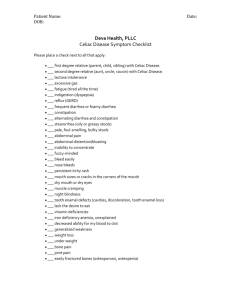
Celiac disease is a common cause of malabsorption of one or more
advertisement

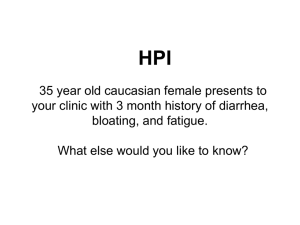
Case scenario:
A 36 years old woman with chronic intermittent diarrhea from
childhood and weight loss,Abdominal distention and bloating,
idiopathic peripheral neuropathy,weakness,fatigue,bone pain
and with unexplained iron-deficiency anemia,Folat deficiency,
Vitamin D deficiency, abnormal liver function tests that by
serologic evaluation and small bowel biopsy and clinicalhistologic response to gluten-free diet, established the
diognosis of coeliac disease.
The patient is worried about risk of malignancy and mortality.
Is she in risk of overal mortality compared with the general
population?
PICO:
P:A 36 years old woman known case of coeliac
disease.
I:Coeliac patient.
C:Non- coeliac patient.
O:Mortality and malignancy.
Meta-analysis:
coeliac disease and the risk of
all-cause mortality
any malignancy
and
lymphoid malignancy
M. Tio, M. R. Cox & G. D. Eslick
Celiac Disease
Celiac disease is
common autoimmune disorder
and common cause of malabsorption
of one or more nutrients.
This picture shows the damage that is caused by gluten
to the microvilli in someone who suffers from Celiac
Disease. As you can see, the image on the left, a
healthy intestine, has much greater surface area than
the one on the right, damaged by gluten
consumption.
Celiac disease is considered an
"iceberg" disease with a small
number of individuals with
classical symptoms and
manifestations related to nutrient
malabsorption
The Celiac Iceberg
Symptomatic
Celiac Disease
Manifest
mucosal lesion
Silent Celiac
Disease
Latent Celiac Disease
Normal
Mucosa
Genetic susceptibility: - DQ2, DQ8
Positive serology
Classical Celiac Disease
(1:4500)
Atypical
Silent
Latent
Detected by screening
(1:250)
Etiology:
The etiology of celiac disease is not
known, but environmental,
immunologic, and genetic factors
all appear to contribute to the
disease.
Environmental factor is the clear association of
the disease with gliadin,a component of gluten
that is present in wheat, barley, and rye.
In addition to the role of gluten restriction in
treatment, the instillation of gluten into both
normal-appearing rectum and distal ileum of
patients with celiac disease results in
morphologic changes within hours.
Sources of Gluten
OBVIOUS SOURCES •
Bread
Bagels
Cakes
Cereal
Cookies
Pasta / noodles
Pastries / pies
Rolls
–
–
–
–
–
–
–
–
Sources of Gluten
POTENTIAL SOURCES
Candy
Communion wafers
Cured Pork Products
Drink mixes
Gravy
Imitation meat / seafood
Sauce
Self-basting turkeys
Soy sauce
–
–
–
–
–
–
–
–
–
•
An immunologic component in the
pathogenesis of celiac disease is critical
Serum antibodies
IgA antigliadin,
IgA antiendomysial,
IgA anti-tTG antibodies—are present.
The antiendomysial antibody has 90–95%
sensitivity and 90–95% specificity. patients
with these antibodies should undergo with
deudenal biopsy.
Genetic factor(s) are also involved in
celiac disease. The incidence of
symptomatic celiac disease is 10% in
first-degree relatives of celiac disease
patients. all patients with celiac disease
express the
HLA-DQ2 or HLA-DQ8 allele, though only
a minority of people expressing
DQ2/DQ8 have celiac disease. Absence
of DQ2/DQ8 excludes the diagnosis of
celiac disease.
Be aware DR3 should now be referred to as DR17
DQ2
DQ2
DR3
{
{
DR3/DR3
DQ8
DR5/DR7
DQA1*0501
DQA1*0201
DQA: Any
DQB1*03
DQB1*0201
CIS
Trans
CIS
APC
Gluten
Genetics
Genes
Several genes are involved
The most consistent genetic component depends on the
presence of HLA-DQ
(DQ2 and / or DQ8) genes.
Other genes (not yet identified) account for 60 % of the
inherited component of the disease.
HLA-DQ2 and / or DQ8 genes are necessary (No DQ2/8,
no Celiac Disease!) but not sufficient for the
development of the disease.
