Lymphadenopathy and Malignancy Andrew W.Bazemore, M.D., and
advertisement

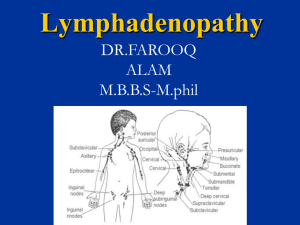
Lymphadenopathy and Malignancy Outline Introducing Historical Clues Physical Examination Nodal Character and Size Diagnosis and Management Lymph Node Biopsy Introducing Lymphadenopathy : an abnormality in the size or character of lymph nodes Categories of Lymphadenopathy : MIAMI Malignancies, Infections, Autoimmune disorders, Miscellaneous and unusual conditions, and Iatrogenic causes The most concerning to the patient and physician : the possibility of underlying malignancy Low Rate of Malignancy in Primary Care : 1.1 % of pt’s presenting to the office with unexplained lymphadenopathy Historical Clues Age and Duration 2. Exposures & History 3. Associated Symptoms 1. Historical Clues : Age and Duration Malignant rate increases with age. A majority of healthy children have palpable cervical, inguinal and axillary adenopathy. Most of them is infectious or benign in etiology. Lymphadenopathy that lasts less than 2 weeks or more than 1 year with no progressive size increase has a very low likelihood of being neoplastic. Rare Exception : low-grade Hodgkin’s/ non-Hodgkin’s lymphomas and, occasionally, chronic lymphocytic leukemia Historical Clues : Exposures & History Animals, biting insects, infectious contacts, recurrent infections, chronic use of medications. Travel-related exposures and immunization status. Tobacco, alcohol, ultraviolet radiation : raise suspicion for metastatic carcinoma Occupational exposures to silicon or beryllium Sexual history and orientation. AIDS pt’s Family history Medications That Can Cause Lymphadenopathy Allopurinol (Zyloprim) Atenolol (Tenormin) Captopril (Capoten) Carbamazepine (Tegretol) Gold Hydralazine (Apresoline) Penicillins Phenytoin (Dilantin) Primidone (Mysoline) Pyrimethamine (Daraprim) Quinidine Trimethoprim/sulfamethoxazole (Bactrim) Sulindac (Clinoril) Historical Clues : Associated Symptoms Constitutional symptoms : fever, fatigue, malaise with atypical lymphocytosis → mononucleosis syndromes Significant fever, night sweats, unexplained BW loss > 10% of normal BW → “B” symptoms of Hodgkin’s lymphoma Arthralgias, muscle weakness, unusual rash → autoimmune diseases such as RA, SLE, dermatomyositis Physical Examination Head and Neck LN Axillary LN Inguinal LN Lymph nodes of the head and neck, and the regions that they drain Head and Neck Lymphadenopathy In one outpatient primary care study : cervical LNs are palpable in 51% of adult physicals, with the incidence declined with age. Infection is the most common cause Most cases resolve quickly; some entities can create persistent lymphadenopathy for months. (ex. Atypical mycobacteria, cat-scratch disease, toxoplasmosis, kikuchi’s lymphadenitis, sarcoidosis, Kawasaki’s syndrome.) Supraclavicular nodes are the most likely to be malignant and should always be investigated, even in children. Axillary lymphatics and the structures that they drain Axillary Lymphadenopathy Most of cases are nonspecific or reactive to local injury/infection in etiology. Persistent lymphadenopathy is less commonly found in the axillary nodes than in the inguinal chain. Breast adenocarcinoma often metastasis initially to the anterior and central axillary nodes, which may be palpable before discovery of the primary tumor. Antecubital or epitrochlear lymphadenopathy can suggest lymphoma or melanoma of the extremity. Inguinal lymphatics and the structures that they drain Inguinal Lymphadenopathy It is common, with nodes enlarged up to 1 to 2 cm in diameter in many healthy adults, but it is of low suspicion of malignancy. Benign reactive lymphadenopathy and infection are the most common etiologies. Although some tumors, such as Hodgkin’s lymphomas, penile/ vulvar SCC, melanoma in this area, may present with inguinal lymphadenopathy, it is typical presenting finding in neither case. Generalized Lymphadenopathy Generalized lymphadenopathy : lymphadenopathy found in two or more distinct anatomic regions More likely to result from