Body Mass Index Charting: Useful Yet Underused in the Pediatric
advertisement
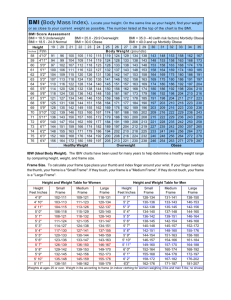
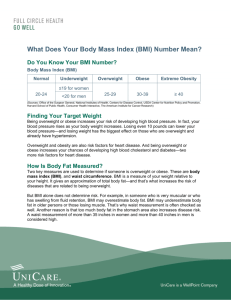
Stemming the tide: Obesity prevention and treatment in primary care pediatrics Eliana M. Perrin, MD, MPH Associate Professor of Pediatrics Department of Pediatrics Division of General Pediatrics and Adolescent Medicine University of North Carolina at Chapel Hill Road Map for Today • My background • My focus: obesity prevention in primary care practice • Earlier project results that form the building blocks for current projects • Current projects • Conclusions and future research directions My background Swarthmore- liberal arts Rochester- biopsychosocial Stanford- academic medicine and weight related disorders UNC- RWJ and faculty and the switch to obesity as a public health problem Six degrees of separation from Indiana How about just two! I love the Tar Heels Hansbrough played for the Tar Heels Now he plays for the Pacers But I digress…. • Right now I spend most of my work time on research – K23 award – R01 award – 2 R03s and AHRQ contract under review • Rest of time I work in primary care pediatrics • Lots of mentorship of medical students, residents, fellows, and junior faculty SCOOPT Lab Possible research focus areas in childhood obesity DOCTOR’S OFFICE CORPORATIONS/POLICY BUILT ENVIRONMENT SCHOOLS BIOLOGY/GENETICS COMMUNITY/ CULTURAL National buy in Primary care prevention involves at least a pediatric provider and a patient (parent and child or family) My research attempts to understand both perspectives and provide interventions that impact both. Primary Care Providers’ Plight • “Healthy People 2010” charged primary care providers with task of curbing the epidemic. • Diagnosis of overweight or trends toward overweight considered one of the 1st steps. • Multiple studies show physicians under-diagnose overweight and obesity in both adults and children. (McArtor RE, et al, Intern’l J of Obesity 1992; Denen ME, Hennessey JV, Markert RJ., J of Gen Int Med. 1993; Eck LH, et al Intern’l J of Obesity 1994; Stafford RS, et al Arch Family Med, 2000, Benson, et al, Pediatrics, 2009) Primary Care Providers’ Plight • Much expected to do with limited time: BP, DBP (toilet training, temper tantrums, discipline, school, ADHD), vision and hearing, immunizations, hct/hgb, lead screening, TB screening, cholesterol, sexuality and STD prevention, injury prevention, violence prevention, sleep positioning, and sleep disturbances, to say nothing of the physical exam, chronic problems, etc. Belamarich PF, Gandica R, Stein RE, Racine AD. Drowning in a sea of advice: pediatricians and American Academy of Pediatrics policy statements. Pediatrics. Oct 2006;118(4):e964-978. • Even obesity screening is complicated… Screening for overweight always involves determining weight for height First complicated aspect of screening… BMI=weight/height2= kg/m2 • In adults: – Definitions for overweight and obesity are static and easy • However, in children: – BMI is a dynamic process that varies as child grows. – BMI values need to be plotted on standardized charts. – A reasonable proxy for weight status. (Dietz WH & Robinson TN, J Pediatrics,1998; Dietz WH & Bellizzi MC, American J Clin Nutr,1999) Second complicated aspect: terminology changes ≥95th % “Obese” previously “overweight” 85th to < 95th % “Overweight” previously “at risk” 5th-85th % Healthy Weight < 5th % Underweight (2007, Expert Committee on Assessment, Prevention, and Treatment of Child and Adolescent Overweight and Obesity, Pediatrics) Overweight Age 4, 93rd Age 4, 87th BMI=17.6 BMI=17.1 Age 5, 94th BMI=17.7 Obese >99th Age 6, BMI=23 Age 12, >99th BMI=29.8 “Visual impression”- how good is it? “Visual impression”- how good is it? BMI ~98th Obese BMI ~93rd Overweight BMI ~12th Healthy . . . . . . . . . . . . . ... . . BMI vs. Height and Weight Study (Journal of Pediatrics, 2004) CONCLUSIONS: • BMI charting compared to height and weight charting • More effective at demonstrating obesity. • Prompted greater concern. • Rarely being used. IMPLICATIONS: • Pediatricians need to detect concerning weight trends. • Further efforts needed to adopt BMI charting. Self-Efficacy Survey Study (Ambulatory Pediatrics, 2005) CONCLUSIONS: • Pediatricians don’t feel effective in treatment/prevention of obesity. • Environmental barriers (like fast food or lack of parks) are