The U.S. Government sued claimant’s attorney in personal injury case seeking to assert its recovery rights under the MSP. CMS had paid approximately $22,549.67 in Medicare claims submitted on the beneficiary’s behalf. Underlying case settled for $25,000.00 and Medicare agreed to reduce its conditional payments to $10,253.59. Counsel never filed any such appeal and also failed to pay CMS within the statutorily required 60-day time period. Penalties U.S. v. Harris Holding: The government was entitled to recover funds received by a Medicare beneficiary from a settlement in a personal injury action from a ladder retailer. Because the defendant took responsibility for the payment of beneficiary's medical services, the government statutorily reserved the right for reimbursement for the medical services paid for by Medicare. Penalties U. S. v Stricker (E.D. N.D. Ala. 2009) (No. CV-09PT-2423-E) The U.S. government sued to recover conditional payments and double damages plus interest under the Medicare Secondary Payer Act. The parties named in the suit include claimants’ counsel, insurers and corporate defendants. Penalties Plaintiff May Have Cause of Action Medicare beneficiaries also have a potential private cause of action against a “primary plan which fails to provide for primary payment” – Plaintiff can seek double damages against RRE Examples: – Beneficiary can sue if a beneficiary’s Medicare benefits are suspended because an agreement did not properly protect his/her interest; OR – If insurer’s/self-insured’s post-settlement reporting or reimbursement violations interrupted the plaintiff’s Medicare payments WHAT IS THE IMPACT ON RESOLVING CLAIMS? Indemnification clauses shifting responsibility to plaintiff are no longer sufficient to protect the insurer Insurers have an affirmative obligation to report Efforts to address Medicare liens must begin at an early stage in litigation Claimant’s Medicare status must be determined by liability insurer or worker’s compensation carrier Websites Centers for Medicare-Medicaid Services: – www.cms.hhs.gov CMS User’s Guide: – www.cms.hhs.gov/MandatoryInsRep/Downloads/NGHPUserGuide022210. pdf CMS Downloads: – www.cms.hhs.gov/MandatoryInsRep/ Town Hall Transcripts: – www.cms.hhs.gov/MandatoryInsRep/07 NGHP Transcripts.asp/#TopOfPage Medicare Advocacy Recovery Coalition: – www.marccoalition.com MSPRC: – http://www.msprc.info/ www.mymedicare.gov QUESTIONS? THANK YOU FOR YOUR PARTICIPATION! GETMAN, SCHULTHESS & STEERE, P.A.