Pituitary gland
advertisement

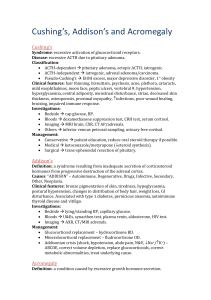
Pituitary gland Gross anatomy of the pituitary gland The average weight of the pituitary gland at birth is about 100 mg. Rapid growth occurs in childhood, followed by slower growth until the adult weight (approximately 500–600 mg) is attained in the latter part of the second decade. The adult hypophysis measures approximately 10 mm in length, 10 to 15 mm in width, and about 5 mm in height Although the adult hypophysis typically measures less than 1 cm in its greatest dimension and weighs less than 1 g, its small size gives a wrong idea about its importance and complexity Embryogenesis of the pituitary gland The pituitary gland originates from two discrete parts of the developing embryo ,(neural & epithelial) The ant. Lobe develop from the roof of the mouth(epith.)and called adenohypophysis The post. Lobe develop from the brain(neural)called neurohypophysis On average, the female gland is almost 20% heavier than the male gland primarily because of relative differences in the size of the pars distalis(adenohypophysis). Furthermore, the weight of the gland increases by 12% to 100% during pregnancy because of enlargement of the pars distalis. the size of the pars nervosa remains relatively constant. The volume of the pituitary gland decreases with aging The pituitary gland derives its blood supply from two groups of arteries. The superior hypophyseal artery (SHA) primarily supplies the anterior lobe, whereas the inferior hypophyseal artery (IHA) is primarily related to the pars nervosa. The SHA can arise from the supraclinoid portion of the internal carotid artery (ICA) or from the posterior communicating artery, whereas the IHA arises from the meningohypophyseal trunk, a branch of the cavernous segment of the ICA The oculomotor nerve, trochlear nerve, and first two divisions of the trigeminal nerve are embedded in the lateral wall of the cavernous sinus, lying between the endothelial lining and the dura mater, whereas the abducens nerve is contained within the sinus itself Pituitary tumors Classifications: a. classification of pit.tumors and tumor like conditions 1.tumors derived from adenohypophyseal cells(adenoma, carcinoma) 2.other primary tumors of sella turcica.(angioma,craniopharyngioma,mening ioma,optic nerve glioma 3.metastatic tumors 4.tumor like conditions(abscess) craniophryngioma Arise from anterior superior margin of pituitary gland. Lined by stratified squamouse epithelium All CP had solid and cyctic part,contain cholestrol crystal (machine oil) CP donot undergo malignant degeneration but malignant behaviour,difficult cure (C.P adherant to the major art. At the base of the brain(int. carotid) craniophryngioma Calcification in plain x ray 54% in childhood ,20%, in adult , 2.5 -4 % of all brain tumor 9% of children brain tu. ,peak incidence age 5-10 year 55-85% five years survival rate 5-10-% mortality due to hypothalamic injurey High recurrence rate in 1st 1-3 years Signs & symptoms Symptoms Headache,nausea &vomiting,visual loss, short stature,mental problems,diplopia Signs Papilledema ,visual defect,endocrine dysfunction,cranial nerve palsy,psychatric abnormality Management Diagnosis Plain x-ray, C.T , M.R.I, endocrine assessment Treatment Surgery(hydrocephalus,cyst drainage) Medical replacement(steroids,A.D.H replacement with fluid) Radiotherapy(better results in children than adults) Treatment of hydrocephalus Ommaya reservior Radiotherapy Linear accelerator Gamma knife radiosurgery Pituitary adenoma b.classification of pituitary adenomas according to endocrine function -SECRETORY 1.prolactinoma 2.GH adenoma 3.ACTH adenoma 4.FSH/LH adenoma 5.T.S.H adenoma 6.plurihormonal adenoma(more than 1 hormone secretion -ADENOMA WITH NO APPERANT HORMONAL FUNCTION c. Classification according to size on radiographic appearance Grade-0 intrapit. Adenoma ,diam.less than 1 cm,normal sella Grade-1 intrapit.ad.,diam.less than 1 cm,focal bulging or minor changes in sellar shape Grade-2 intrasellar adenoma,diam. More than 1 cm,enlarge sella, no erosion Grade-3 diffuse ad.,diam more than 1 cm,enlarge sella, localized erosion Grade-4 invasive ad.,diam more than1 cm,extensive destruction of bony struc.(gohst sella) Adenoma Arise from adenohypophyseal cells 10-15% of intracranial tu. Benign tu. Mostly,slow-growing 1. Adenoma with no apparent hor. Func.(20%) 2. Secretory adenoma(prolactinoma,GH,TSH,ACTH,FSH/LH adenoma PROLACTINOMA Most common functional pituitary tu., accounting for approximately 25% of all pit. Tu.& 3% of all intracranial tumors Prolactin level elevated(200-300ng/ml) ,lower levels may be found if there is other tumors compressing the stalk and interrupt the flow of inhibitory dopamine. Clinical presentation Mass effect (visual field defect(bitemporal hemianopia),impaired acuity,headache,rarely 3rd,4th,6th nerve palsies,hydrocephalus, other endocrinological symp.) women symptoms(primary or secondary amenorrhoea and infertility, galactorrhoea) Men symptoms(decreased libido,impotence,oligospermia) Hyperprolactinoma suppresses the hypothalamic –pituitarygonadal axis) leading to hypogonadism in both sexes DIAGNOSIS Endocrine testing 1.fasting level of prolactine(>150ng/ml indicate that the cause pit.adenoma, if it >1000ng/ml ,it signify the invasiveness of tu. that extend to cavernous sinus) 2. other hormonal assessment(pit.