Obstetrics Anesthesia

2020/4/15
Obstetric Analgesia and
Anesthesia
Prof. Dr.Xia Rui
Head of Department
Presented by:- Dr. Pramee
Department of Anesthesia
The First Affiliated Hospital
Yangtze University
1
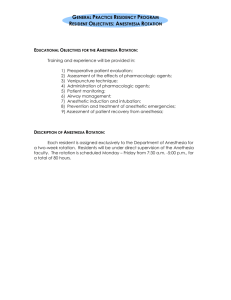
Objectives
Anesthetic implications according to physiological changes in parturients
Effects of anesthetic agents in uteroplacental circulation
Anesthesia for Cesarean section: Regional and GA
Side Effects of Epidural/Spinal Anesthesia
Anesthesia for Painless labor
Analgesia and anesthesia for abnormal obstetrics
2020/4/15 2
Analgesia denotes the state in which only modulation of pain perception is involved. It may be local and affect only a small area of the body; regional and affect a larger portion ; or systemic.
Anesthesia is a triad of hypnosis, analgesia and areflexia by the virtue of anesthetic agents.
2020/4/15 3
In obstetrics , regional anesthesia
more commonly performed for cesarean delivery
local anesthetics (spinal , epidural)
general anesthesia
systemic medication and endotracheal intubation
Difficulty with intubation , aspiration, and hypoxemia leading to cardiopulmonary arrest are the leading causes of anesthesia related maternal death.
2020/4/15 4
Physiological changes during pregnancy
There are considerable physiological changes in parturient which can affect the anesthesia technique
Cardiovascular system
Respiration and metabolism
Center nervous system
Gastrointestinal Tract
Hematology and coagulation
Uterus
2020/4/15 5
1. Cardiovascular system
The anesthetic implication is that these patients due to hyperdynamic circulation can go in congestive heart failure.
2020/4/15 6
2020/4/15
2.
Respiration and metabolism
7
Anesthetic implications of
Respiratory Changes
Due to increased minute ventilation, induction with inhalational agents is faster and dose requirement is less, making pregnant patients more susceptible to anesthetic overdose.
Due to decreased FRC,ERV and increased oxygen requirement these patients are vulnerable to go in hypoxia.So,preoxygenation of 5-6 min is required. This is the time required for maternal fetal equilibrium.
Due to capillary engorgement in upper airway chances of trauma and bleeding during intubation is high.
Laryngeal edema can be the prominent feature of PIH patients, making intubation difficult.
2020/4/15 8
3. Center nervous system
Progesterone has got sedative effect decreasing the anesthetic requirement by 25-40%.
MAC ↓ by 20-40%
↓ Vasopressor response
There is decrease in local anesthetic requirement by
30-40% for spinal and epidural anesthesia.
More chances of high spinal and epidural in pregnancy.
2020/4/15 9
4.Gastrointestinal Tract
Parturients are very vulnerable for aspiration due to following reasons:
Gastric emptying is delayed due to progesterone.
Gravid uterus changes the angle of gastroesophageal junction making the lower esophageal sphincter (LES) incompetent.
Progesterone relaxes the LES.
Gastric contents are more acidic.
2020/4/15 10
Anesthetic implications
A pregnant patient should always be considered as full stomach even if she is fasting.
The minimum fasting period for elective CS is recommended to be 6 hrs for light meals and 8 hrs for heavy meals.
Preoperative antacids—H2-blockers (Ranitidine 100-
150mg orally or 50mg IV)
Metoclopramide 10mg orally or IV
Sellick’s maneuver(cricoid pressure)while intubation.
2020/4/15 11
5.Hematology and coagulation
Blood volume ↑ 50%, increase in plasma volume > increase in RBC mass → relative anemia
Plasma cholinesterase level is decreased by 25% prolonging the effect of succinylcholine.
Hypercoagulable state in pregnancy:↑ platelet turnover, clotting and fibrinolysis
↑ 2,3-DPG→right shift of oxyhemoglobin curve →
↑O
2 delivery
2020/4/15 12
6.Uterus
In supine position the gravid uterus compresses the inferior vena cava and aorta, decreasing the cardiac output and blood pressure causing Supine hypotension syndrome(SHS) which can cause severe hypotension after spinal anesthesia.