most frequently encountered. • Low self-efficacy is associated with practice-based barriers (like lack of EMR to calculate BMI). • Pediatricians want resources including better counseling tools and better ways of communicating weight status to parents. IMPLICATIONS: • Interventions in office-based setting increase self-efficacy increase counseling? Pediatrician Weight Self-Perception Study (Obesity Research, 2005) CONCLUSIONS: • Nearly half of overweight pediatricians did not classify themselves as such and misperception of overweight was worse than in non-doctor US samples. • Those identifying themselves as “thin” & those identifying themselves as “overweight” reported more difficulty counseling regardless of actual weight status. IMPLICATIONS: • Physicians’ own weight self-perceptions may be one barrier to appropriate screening and counseling. Pediatrician self-efficacy with a counseling toolkit (Patient Education & Counseling, 2008) CONCLUSIONS: Pre-/post• Confidence to interpret BMI, identify concerning dietary and PA behaviors and counsel during well child checks improved. • Ease of counseling about healthy eating, PA, and healthy weight improved from less than 10% reporting ease of counseling to nearly 40%. IMPLICATION: • If a very simple toolkit improves self-efficacy and ease, perhaps similar toolkits might help boost counseling rates. Barriers & facilitators of using BMI Pediatrician focus group study (Flower, Perrin, et al, Ambulatory Pediatrics, 2007) CONCLUSIONS: • There are many systems’ barriers to using BMI but it can be a useful diagnostic and even counseling tool. IMPLICATIONS: • Practice-level changes such as incorporating BMI into office systems and EMRs may be needed to support pediatric primary care providers in using BMI routinely. • More research on whether parents understand the concept of BMI or it serves as a communication tool. Do parents understand color-coded BMI charts better than standard charts? What is the relationship of literacy and/or numeracy to that understanding? Oettinger MD, Finkle JP, Esserman D, Whitehead L, Spain TK, Pattishall SR, Rothman RL, Perrin EM. “Color-coding improves parental understanding of body mass index charting.” Acad Pediatr. 2009; 9(5):330-8. Stop-light color coded (à la asthma action plan) vs. standard BMI Methods •N=163 parents (children aged 2-8 yrs) •Two academic pediatric clinics •Parents given: –Demographics, color blindness test, WRAT-3R, S-TOFHLA –“Understanding BMI” questionnaire •Parallel questions -- compare understanding of standard vs. color-coded BMI charting •“Control” questions-- independent of color-coding. Comparison of correctness on parallel questions for B&W vs. color-coded questions (N=163) Question # AOR (95% CI) P value 1 6.5 (3.3-12.6) <0.0001 2 3.5 (2.18-5.53) <0.0001 3 2.0 (1.25-3.14) <0.0005 4 8.8 (5.0-15.4) <0.0001 pooled 4.3 (3.1-6.0) <0.0001 Mean Correct on Questionnaire Performance by numeracy level Numeracy level (WRAT) Summary: Understanding BMI and Numeracy • Many parents reported understanding BMI (60%) but only 33% could explain it correctly. • Parents had greater odds of answering BMI chart questions correctly using color-coded vs. standard charts. • Lower numeracy parents benefited more from color charts than did higher numeracy parents, who performed well using both charts. • “NNT”= 2 to 6 (K-5 numeracy) = 3 to 23 (middle school numeracy) = 5 to 13 (high school numeracy) Use of a Pediatrician Toolkit (Perrin EM, et al, Academic Pediatrics, 2010) CONCLUSIONS: Post toolkit use in an academic clinic: Children had healthier behaviors Parents developed greater accuracy in children’s weight status IMPLICATIONS: Further RCT research needs to be done, but it looks like our toolkit helps change parental perception! These studies have been the building blocks for my current and future research… Now my research is focused on the parent perspective and primary prevention • What do parents find sensitive and motivating? What is their advice for doctors? -K 23 grant in progress • What health effects are there of obesity at young ages and as predictors for the future that parents might find motivating? -Asheley has presented • How can pediatricians best help prevent obesity from the beginning? -R01 grant in progress Context: Parents don’t see the problem of overweight Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics 2000;106:1380-6. Etelson D, Brand DA, Patrick PA, Shirali A. Childhood obesity: do parents recognize this health risk? Obes Res 2003;11:1362-8. Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics 2000;106:52-8. Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don't lowincome mothers worry about their preschoolers being overweight? Pediatrics 2001;107:1138-46. Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics 2003;111:1226-31. Crawford PB, Gosliner W, Anderson C et al. Counseling Latina mothers of preschool children about weight issues: suggestions for a new framework. J Am Diet Assoc 2004;104:387-94. Jeffery AN, Voss LD, Metcalf BS, Alba S, Wilkin TJ. Parents' awareness of overweight in themselves and their children: cross sectional study within a cohort (EarlyBird 21). BMJ 2005;330:23-4. Lampard AM, Byrne SM, Zubric SR, Davis EA, Parents’ concern about their children’s weight., Int J of Pediatr Obesity 2008; 3 (2): 84-92. In my CLINCAL experience, this is how this plays out If child is healthy weight, parent thinks child is skinny parents try to get the child to GAIN weight If the child is overweight, parents think the child is at a healthy weight no motivation to change dietary or PA behaviors Both groups of parents need education about weight status healthy recommendations Can we teach parents about their children’s weight status in a way that is sensitive and motivating? Theory is…. Communication of BMI Understanding the child is an unhealthy weight Intention to change behaviors Behavior change Understanding health consequences Healthier weight trajectory How to do this quickly, effectively, and sensitively??? Interviews with parents Semi-structured interviews • 24 parents of children (12 AA and 12 white) • 4 each of healthy weight, overweight, obese • 1.5 hours; 25 pages of transcript each • Coded themes with Atlas ti software Broad concept of ideal visit and what would be sensitive and motivating Reactions to: • “Ideal” video • Color-coded charts and other tools Interviews with parents study: Demographics Education 16 14 12 10 8 6 4 2 0 8th-11th grade High school/GED Some college Two year degree Graduate degree Interviews with parents study: Demographics Insurance 18 16 14 12 10 8 6 4 2 0 Medicaid Private Among 20 actually overweight parents, self-report: 16 14 12 10 8 6 4 2 0 Healthy Weight Overweight Obese 14 Among 16 overweight children, parents report: 12 10 8 6 4 2 0 Overweight Healthy Weight Interviews with parents study Body Mass Index Previous knowledge and chart preference 12/24 parents indicated they had not heard of the term body mass index. 7/12 indicated they had heard of the term BMI, but incorrectly defined the term when asked. 23/24 parents preferred the color coded BMI chart over the standard chart. Advice From Parents • Give me charts to help explain recommendations • Give me the color-coded chart • Give it to me straight, but be sensitive in your language • Get to know me & make tailored and realistic recommendations • Listen and know me as a person before making recommendations • Tell me more about health than weight Give me charts Yesterday, I went to the doctor with my youngest son who is the middle boy and they weighed him. … And I was concerned that he weighs very, very little. … And I did ask the doctor what about his weight …I don't know what to do. Does he need vitamins? ‘Oh, no. He looks good. He is healthy. He is not bones, bones, bones like he is not eating well.’ For him it was normal. And I still didn't quite understand him because he didn't show me a paper okay…. Like he is at this age, he should weigh this much, he should be tall this size, you know like that. I wasn’t very happy because I wanted to hear something else… He could show me a paper saying this is the age of certain kids, and this is what they weigh…. Charts help explain recommendations The doctor came in and he didn’t say nothing to me about him being overweight or anything like that. He just said we need to talk about a nutrition plan and get him on this and that, and, well, I’m looking at him like I don’t understand why you are telling me this….I think laying it out what you are going to talk about before you decide to talk about it is something that I think is going to help me to not feel like I need to be defensive…. Give me the color-coded chart This one is better (pointing to the color coded chart)…. I am looking at this (the non-color coded