?
?
?
HLA
?
+
Gluten
Celiac Disease
Diagnosis:
A biopsy should be performed in
patients with symptoms and
laboratory findings suggestive of
nutrient malabsorption and/or
deficiency and with a positive
endomysial antibody test.
The diagnosis of celiac disease
requires the presence of characteristic
histologic changes on small-intestinal
biopsy together with a prompt clinical
and histologic response following the
institution of a gluten-free diet. If
serologic studies have detected the
presence of IgA antiendomysial or tTG
antibodies, they too should disappear
after a gluten-free diet is started.
The hallmark of celiac disease is the presence of an
abnormal small-intestinal biopsy (Fig. 294-4) and the
response of the condition—symptoms and the
histologic changes on the small-intestinal biopsy—to
the elimination of gluten from the diet.
The histologic changes have a proximal-to-distal
intestinal distribution of severity, which probably
reflects the exposure of the intestinal mucosa to varied
amounts of dietary gluten.
Diagnosis
1st: Physical exam and blood testing
2nd: Duodenal biopsy
3rd: Implement gluten-free diet
http://www.csaceliacs.org/celiac_diagnosis.php
The classical changes seen on duodenal/jejunal biopsy
are restricted to the mucosa and include:
1:an increase in the number of intraepithelial
lymphocytes.
2: absence or reduced height of villi, resulting in a flat
appearance with increased crypt cell proliferation,
resulting in crypt hyperplasia and loss of villous
structure, with consequent villous, but not mucosal,
atrophy.
3:cuboidal appearance and nuclei that are no longer
oriented basally in surface epithelial cells.
4:increased lymphocytes and plasma cells in the
lamina propria.
Histology of intestinal biopsy in CD
Modified Marsh score
Normal
small
intestine
Small
intestine
with
scalloping
Normal villi
Small
intestine
with villous
atrophy
It Takes A Villi
Damaged •
Healthy •
Duodenum
ENDOSCOPY
CELIAC DISEASE
Scalloped
Gluten-free diet
HISTOLOGY
Normal
Increased IEL
Villous atrophy
Recovering
This is what the small intestine looks like under the microscope when the
mucosa is injured like the left photo shows. The villi are essentially flat
and numerous lymhocytes are near the surface lining.
This endoscopic photo of the small bowel (duodenum) shows
the classic fissuring or cobblestoning of the surface as well as
"scalloping" of the folds in Celiac disease.
This endoscopic photo was taken with special light technique called
Narrow Band Imaging (NBI). It brings out some of features of atrophy,
fissuring or cobblestone appearance of the mucosa (surface lining) and
the "scalloping" of the folds seen in Celiac disease.
The folds are flattened and the mucosa in this patient with
Celiac.
GI symptoms
•
•
•
•
•
•
•
diarrhea
weight loss
weakness
pedal edema - protein malabsorption
easy bruising - vitamin K malabsorption
classic steatorrhea
increase in stool mass in most patients
Extraintestinal features
Hematopoietic
• anemia - iron or folate deficiency, but also
increased blood loss
• B12 deficiency in severe cases
• hyposplenism - may resolve with dietary
therapy
• thrombocytosis with Howell-Jolly bodies
• bleeding diathesis
Osteopenic bone disease
• decrease Ca absorption
• decrease in absorption fat-soluble vitamin D
• binding of Ca and Mg in lumen by unabsorbed
dietary fatty acids
Osteopenic bone disease
• Osteoporosis with bone pain and pathologic
fractures
• paresthesia, muscle cramps and tetany if
severe hypocalcemia
• chronic can result in secondary and even
tertiary hyperparthyroidism
• problems with premenopausal bone mass
Neurologic symptoms
•
•
•
•
•
•
•
•
peripheral neuropathy
myopathy
cerebellar ataxia
myoclonus
cerebral atrophy and dementia
cerebral vasculitis
brain-stem encephalitis
epilepsy and cerebral calcifications
Renal and liver disease
• Glomerulonephritis
• IgA nephropathy may respond to gluten-free
diet
• PBC, PSC and chronic active hepatitis
• elevated transaminases
Autoimmune and
Connective tissue disease
•
•
•
•
•
•
•
Vasculitis
cryoglobulinemia
Sjogren’s syndrome
SLE
selective IgA deficiency
thyroid disease
IDDM- and celiac both have HLA-DR3 and
DQB1*0201 alleles
OB-GYN
•
•
•
•
•
•
Impaired fertility in women
high incidence of spontaneous abortion
low birth-weight babies
reduced breast milk production
paripartum exacerbation or first presentation
correctable with gluten-free diet
Treatment Options
Option #1:
Remove the genes
Option #2:
Remove the grains
Treatment
Only treatment for celiac
disease is a gluten-free
diet (GFD)
Strict, lifelong diet.