To prevent this patient should be kept in left lateral position by:
Putting a 15˚ wedge under the right hip
Tilting the operation table by 15˚to left
Manually displacing the uterus to left
2020/4/15 13
Passing through the maternal-fetal barrier
Drugs with molecular weighs ﹤ 600 cross the placenta easily
By simple diffusion according to the principles of
Fick’s law:
A(C
C
F
)
D
Q/T: rate of diffusion
A: the surface area available for drug transfer
C
M
: maternal drug concentration
C
F
: fetal drug concentration
D: membrane thickness
K : the diffusion constant of the drug
At term, transfer of drugs across the placenta↑
2020/4/15 14
Placental transfer
The rate of drug transfer into the fetus is governed mainly by:
Lipid solubility of drug
Degree of drug ionization
Molecular weight of the drug
Dose administered
Placental blood flow
Placental metabolism
Protein binding.
2020/4/15 15
Placental blood flow and effects of anesthetic agents in uteroplacental circulation
Uterine blood flow is 500-700 ml/min(10% of cardiac output)
Placental blood flow is directly dependent on maternal blood flow.
Effects of anesthetic agents in uteroplacental circulation
Hypotension and drugs causing vasoconstriction can severely compromise fetal well being.
- Ephedrine is drug of choice for treating spinal induced hypotension in pregnancy since it doesn’t decrease placental flow.
2020/4/15 16
Effects of anesthetic agents in uteroplacental circulation Contd..
Positive pressure ventilation cardiac output by venous return compromise placental flow.
Inhalational agents(higher conc.) hypotension , cardiac output compromise uterine flow
IV agents:
Sodium thiopentone and Propofol blood pressure uterine blood flow
Ketamine uterine hypertonicity uterine blood flow.
Spinal/epidural anesthesia hypotension compromise uterine blood flow.
2020/4/15 17
Fetal distribution
All anesthetic drugs except muscle relaxants and glycopyrrolate can be transferred to fetus from maternal circulation. So, all drugs should be used in minimum concentration and dosage.
A large fraction of drug coming from placenta to fetal liver(75% of umbilical vein blood flows through liver), so less drug reaches the fetal vital organs(brain, heart).
Drugs like local anesthetics and opioids which are bases, crosses the placenta in non-ionized form and becomes ionized in the fetal circulation(low pH) and can’t come back to maternal circulation leading to accumulation of drugs in the fetus.
2020/4/15 18
Distribution of drugs between maternal and fetal compartments
2020/4/15 19
The techniques in obstetric analgesia and anesthesia
1. Regional
Spinal anesthesia For Cesarean section
Combined Spinal-Epidural
Anesthesia (CSEA)
Lumbar epidural block For painless labor
Caudal block
2 . Systemic
General anesthesia
2020/4/15 20
Anesthesia for Cesarean section
Spinal anesthesia
Procedure:
1) Preloading:- Ringer’s Lactate 10ml/kg
2) Patient positioning:- Sitting or left lateral
3) Painting and draping
4) Space: L
2
~L
3 or L
Whitacre, Sprotte
3
~L
4
5) Needle: 25 gauge Quincke or 22 gauge
6) Needle advanced to pierce dura. After free flow of
CSF,
7) Drug used: 0.25~0.5% bupivacaine 2-5mg, with or without narcotic (fentanyl 25μg)
Short onset time
Duration of action: 50~70mins
2020/4/15 21
Combined Spinal-Epidural Anesthesia(CSEA)
Immediate onset of analgesia by spinal anesthesia
After giving spinal anesthesia , an epidural catheter is placed immediately prior the surgery
Drug can be re-injected according to the need during the surgery
Most common used in cesarean section delivery
2020/4/15 22
Puncture the spinal needle, fluid from the subarachnoid space
Inject 0.5%bupivacaine
Inject
1.5%lidocaine 23
Spinal/Epidural Anesthesia Contd..
General considerations:
1) Sensory level up to T
6 is required for cesarean section
2) Dose reduction is required due to decreased epidural and subarachnoid space.
3) Left lateral tilt should be maintained to prevent supine hypotension syndrome.
4) If there is significant fetal distress, general anesthesia must be opted since regional anesthesia takes time, esp. epidural anesthesia.
5) Onset of epidural takes time (15-20 mins) so reserved for elective cases only or for condition like PIH.
2020/4/15 24
Advantages of regional anesthesia over general anesthesia
Risk of pulmonary aspiration is bypassed.