-thyroid ,pit.gonadal(FSH-LH,testosterone),pit-adrenal(a.m cortisol),antidiuretic hor,(urine &serum electrolytes) Neuroimaging studies C.T SCAN of sella with thin slices(1.5-2 mm)plus contrast ,to exclude ac. Haemorrhage. MRI of sellar & parasellar(<2.5mm slices) Cerebral angiography or MRI angio to exclude aneurysms. TREATMENT Mode of treatment depend on : 1.size of tumor 2.the level of serum prolactin. 3.the patient age & overall health. 4.The patient`s tolerance of or compliance with medical therapy. 5.the patient desires fertility. 6.surgical risk factors Indications of surgical treatment of prolactinoma 1.Non invasive tu. With prolactine level(150-500ng/ml) and patient not wish to take long term medications. 2.A woman with non invasive tu.,prl. (<500 ng/ml),who desires pregnancy. 3. A Woman with macroprolactinoma who desire pregnancy. 4.Macroprolactinoma with s.prolactin>500ng/ml 5.Pituitary apoplexy as a complication of prolactinoma> 6.A prolactinoma in pregnant patient causing mass effect( visual loss) 7.A prolactinom that is not respond to medical treatment 8.A recurrent prolactinoma SURGICAL TREATMENT Craniotomy (rt. Frontal) Trans-sphenoidal & transnasal approach craniotomy transsphenoidal COMPLICATIONS OF TRANS-SPHENOIDAL 1.C.S.F leak 2.Meningitis 3.Hypopituitarism & Diabetes insipidus 4.pneumocephalus RADIOTHERAPY: 1.conventional external radiation Adverse effect(hypopituitarysm, optic nerve or chiasmal injury,brain radionecrosis,carcinogenesis) 2.stereotactic radiosurgery (GAMMA KNIFE RADIOSURGERY). Indication(microadenoma or macroadenoma<5 cm) Gamma knife Pituitary apoplexy Acute haemmorrhagic necrosis of a pituitary adenoma&adjacent pituitary tiss. Predisposing factors:pregnency,endocrinologic manipulations(estrogen adminstration,bromocriptine medication),H.injury,chronic cough&sneezing,anticoagulant drugs,cerebral angio.,radiotherapy Symptoms &signs Headache,nausea & vomiting, diplopia&visual impairment, compression of cranial n.s in one or both cavernous sinuses,ophthalmoplegia, meningeal irritation,photophobia Diagnosis(MRA,ANGIO,CT,CLINICAL) Treatment : surgery Acromegaly THE AIMS OF ACROMEGALY TREATMENT (1) to control clinical signs while preserving pituitary function with as minimal adverse effects as possible. (2) to normalize excessive growth hormone (GH) and IGF-1 secretion as quickly as possible, thereby achieving biochemical control (3) to avoid the expansion of the tumor volume and if possible reduce tumor size in order to relieve any symptom due to tumor mass. TREATMENT ALGORITHM Neurosurgery 56:877-885, 2005)SRL=Ssomatostatin receptor ligand ,DA=dopamine agonist) Indications for surgery include active acromegaly visual loss and other forms of mass effect pituitary tumor apoplexy failure of other therapies (medical, radiation). visual compromise develops quite slowly and gradually surgical decompression of visual pathways is usually recommended unless the compression can be resolved by medical treatment. Undisputedly, the most rapid and reliable relief from optic nerve and chiasmal compression is being achieved by surgery, which is particularly appreciated if severe loss of vision occurred acutely, as in pituitary apoplexy Hormonal oversecretion for patients with secretory pituitary adenoma increasing the morbidity and mortality. Clinical diagnosis of these diseases is generally considered an indication for surgery. Because surgery is still generally considered the most rapidly acting and cheapest long-term solution for most patients. recent data suggest that hypopituitarism can also be considered an indication for surgery since pituitary function may be improved following decompression of the gland by selective tumour resection A conservative approach is usually recommended in incidentally detected lesions, which became more frequent with the widespread availability of MR imaging. BUT the progression of a tumour, which is clearly documented in the MR, is another indication to surgically attack a lesion that has already shown an increase in size. Re-operations should be strongly considered if a resectable lesion has not been excised satisfactorily by the primary intervention patients with recurrent disease, if adjunctive medical or radiation therapy failed to achieve control of the adenoma in symptomatic progressions of residual tumours. It seems easier for an expert neurosurgeon with an excellent success and a low complication rate to recommend an operation for a pituitary tumour Radiotherapy Conventional radiotherapy Stereotactic radiosurgery Remission rate (50-60%) Remission rate(17-96%) Time of remission delayed faster growth hormone by several years(10y). Propsed for patients with aggressive adenoma when surgery cannot allow biochemical control. Hypopituitarism increases with time (50-80%),also its more with previosly altered pit. Function(by surgery) hypersecretion decline.(2y) requires a well defined target volume. be used as an alternative primary treatment to surgery. Hypopituitarism(0-33%) Optic neuropathy, radionecrosis, vascular injury were much lower in gamma knife than conventional radiothearapy Pre. Post Post medical.