Lymphadenopathy
advertisement

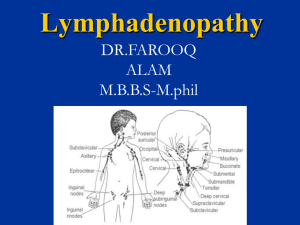
Lymphadenopathy Surapon Wiangnon References • Ferrer R. Lymphadenopathy: Differential Diagnosis and Evaluation. American Family Physician October 15, 1998 • Nelson Textbook of Pediatrics. 17th edition. 2004 • Oski’s Pediatrics, Principles & Practice. 2006 General principles • usually a result of benign infectious causes. • Mostly diagnosed on the basis of a careful history and physical examination. • Localized adenopathy should prompt a search for an adjacent precipitating lesion. • In general, cervical, axillary lymph nodes greater than 1 cm and inguinal > 1.5 cm in diameter are considered to be abnormal. • Generalized adenopathy should always prompt further clinical investigation. Definition • Lymphadenopathy refers to nodes that are abnormal in either size, consistency or number. • "generalized" if lymph nodes are enlarged in two or more noncontiguous areas • "localized" if only one area is involved. • Generalized lymphadenopathy almost always indicates the presence of a significant systemic disease. Lymphoid type Epidemiology • Population-based study (Dutch): 10% of patients with unexplained adenopathy required referral to a subspecialist, and only 1 percent had a malignancy • In primary care settings, patients 40 years of age and older with unexplained lymphadenopathy have about a 4 % risk of cancer versus a 0.4% risk in patients younger than age 40. (Fijten GH, Blijham GH. Unexplained lymphadenopathy in family practice. An evaluation of the probability of malignant causes and the effectiveness of physicians' workup. J Fam Pract 1988;27: 373-6) Evaluation of possible adenopathy • • • • Is the swelling a lymph node? Is the node enlarged? What are the characteristics of the node? Is the adenopathy local or genralized? Physical examination Five characteristics should be noted and described: • • • • • Size. normal if < 1 cm in diameter; Abnormal: epitrochlear nodes > 0.5 cm inguinal nodes > 1.5 cm Pain/Tenderness. inflammatory process or suppuration, hemorrhage into the necrotic center of a malignant node. Consistency. Stony-hard nodes: cancer, usually metastatic. Very firm, rubbery nodes: lymphoma. Softer nodes: infections or inflammatory conditions. Suppurant nodes may be fluctuant. "shotty" (small nodes that feel like buckshot under the skin) cervical nodes of children with viral illnesses. Matting. benign (e.g., tuberculosis, sarcoidosis or lymphogranuloma venereum) malignant (e.g., metastatic carcinoma or lymphomas). Location. Lymph Node Groups: Location, Lymphatic Drainage and Selected Differential Diagnosis Location Lymphatic drainage Causes Submandibular Tongue, submaxillary gland, lips and mouth, conjunctivae Infections of head, neck, sinuses, ears, eyes, scalp, pharynx Submental Lower lip, floor of mouth, tip of tongue, skin of cheek Mononucleosis syndromes, Epstein-Barr virus, cytomegalovirus, toxoplasmosis Jugular Tongue , tonsil, pinna, parotid Pharyngitis organisms, rubella Posterior cervical Scalp and neck, skin of arms and pectorals, thorax, cervical and axillary nodes Tuberculosis, lymphoma, head and neck malignancy Suboccipital Scalp and head Local infection Lymph Node Groups: Location, Lymphatic Drainage and Selected Differential Diagnosis Location Lymphatic drainage Causes Postauricular External auditory meatus, pinna, scalp Local infection Preauricular Eyelids and conjunctivae, temporal region, pinna External auditory canal Right supraclavicular node Mediastinum, lungs, esophagus Lung, retroperitoneal or gastrointestinal cancer Left supraclavicular node Thorax, abdomen via thoracic duct Lymphoma, thoracic or retroperitoneal cancer, bacterial or fungal infection Axillary Arm, thoracic wall, breast Infections, cat-scratch disease, lymphoma, breast cancer, brucellosis, melanoma Lymph Node Groups: Location, Lymphatic Drainage and Selected Differential Diagnosis Location Lymphatic drainage Causes Epitrochlear Ulnar aspect of forearm and hand Infections, lymphoma, sarcoidosis, tularemia, secondary syphilis Inguinal Penis, scrotum, vulva, vagina, perineum, gluteal region, lower abdominal wall, lower anal canal Infections of the leg or foot, STDs (e.g., herpes simplex virus, gonococcal infection, syphilis, chancroid, granuloma inguinale, lymphogranuloma venereum), lymphoma, pelvic malignancy, bubonic plague Common causes of generalized lymphadenopathy • Infections: Typhoid fever, TB, AIDS, mononucleosis, CMV, rubella, varicella, rubeola, histoplasmosis, toxoplasmosis • Autoimmune diseases: RA, SLE, dermatomyositis • Malignancies: primary: HD, NHL, histiocytic disorders, metastatic: leukemia, NB, RMS • Lipid storage diseases: Gaucher, Niemann-Pick • Drug reactions Medications That May Cause Lymphadenopathy Allopurinol Atenolol Captopril Carbamazepine Cephalosporins Gold Hydralazine Penicillin Phenytoin Primidone Pyrimethamine Quinidine Sulfonamides Sulindac . Pangalis GA, Vassilakopoulos TP, Boussiotis VA, Fessas P. Clinical approach to lymphadenopathy. Semin Oncol 1993; 20:570-82 Common causes of regional node enlargement • Occipital: roseola, rubella, scalp infections • Preauricular: cat-scrath disease, eye infections • cervical: Streptococcal/staphyllococcal adenitis or tonsillitis, mononucleosis, toxoplasmosis, maligancies, Kawasaki disease • Submaxillary: HD, NHL, tuberculosis, histoplasmosis Common causes of regional node enlargement • Axillary: infections of arm/chest wall, catscratch disease, malignancies • Mediastinal: maligancies (T-cell leukemia/lymphoma, thymoma, teratoma), TB • Abdominal: malignancies, mesenteric adenitis • Illioinguinal: infections of leg, groin Indication for biopsy • increase in size over baseline in 2 weeks • no decease in size in 4-6 weeks • no regression to normal in 8-12 weeks • development of new signs and symptoms Caution! • Biopsy should be avoided in patients with probable viral illness because lymph node pathology in these patients may sometimes simulate lymphoma and lead to a falsepositive diagnosis of malignancy. • Fine-needle aspiration is occasionally considered an alternative to excisional biopsy but is often unhelpful. Final Comment • In most patients, lymphadenopathy has a readily diagnosable infectious cause. • A diagnosis of less obvious causes can often be made after considering the patient's age, the duration of the lymphadenopathy and whether localizing signs or symptoms, constitutional signs or epidemiologic clues are present. • When the cause of the lymphadenopathy remains unexplained, a 10-14 day (3-4-week) observation period is appropriate when the clinical setting indicates a high probability of benign disease.