Effect of anesthetic drugs on fetus is not seen.
Awake mother can interact with her newborn immediately.
2020/4/15 25
Side Effects of Epidural/Spinal
Anesthesia
Hypotension :There can be significant hypotension with spinal(less with epidural) anesthesia.
Treatment for hypotension:-
Preloading the patient with 500ml-1000ml of Ringer’s lactate
Left lateral position
Oxygen given by face mask .
Ephedrine 5~10mg iv to sustain a mild vasopressor effect.
2020/4/15 26
Side Effects of Epidural/Spinal
Anesthesia
Nausea and vomiting
Due to rapid onset of hypotension and parasympathetic stimulation of the gastrointestinal tract
Treatment:-
Antiemetics: Inj Ondansetrone 4 mg iv
Fluid
Bradycardia
Treatment:-
Inj.Atropine or Inj.Glycopyrrolate
2020/4/15 27
Side Effects of Epidural/Spinal
Anesthesia
Postdural puncture headache(PDPH)
Due to leakage of cerebrospinal fluid through the needle hole in the Dura
Treatment:-
Use a small-caliber needles (25G)
Recumbent position (bed sore)
Hydration
sedation
2020/4/15 28
Side Effects of Epidural/Spinal Anesthesia
Time taken is more than General Anesthesia , so not ideal for fetal distress.
Difficulty in controlling sensory level with spinal anesthesia( chance of high spinal is more in parturient)
Cardiopulmonary arrest
Inadvertent intravascular injection of local anesthetic (toxic reaction) or intrathecal injection of anesthetic (total spinal)
The pregnant patient is more likely to have an intravascular drug injection because of the venous distention in the epidural space
Injection of the drug into a highly vascularized area will result in rapid systemic absorption
2020/4/15 29
Side Effects of Epidural/Spinal Anesthesia
Cardiopulmonary arrest(contd..)
Full cardiopulmonary resuscitation (CRR) is indicated
(establish a patent airway, intubate the trachea, O
2 supply,give vasopressors, treat arrhythmias, provide external cardiac massage)
Then, immediate cesarean section delivery to savage fetus.
2020/4/15 30
Prevention and treatment of local anesthetic overdose
Maximum doses of local anesthetics used in obstetrics
Lidocaine: 5 mg/kg
Bupivacaine: 1.5 mg/kg
Ropivacaine: 3.0 mg/kg
Add epinephrine (1:200,000) to produce local vasoconstriction: prevent too-rapid absorption and prolong the anesthetic effect.
2020/4/15 31
Prevention and treatment of local anesthetic overdose
If manifested by central nerve system toxicity
(convulsion):
Recognize the prodromal sings: ringing in the ears, diplopia, perioral numbness, slurred speech
100 % Oxygen supply
protect the patient’s airway
Inject: thiopental 50mg, midazolam 1~2mg
2020/4/15 32
Anesthesia for Painless labor
Lumbar Epidural Block
Well suited to obstetric anesthesia: vaginal delivery, or cesarean surgery
After evaluation of patient, Epidural catheter is placed once labor is established.
The catheter can be used for surgery and postoperative analgesia
Satisfactory results of analgesia
The fetal outcome is not adversely affected
2020/4/15 33
Procedure: After putting the patient in sitting or left lateral position. puncture sites:L2~3, L3~4
2020/4/15 34
Puncture with the epidural needle and place the catheter
2020/4/15 35
Lumbar epidural block
i. Inject 3ml of a 1.5%
Lidocaine as a test dose . If spinal anesthesia dose not result after 5~10min, inject an additional 5ml .In total
10ml of anesthetic solution is given to accomplish an adequate level of anesthesia.
ii. Continuous infusion
0.125%~0.25% of
Bupivacaine
10~12ml/hr with
Fentanyl 2~5μg/ml in the epidural mixture
2020/4/15 36
Caudal block
An epidural block approached through the caudal space
Seldom used
Hard to perform (the landmarks of the sacral hiatus is obscured , and the fetus might be injured by the needle )
2020/4/15 37
General Anesthesia for Cesarean Section
General considerations:
Usually considered for fetal distress or if contraindication to regional anesthesia-Coagulopathy, infection (at site for spinal), hypovolemia, moderate to severe vulvular stenosis, progressive neurologic disease
Due to high chances to aspiration, prophylaxis should be taken.