chart) and all I see is numbers versus I can look at this and I see the colors and I know yellow is high risk, red is just completely overweight, green is she is doing well and below the green she is underweight, so this helps me to specify where I am…. Give it to me straight! Well, I like the way the lady showed her the chart and explained it to her and came straight out with it and told her that her child was overweight for her age. Instead of just hiding it and not telling her. We are going to try to get her back in the green area where she needs to be at. I see the woman (mother in the video) didn't like it as much, but wow, you know you got to take the bitter with the sweet….. The woman (doctor) is just doing her job letting you know. I like that, I want somebody to tell me something about mine. Well, you think she is overweight, well ok, I am going to work on it. When I come back I guarantee you going to say, ‘Oh, she is fine!’ But be sensitive in your language The doctor should say, “Okay we're a little bit concerned, he looks like he's bigger than most kids his age or something of that sort, then it would've probably been okay, but I don't know, the ‘obese’ word, I, I don't like it.” Get to know me & make tailored and realistic recommendations You have to look at your socioeconomic stuff … You know you have to bring all of that in before you can sit down and make these high hat recommendations like you should take your child to the park more often. Well we don’t have a park in the inner city, not one that is not run by the gangs. So, in order to make the recommendations that the doctors are wanting to make, they are going to need more personal information, and they are going to need a way to get it without offending people. We live on $459 dollars a month and my disability check. Forty fifty nine a month for three people. It is not feasible to recommend fresh vegetables when I can get ‘three-for-a-dollar’ cans, and the cans with the dents for a quarter. And that is the reality. Get to know me & make tailored and realistic recommendations They never really said anything about exercise. Only thing they really say is to water their juice down and try to portion out their foods but they don't really tell you how to manage the foods, what types of foods you should give 'em, you know what kind of exercises you should have them doing you know to make it fun obviously, 'cause a five and a four year-old ain’t gonna just sit there and exercise. Get to know me & make tailored and realistic recommendations They (doctors) usually start saying, ‘OK, your child is overweight. I think you need to make sure they are eating vegetables or getting exercise.’ I’d rather they’d say, you know, ‘tell me about the average day. What is this child eating? How are they exercising?’ And make some real suggestions based on that lifestyle, because, you know, to say to me, ‘Add in vegetables.’ Well, maybe that’s not in my budget. Maybe there is a reason why there aren’t vegetables. You know, to say ‘add in physical activity,’ maybe I work two jobs… and so, you know, to get to a park isn’t as feasible. So, to have that conversation and ask what you are currently doing, and why, and ‘have you thought of this as an option?’ versus ‘do this,’ but throw out different things, because different things are going to work for different families. Listen and know me as a person before making recommendations Because if you listen to me and you get to know me as a person and the things that are going on in my life then I will be more receptive to take what you are saying versus the doctor coming and saying, ‘Hey, you know I heard your child is overweight. Y’all watch a lot of TV? Yeah? Ok, now you need to cut that off.’ Tell me more about health than weight! I would listen to advice on how, you know, I can make them healthier, not help them lose weight, 'cause I don't want to help them lose weight. It's like putting a child on a diet, which I don't think my child needs, either one of them. Another approach: primary prevention Greenlight Study to Prevent Obesity •NIH-funded (NICHD) multiple PI R01 •4 sites: Vanderbilt, NYU, UNC, and UM •Will discuss: –Background –Objectives and Principles –Methods –Measures –Time line Background: Obesogenic behaviors start young By 4 months: • 66% regularly had juice/sugary drink in the bottle • 20% were fed solid food • 18% were fed whenever