Avoid:
Wheat
Rye
Barley
Associated Diseases:
Celiac disease is associated with dermatitis herpetiformis
(DH), Almost all patients with DH have histologic
changes in the small intestine consistent with celiac
disease, although usually much milder and less diffuse
in distribution. Most patients with DH have mild or no
gastrointestinal symptoms.
Celiac disease is also associated with:
Diabetes mellitus type 1
IgA deficiency
Down syndrome
Turner's syndrome.
Dermatits herpetiformis
Erythematous macule >
urticarial papule > tense
vesicles
Severe pruritus
Symmetric distribution
90% no GI symptoms
75% villous atrophy
Gluten sensitive
Dermatitis Herpetiformis
Skin manifestation of coeliac disease.
Raised, red patches, often blistered.
Commonly on elbows/knees/buttocks.
Symmetrical
Skin biopsy, treated with dapsone.
The most important complication of celiac disease
is the development of cancer.
An increased incidence of both gastrointestinal and
nongastrointestinal neoplasms as well as intestinal
lymphoma exists in patients with celiac disease.
The possibility of lymphoma must be considered
whenever a patient with celiac disease previously
doing well on a gluten-free diet is no longer responsive
to gluten restriction or a patient who presents with
clinical and histologic features consistent with celiac
disease does not respond to a gluten-free diet.
Other complications of celiac disease include
the development of intestinal ulceration
independent of lymphoma and so-called
refractory sprue and collagenous sprue.
In the past, patients with celiac disease or DH
had been reported to have a 10-fold
increased risk for certain gastrointestinal
tract malignancies and 40- to 70-fold
increased risk for non-Hodgkin's lymphoma
(NHL).
Recent studies, however, indicate that the
increase in risk of malignancy, particularly
less than initially .lymphoma, is much
believed
Small intestinal lymphoma, often multifocal and diffuse,
accounts for one half to two thirds of the malignancies
complicating celiac disease and typically occurs after 20 to
40 years of disease.
Whereas in the general population, most small intestinal
lymphomas are of B-cell origin, intestinal lymphoma in
celiac disease is typically of T-cell origin.
the term EATL (enteropathy-associated T-cell lymphoma) was
coined to describe both the intestinal and extraintestinal
lymphomas that complicate celiac disease.
EATL commonly is accompanied by mucosal ulceration,
as seen in ulcerative jejunoileitis, and these ulcers
sometimes are the only endoscopic manifestation of
lymphoma.
Although some patients with EATL have a partial or
temporary response to a strict gluten-free diet, most
are eventually unresponsive to gluten withdrawal.
In patients whose disease was previously controlled on a
gluten-free diet, recurrence of gastrointestinal
symptoms (e.g., abdominal pain, weight loss, diarrhea)
should raise the clinical suspicion of lymphoma.
Other features suggesting lymphoma include:
Intestinal obstruction
Intestinal bleeding
Fever
Hypoalbuminemia
Lymphadenopathy
Erythrophagocytosis evident in bone marrow or the
peripheral blood.
Diagnose:
Small intestinal radiology
enteroscopy with biopsy of the mucosa at multiple levels
capsule endoscopy
CT or MR scanning.
If the index of suspicion is high and studies are not
diagnostic, full-thickness biopsy specimens of the small
intestine should be obtained at laparoscopy or
laparotomy with careful examination of the entire
length of the small intestine and examination of
mesenteric lymph nodes. Even with such an aggressive
approach, EATL can be extremely difficult to diagnose.
EATL commonly is fatal:
Overall one-year and five-year survival rates of 31% and
11%, respectively, were reported in one small series,
with long-term survival almost exclusively confined to those
treated with chemotherapy.
one third of the remaining malignancies complicating celiac
disease. The average patient so affected is older than 50
years.
The Swedish study reported elevated risks for small intestinal
cancer (standardized incidence ratio,SIR, 10), oropharyngeal
cancer (SIR, 2.3), esophageal cancer (SIR, 4.2), and primary
liver cancer (SIR, 2.7).
Patients with DH also had a slightly increased overall cancer
risk (SIR, 1.2) owing to excesses of lymphoma and leukemia,
but they had no increases in gastrointestinal carcinomas.