Intubation with Sellick’s maneuver (cricoid pressure).IPPV with bag and mask avoided
2020/4/15 38
Difficult intubation should be anticipated and ready for management.
Patient should be nursed in left tilt position.
All drugs should be given in minimal doses as all drugs crosses the placenta and attain equilibrium between mother and fetus in 10~15 mins.
2020/4/15 39
Procedure for GA
Be prepared with antacid
Preoxygenation: Give 100% oxygen with a close-fitting mask for 5~6min
Patient’s abdomen is surgical scrubbed (disinfection) and draped for surgery (anesthetics act on the fetus ↓)
Induction: Thiopental 2-5mg/kg iv or Ketamine 1-2mg/kg
Muscle relaxant: Succinylcholine 1.5 mg/kg
Endotracheal intubation with Sellick’s maneuver
2020/4/15 40
Procedure for GA(Contd..)
Maintenance: 50% Nitrous oxide, 50% oxygen,
(0.5%)halothane or 0.75% isoflurane or 1% Sevoflurane.All inhalational agents relax the uterus and may cause Postpartum
Hemorrhage(PPH).So, low concentration to be used.
Induction to delivery time under 10 mins …..fast!!!
After delivery of the fetus ,the nitrous oxide concentration may be increase to 70%, intravenous narcotics and benzodiazepines injected for supplemental anesthesia
2020/4/15 41
Analgesia and anesthesia for abnormal obstetrics
1) The trapped head in breech delivery
If an epidural block is in place, no further analgesia will be required (forceps?)
General anesthesia is acceptable
2020/4/15 42
2) Fetal distress
Fetus development of bradycardia and appearance of meconium
Uterine perfusion is correlated with BP. Hypotension will aggravate fetal distress
Regional anesthesia can cause hypotension , so usually contraindicated if fetal distress exist.
GA might be required for speedy delivery.
Neonatal resuscitation is needed .
2020/4/15 43
3) Pregnancy Induced Hypertension
(PIH)/Preeclampsia
Composed of hypertension, generalized edema, and proteinuria.
The primary pathologic characteristics is generalized arterial spasm
Regional and general anesthesia are used
Contraindications to regional anesthesia include coagulopathy, urgency for fetal distress
2020/4/15 44
Pregnancy Induced Hypertension
(PIH)/Preeclampsia (Contd..)
If coagulation profile is normal epidural anesthesia is anesthesia of choice because:
These patients can manifest severe, uncontrollable hypotension with Spinal anesthesia( hypertensives are more prone to hypotension after Spinal).
Intubation may be very difficult due to laryngeal edema.
2020/4/15 45
Pregnancy Induced Hypertension
(PIH)/Preeclampsia(Contd..)
If coagulation profile is abnormal GA should be administered.
Extra considerations besides the protocol for C/S to be taken in case of PIH which are:
Intubation to be done by expert hands with minimum trauma
Attenuation of cardiovascular response to intubation to be blunted, otherwise intracranial hemorrhage can occur.
These patients are on Magnesium which potentiates the action of non-depolarizing muscle relaxants(NDMR).so, dose of NDMR should be reduced.
Patients with PIH have decreased levels of cholinesterase, prolonging the effect of succinylcholine
2020/4/15 46
4) Eclampsia
Patient presenting with hypertension, generalized edema, proteinuria and seizure.
Induction should be done with thiopentone(anticonvulsant activity) and followed by GA protocols same as PIH
5) Hemorrhage and shock
Placenta previa and aruptio placenta are accompanied by serious maternal hemorrhage.
Treatment of shock must be formulated.
Ketamine can support BP for induction
Regional block is contraindicated in the presence of hypovolemia
2020/4/15 47
Anesthesia for surgeries during pregnancy
Elective surgeries should be deferred until delivery
Urgent surgeries should be done during second trimester.
First trimester high chances of abortion and congenital abnormalities.
Third trimester high chance of preterm labor
Only Emergency surgeries should be taken in first and third trimester.
2020/4/15 48
Choice of Anesthesia
If possible surgery to be performed under local/ regional anesthesia.
Avoid GA as much as possible.
If GA must be opted ,do not use nitrous oxide. minimum use of inhalational and intravenous agents.
If Spinal anesthesia is to be given, avoid hypotension.
2020/4/15 49