s/he cried • 29% of formula-feeding babies fed "until s/he finished the bottle" • 33% were fed solid food until the jar was finished At 6 months • Mean media exposure= 159 minutes/day Objectives and Principles • Prevent obesity as measured by % overweight or obese by BMI% at age 2. • Obesity prevention RCT study targeting children at 2 mo of age and following them through age 2 years. – Low literacy educational materials for parents – Addresses cultural challenges, language barriers – Health communication ,teach back, goal setting, motivational interviewing training for residents Methods: RCT with following structure 250 2 mo. olds @ NYU 250 2 mo. olds @ Vanderbilt Obesity Prevention Baseline measures at 2 months 250 2 mo. olds @ UNC 250 2 mo. olds @ U. Miami Attention placebo f/u measures and BMI status at 24 months Measures •BMI% at age 2 •Demographics including very good SES •Dietary and PA measures at every well child check •WRAT and S-TOFLA •PHLAT •Food insufficiency, maternal depression, satisfaction with visit, locus of control, etc. Timeline • • • • Started January, ‘09 Enrolling cohort now- 18 month process Follow cohort for 2 years Cross sectional analyses throughout and cohort analyses at end Conclusions of my research • Parents and doctors do not visualize early concerning weight trajectories, but there ways that doctors and parents can have helpful conversations together. • Providers would benefit from tools that help their selfefficacy, screening, and ways to motivate families to adopt healthy lifestyles. • Color coded BMI charts may help doctors communicate weight status, particularly to those of lower numeracy. • Parents would appreciate sensitive, yet straightforward, tailored communication from providers who know them well. • We anticipate learning a lot about prevention of overweight and injury from our R01 research Future Directions and Goals •Testing a BMI screening communication and early intervention that builds from both parent and pediatrician perspectives. •Further work on the relationships between obesity and health in young children. –Teasing apart vitamin D, PA, and inflammation •R01 has a reverse RCT that helps me learn a new discipline- injury prevention! •Continue mentorship and collaborations. Thank you. I’d like to especially acknowledge many mentors and collaborators: Cynthia Bulik, PhD Alice Ammerman, RD, DrPH Jacob Lohr, MD Michael Simmons, MD Tom Robinson, MD Matt Gillman, MD Joanne Finkle, RN, JD Michael Steiner, MD Asheley Skinner, PhD Kori Flower, MD, MPH Russell Rothman, MD, MPP Shonna Yin, MD, MPH Lee Sanders, MD, MPH Research Assistants: Brenda Calderon and Alison Mendoza Why is parent literacy important for child obesity? • “Health literacy” includes understanding … – Connection between obesity and disease – How to interact with medical system – How to set health-behavior goals • “Health numeracy” includes understanding – Weight status (percentiles) – Food labels – Portion sizes • 3. A pediatrician points to a mark on the BMI chart (point to the X marked on the standard BMI chart indicating a 6 year old boy with a BMI of 20) and tells you that your 6 year old boy falls above the 95th percentile line on the BMI chart. On this chart, below the 5%ile indicates underweight, between the 5%ile and 85%ile indicates healthy weight, between the 85%ile and 95%ile indicates at risk for overweight and above the 95%ile indicates overweight. What does the BMI chart tell you about the weight status of your child?Answer choices: The child is underweight; The child is a healthy weight; The child is at risk for overweight; The child is overweight • 3. The pediatrician points to a mark on the BMI chart (point to the X marked on the color-coded BMI chart indicating a 6 year old boy with a BMI of 20) and tells you that your 6 year old boy falls above the 95th percentile line on the BMI chart. On this chart, green indicates healthy weight, yellow indicates at risk for overweight and red indicates underweight (below) or overweight (above).What does the BMI chart tell you about the weight status of your child? Answer choices: The child is underweight; The child is a healthy weight; The child is at risk for overweight; The child is overweight. NICHD K23 (Perrin, PI) Keep TABS (Talking about BMI Screening): Phase 1, developing the intervention Aim 1. Determine how parents of children ages 3-8 in different BMI risk