The mechanisms responsible for the increased prevalence of malignancy in celiac
disease are unknown.
potential factors :
Increased crypt mitotic activity
increased turnover of lymphoid cells within the mucosa
penetration of the damaged intestinal mucosa by carcinogens
infection with oncogenic viruses
underlying abnormalities in the mucosal immune system epithelium
and surface
.
the excess risk of malignancies, which was confined to adults,
disappeared after a 10-year follow-up.
This declining risk of malignancies with increased duration of
follow-up, and thus with the length of gluten-free diet,
supports the results of a previous study, which indicated
that a strict gluten-free diet for five years reduced the risk
of all malignancies, not just EATL, to that of the general
population.
Meta-analysis:
coeliac disease and the risk of
all-cause mortality
any malignancy
and
lymphoid malignancy
M. Tio, M. R. Cox & G. D. Eslick
INTRODUCTION:
Coeliac disease is a common autoimmune disorder, with
a prevalence approaching 1% in the United States.
Although it is classically associated with malabsorption
and the attendant complications that can arise from the
malabsorptive state, it has also been associated with an
increased risk of lymphoid malignancies.
This association is particularly clear in the case of a
specific non-Hodgkin lymphoma (NHL) subtype,
enteropathy-associated Tcell lymphoma (EATL), which
has been long established as a complication of coeliac
disease.
The magnitude of the risk of other forms of lymphoid
malignancies is much less clear. Data on lymphoid
malignancy risk other than NHL are scant, and the risk
estimates for the more commonly reported NHL vary
significantly.
Similarly, whether coeliac disease increases the overall
risk of malignancy or not remains unknown, with large
discrepancies in reported estimates.
Coeliac disease has also been associated with an
increased risk of all-cause mortality, although again,
the estimates vary widely, ranging from no association
to a 3.9-fold increased risk.
METHODS:
Search strategy:
Relevant articles were identified by one reviewer
(M.T.) by systematically searching through
MEDLINE (from 1950), PubMed
(from1946),EMBASE (from 1949) and Current
Contents Connect (from 1998) through to 4
January 2012.
No language restrictions were used in either the
search or study selection. A search for
unpublished literature was not performed.
Study selection:
To be included, eligible studies needed to:1-have a
study design of either a cohort or case control;
2-report the risk of all-cause mortality, any specific
mortality any malignancy or any lymphoid malignancy
in coeliac patients.
3-report the risk point estimate as an odds ratio
(OR), hazard rate or relative risk.
4-report the 95% confidence interval (CI) for the point
estimate.
5-use an internal comparison when calculating the
risk estimate.
RESULTS:
From 8698 citations screened by our search, we identified a total of 17
observational studies that met our inclusion criteria (Figure 1). Table
1 shows selected characteristics of the identified studies.2, 8, 15–29.
In terms of study design, nine were case control studies and eight
were cohort studies.
There was heterogeneity in the method of coeliac disease diagnosis,
with six studies using medical records, one study using patient
interview, three studies using patient interview or positive serology
plus positive histopathology and two studies using positive
histopathology. Latent or undiagnosed coeliac disease was used as a
coeliac disease subtype diagnosis in seven studies, with two studies
using positive eurospital tissue-transglutaminase antibodies (Eu-tTG)
plus positive endomysial antibodies (EMA) or positive celikey tissuetransglutaminase antibodies (celikey-tTG), two studies using positive
tTG plus positive EMA, two studies using positive tTG or positive EMA
or positive antigliadin antibody and two studies using positive EMA
alone.
All-cause mortality:
the all-cause mortality meta-analysis of five
prospective studies[8, 22, 24, 26, 29] comprising
of 38 039 coeliac cases with a total of 304 694
individuals, indicating that coeliac patients are at
an increased risk of all-cause mortality with a
pooled OR of 1.24 (95% CI 1.19–1.30). There was
no significant heterogeneity .
Non-Hodgkin lymphoma:
Eight studies[15, 16, 18, 21, 23, 25, 27, 28] (six
case control studies and two cohort studies)
comprising of 110 245 cancer or coeliac cases
with a total of 538 493 individuals were
identified for the non-Hodgkin lymphoma
(NHL) meta-analysis. Coeliac patients were at
significantly increased risk of NHL.This
resulted in a pooled OR of 2.61 (95% CI 2.04–
with no significant heterogeneity.3.33),
T-cell non-Hodgkin lymphoma:
Five studies[15, 16, 18, 25, 28] (four case–
control studies, one cohort study) comprising
of 35 358 cancer cases with a total of 311 888
individuals were identified for the TNHL metaanalysis. The risk of TNHL was significantly
elevated, with a pooled OR of 15.84 (95% CI
7.85–31.94) (Figure 4). There was no
significant heterogeneity (I2 = 55.6%, P =
0.06).