serious infections, autoimmune diseases, and disseminated malignancies. Specific testing is usually required. Generalized adenopathy infrequently occurs in pt’s with neoplasms, but it is occasionally seen in patients with leukemias and lymphomas, or advanced disseminated metastatic solid tumors. Nodal Character and Size Hard and painless nodes have higher suspicion of malignancy or granulomatous disease. Viral infection typically produces hyperplastic nodes that are bilateral, mobile, nontender, and clearly demarcated. Palpable supraclavicular, iliac, or popliteal nodes of any size and epitrochlear nodes larger than 5mm are considered abnormal. Increasing size and persistence over time are of greater concern for malignancy than a specific level of nodal enlargement. Algorithm for evaluation, diagnosis, and management. Diagnosis and Management The first step : reviewing pts’ medications, considering unusual causes of lymphadenopathy, and reconsidering the risk factors for neoplasm. If a diagnosis is not suggested, and the patient is deemed low risk for neoplasm, the regional lymphadenopathy can be safely observed. It is suggested that non-inguinal lymphadenopathy lasting more than one month merits specific investigation or biopsy. Lymph Node Biopsy Once biopsy has been chosen, ideally the largest, most suspicious, and most accessible node is selected, taking into account differing diagnostic yields by site. Inguinal nodes offer the lowest yield, and supraclavicular nodes have the highest. Excisional biopsy remains the diagnostic procedure of choice. Persistent Generalized Lymphadenopathy (PGL) Presenting Signs and Symptoms Lymph nodes larger than 1.5 cm in diameter in 2 or more extrainguinal sites of 3 or more months duration Nodes are non-tender, symmetrical, and often involve the posterior cervical, axillary, occipital, and epitrochlear nodes Overview Swelling of lymph nodes is a frequently encountered symptom It is important to carry out a careful history and physical exam The cause often becomes obvious, but in more complicated cases, laboratory tests and lymph node biopsy may be necessary to establish a definitive diagnosis Diagnostics Where possible, do a CBC (FBC) and chest xray before making a diagnosis of PGL Hilar or mediastinal lymphadenopathy on CXR Management and Treatment No specific treatment for PGL Unique features, Caveats Develops in up to 50% of HIV-infected individuals Up to one-third do not have any other symptom on presentation (WHO clinical stage 1) In HIV-positive patients, PGL is a clinical diagnosis. No further examinations are necessary, unless there are features of another disease PGL may slowly regress during the course of HIV infection and may disappear before the onset of AIDS Tuberculosis lymphadenopathy Presenting Signs and Symptoms Cervical nodes most commonly involved Usual course of lymph node disease is as follows: Firm, discrete nodes fluctuant nodes matted together skin breakdown, abscesses, chronic sinuses healing and scarring Diagnostics Fine-needle aspiration of the involved lymph node Extra-thoracic lymph node aspiration Positive smears for acid-fast bacilli on fineneedle aspirates of the involved lymph nodes (high rate in HIV patients) In smear-negative pulmonary TB, it is worthwhile aspirating extra-thoracic lymph nodes to confirm diagnosis of TB (80% positive) TB abscess as part of immune reconstitution syndrome Management and Treatment Treatment should be started following the national TB Guidelines. For further details, see Part A Module 2, Session 3. Unique features, Caveats One of the most common forms of extrapulmonary TB in HIV patients Fluctuant cervical nodes that develop over weeks to months without significant inflammation or tenderness suggest infection with M. tuberculosis, atypical mycobacteria, or scratch disease (Bartonella henselae). In severe immunocompromised patients, tuberculosis lymphadenopathy may be acute and resemble acute pyogenic lymphadenitis Miliary TB is an important consideration in patients with generalized lymphadenopathy