category groups (“healthy weight,” “at risk for overweight,” and “overweight”) understand and experience communication of BMI screening results via semi-structured and structured interviews. Aim 2. Assess pediatricians’ current knowledge, attitudes, and beliefs regarding communication of BMI weight status screening results to parents of young children via focus groups. Aim 3. Develop and refine theory- and evidence-based intervention tools and strategies to build the Keep TABS (Talking About BMI Screening) intervention that is efficient for pediatricians and potentially motivating to parents, based on qualitative investigation outlined by Specific Aims 1 and 2. Keep TABS Phase II. Perform a Feasibility Study of the Keep TABS Intervention Specific Aim 4. Conduct a feasibility study of our Keep TABS intervention at pediatric practices (N=4; n=2 intervention, n=2 control; 80 parent-child pairs to allow for attrition) to provide essential data to inform a later large multi-site, randomized controlled trial with regard to the following outcomes: Specific Aim 4 Outcomes A. Process outcomes: 1. Determine our ability to recruit patients in different BMI risk profiles. 2. Determine our ability to deliver the Keep TABS intervention (training, implementation, data collection) in busy practice settings. 3. Determine our ability to measure study outcomes, including parental accuracy of assessment of their children’s weight. B. Study outcomes: 1. Determine the effect size, intraclass correlations, and receiver characteristics that will form the basis for the larger effectiveness trial for the intervention, particularly on the primary effect size of interest (parental accuracy of children’s weight status). Ineligible-subspecialty, retired, deceased n=86 NCPS/AAP Members n=824 Allocated respondents n=738 Ht/Wt Vignette Completed n=173 BMI Vignette Completed n=183 Did not return questionnaire n=214 Returned survey but screened out no routine care n=168 Response rate=71% An interesting finding: In one study, while 2 in 5 children whose BMIs were ≥50% by age 3 years were overweight at age 12, none of the children whose BMIs were <50% were overweight at age 12 . (Nader PR, O'Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics 2006, 118:e594-601) Career Development- gaps needed to fill to get to where I’m going • Qualitative methodology (class work and CHAI CORE-behavioral/social interventions training) • How culture intersects with health behavior (class work and observational) • Risk communication and health behavior (private tutorials) • Motivational interviewing (seminars) • Obesity epidemiology (class work and project work) • Randomized trials (summer institute work) • Grant writing (seminars), responsible conduct of research (serve on IRB), manuscript preparation Percentage Difference in CRP Compared to Healthy Weight 1600 1400 1200 Very obese, p<0.01 age 3+ Obese, p<0.01 age 6+ Overweight, p<0.01 age 6+ 1000 800 600 400 200 ye ar s s ar 15 -1 7 Ye -1 4 12 9- 11 Y ea rs ar s 6- 8 Ye s ye ar 5 3- 1- 2 Ye ar s 0 Percentage Difference in ANC Compared to Healthy Weight 60 50 Very obese, p<0.05 age 1+ Obese, p<0.01 age 6+ 40 30 Overweight, p<0.01 age 9+ 20 10 ye ar s 15 -1 7 Ye ar s 12 -1 4 ea rs 911 Y rs Ye a 68 ye ar s 35 12 Ye a rs 0 Percentage Difference in Ferritin/Transferrin Compared to Healthy Weight 160 140 120 Very obese, p<0.05 age 3+ Obese, p<0.01 age 6+ 100 80 60 Overweight, p<0.01 age 9+ 40 20 ye ar s 15 -1 7 Ye ar s 12 -1 4 ea rs 911 Y rs Ye a 68 ye ar s 35 Ye a 12 -20 rs 0 Methodology and Aims of K23 #1-Interviews with parents- what’s motivating and understandable? #2-Focus groups with pediatricians-how do they respond to what parents tell us? #3-Use theory and what is learned from #1 and #2 to develop the communication intervention. #4-Test the intervention: a) process outcomes of feasibility; and; 2) study outcomes-determination of change in parental perception of child’s weight status. Results: Demographic Characteristics % Race/Ethnicity American Indian Asian Black/African American Native Hawaiian/Pacific Islander White/Caucasian Hispanic/Latino Combined centers (N=163) 1 3 48 1 38 9 Results: Characteristics HOUSEHOLD INCOME Combined (163) <$10,000 26% $10,000-19,999 13% 20,000-39,999 32% 40,000-59,999 8% 60,000+ 17% Medicaid or Tenncare 66% Private 33% None 1% INSURANCE MEAN YRS OF EDUCATION 13.5 DOCTOR DISCUSSED BMI AT LAST VISIT 27%