Any malignancy:
Three prospective studies[8, 23, 26] (two cohort
studies, one nested case–control study)
comprising of 5134 cancer or coeliac cases
with a total of 35 582 individuals were
identified for the any malignancy metaanalysis. There was no association between
coeliac disease and the risk of any malignancy,
with a pooled OR of 1.07 (CI 0.89–1.29)
(Figure 5). There was no significant
heterogeneity (I2 = 0%, P = 0.58).
Cause specific mortality and other
lymphoid malignancies:
As shown in Table 2, we found that coeliac patients had an
increased risk of cardiovascular mortality 1.19 (95% CI
1.12–1.27), lymphoproliferative disease/malignancy 2.53
(95% CI 1.59–4.04), Hodgkin lymphoma 2.01 (95% CI 1.01–
4.01) and diffuse large cell B-lymphoma 2.25 (95% CI 1.32–
3.85).
There was no increased risk of any malignancy mortality 1.24
(95% CI 0.96–1.60), lymphoma 1.99 (95% CI 0.29–13.58),
chronic lymphocytic leukaemia 0.80 (95% CI 0.46–1.38) or
multiple myeloma 1.26 (95% CI 0.83–1.90). However, all of
together only two or .these results are based on pooling
three studies
Discussion:
Our systematic review and meta-analysis shows that
coeliac patients are at an increased risk of mortality,
and are at a substantially increased risk of NHL and
TNHL.
Serologically defined coeliac patients are at a similarly
increased risk of both NHL and mortality.
However, coeliac patients do not have an increased
risk of any malignancy overall.
The all-cause mortality results:
This raises the possibility that as the current pooled mortality
risk estimate is based on an average of 13.4 years of follow
up, this may in fact be an underestimate of the true risk.
Further prospective studies with a longer follow-up are needed
to determine if the mortality risk is higher than the current
estimate.
However, our estimate still needs to be interpreted with
caution, as it is limited by the availability of only six studies to
analyse, combined with the heterogeneity in coeliac disease
diagnosis method between studies.
Nonetheless, it is likely that our pooled result is the most
reliable estimate currently available.
This increased risk of all-cause mortality in coeliac patients
may be partly explained by our findings that coeliac
patients have an increased risk of cardiovascular
mortality.
our cardiovascular mortality result is based on only three
studies, more studies using internal comparisons are
required to determine this association.
Further studies examining specific mortality risks among
coeliac patients may help guide future studies on whether
any preventative measures beyond the gluten free diet
could be taken to minimise mortality.
Any malignancy and coeliac disease:
No association between the risk of any malignancy and
coeliac disease was found in our pooled risk estimate.
It is not clear how an increased risk of any malignancy overall is
not found when there is a clear increased risk of NHL, although
one study[36] found a decreased risk of breast cancer in coeliac
disease.
If coeliac disease decreases the risk of certain non-lymphoid
malignancies, it may explain why there is no increased risk of
any malignancy overall.
Further study into the possibility of decreased cancer risks other
than NHL may be warranted. However, it is possible that the
lack of increased risk is due to a lack of statistical power, given
low absolute risk of NHL.
The serology subgroup analysis found that serologically
diagnosed coeliac patients had an increased risk of
mortality and NHL compared with non-coeliac patients.
These results suggest that serologically defined coeliac
patients may be subject to a similar level of risk as
coeliac
patients diagnosed by other means.
However, given that these results are only marginally
significant, further research into clarifying any
association between positive coeliac serology and NHL
and mortality is warranted .
We were not able to determine from our systematic
review and meta-analysis if compliance with a glutenfree diet had any effect on the risk of mortality and
NHL in coeliac patients.
There is evidence suggesting that the gluten-free diet
decreases the risk of mortality and malignancy;
however, some studies have not found this association.
Future studies should include measurement of
compliance with the gluten-free diet.
Conclusion:
Our systematic review and meta-analysis shows that
coeliac patients are at an increased risk of mortality
and non-Hodgkin lymphoma, but do not have an
increased risk of any malignancy overall.
Serologically defined coeliac patients also have an
elevated risk of mortality and non-Hodgkin lymphoma.
Our results are limited by the small number of studies
available for analysis, and by heterogeneity in diagnostic
methods. More studies using internal comparators are
needed, particularly to more accurately determine the
risk of NHL and mortality in both serologically defined
and histologically defined coeliac patients.