Management of Nausea and Vomiting in the
advertisement

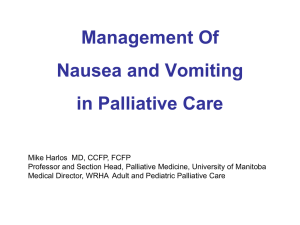
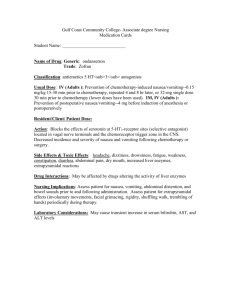
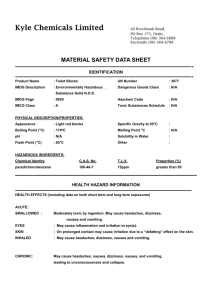
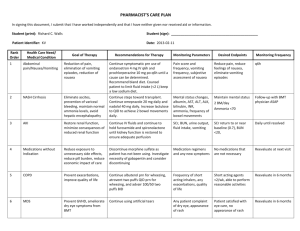
“I am Sick of Feeling Sick” Managing Nausea and Vomiting in the Palliative Patient Paul Daeninck WRHA Palliative Care Program Greg Harochaw Taché Pharmacy Declaration Advisor or Paid Speaker for the following: Valeant Pharmaceuticals Bayer Wyeth Pharmaceuticals Objectives At the end of this session, the attendee will be able to: Identify the numerous GI issues causing nausea and vomiting in the palliative patient Discuss the principles in determining the therapies for specific situations of nausea and vomiting Recognize the complex physiology and potential for use of alternative routes in treating nausea and vomiting GI Issues Causing Nausea/Vomiting Medications Radiation Constipation Bowel obstruction Diarrhea Ascites Hemorrhage Viscus perforation Esophageal/gastric/ biliary duct obstruction Liver failure Pancreatic failure Absorption syndromes Infections Electrolytes Approach To Symptom Control Thorough assessment history; physical examination Discussion goals of care, hopes, expectations, anticipated course of illness (impact on investigations & interventions) Investigations blood tests, X-Ray, CT, MRI, etc Treatments pharmacological and non-pharmacological; interventions Ongoing reassessment/review Options, goals, expectations, etc. Symptom Prevalence Pain Fatigue/Asthenia Constipation Dyspnea Nausea Vomiting Delirium Depression/suffering 80 - 90+% 75 - 90% 70% 60+% 50 - 60% 30% 30 - 90% 40 - 60% Mechanisms of Nausea & Vomiting vomiting centre: medulla activated by stimuli from: Chemoreceptor Trigger Zone (CTZ) area postrema, floor of 4th ventricle outside BBB (fenestrated venules) Upper GI tract & pharynx Vestibular apparatus/Cerebellum Higher cortical centres Chemoreceptor Trigger Zone Vo m Vestibular Cerebellar Opioids Cerebellar Tumor Increased Intracranial Press Primary or Metastatic Tumor G. Michael Downing Integrative Vomiting Centre (IVC) iti ng au sea Sights, Smells Memories N Cerebral High CNS Toxic Cancer Infection Radiation Drugs Chemotherapy Opioids Digoxin, etc Biochemical Uremia Hypercalcemia GI Tract Vagal Distension Over-eating Gastric Stasis Ext. Pressure Obstruction High, mid, low Constipation Chemical Irritants Blood, drugs Pathogenesis of chemo- & RT-induced emesis (CIE, RIE) Area postrema 3rd vent N/V Related Problems Medical dehydration / electrolyte abnormalities esophageal tears / GI bleed aspiration pneumonia Decreased QoL weight loss / anorexia weakness / lethargy Psychological distress Refusal of beneficial therapy Principles of Therapy Treat the underlying cause Environmental measures Antiemetic use: anticipate need use adequate, regular doses aim at receptor involved combinations if necessary anticipate need for alternate routes Environmental Measures Limit exposure to food smells open food trays prior to presentation Bland foods (BRAT) Small, frequent snacks/meals Good oral hygene Fresh air, calming environment Sitting upright post meal Avoid alcohol Acupuncture/pressure Not as well studied Safe in trained hands Often used in conjunction with meds Some evidence in CINV, delayed NV Theory behind wrist/pressure bands Dibble et al. Oncol Nurs Forum 2007 34:813-20 Weightman et al. BMJ 1987 295:1379 Anti-Emetic Agents Transdermal scopolamine Benzodiazepines Antihistamines Cannabinoids Metoclopramide, Domperidone Neuroleptics / Anti-psychotics Corticosteroids 5-HT3 Antagonists NK1 Antagonists (aprepitant) Chemoreceptor Trigger Zone Vo m iti Vestibular Cerebellar H1 Antagonist Dimenhydrinate Methotrimeprazine Anticholinergic Scopolamine Atropine Cannabinoids Increased Intracranial Press Dexamethasone ? VP Shunt G. Michael Downing Integrative Vomiting Centre (IVC) Anticholinergic Scopolamine Atropine H1 Antagonist Dimenhydrinate Cyclizine Methotrimeprazine 5HT2 Antagonist Methotrimeprazine 5HT3 Antagonist Ondansetron ng au sea Benzodiazepines Cannabinoids Relaxation N Cerebral High CNS D2 Antagonist Prochlorperazine Haloperidol Methotrimeprazine Gastrokinetics Metoclopromide 5HT3 Antagonist Ondansetron Granisetron Olanzepine? GI Tract Vagal D2 Antagonist Gastrokinetics Metoclopromide Domeperidone Phenothiazines Methotrimeprazine 5HT4 Agonist Metoclopromide 5HT3 Antagonist Ondansetron Octreotide Dexamethasone Cannabinoids Antiemetics and Dosing Haloperidol 0.5 - 1 mg po/sq/iv q4-12h DOPAMINE ANTAGONISTS MTMZ 5 - 10 mg po/sl/sq q4-8h ANTIMUSCARINIC Scopolamine patch (Transderm-V) PROKINETIC Prochlorperazine 5 - 20 mg po/pr/iv CPZ 25 - 50 mg po/pr/iv Metoclopramide 10 - 20 mg po/sq/pr q4-8h Domperidone 10 mg po q4-8h Antiemetics and Dosing H1 ANTAGONISTS Dimenhydrinate 25 - 100 mg po/pr q4-8h SEROTONIN ANTAGONISTS Ondansetron 8 -16 mg q 12 h po/sq/iv Granisetron 1- 2 mg q 12 h po/sq MISCELLANEOUS Promethazine 25 mg po/iv q4-6h (Not sq) Meclizine 25 mg po q6-12h Dexamethasone 4-16 mg po/sq/iv daily Lorazepam 0.5 - 1 mg po/sl q4-12h Nabilone 0.5-1 mg po/sl q8-12h Olanzepine 2.5-10 mg OD Olanzepine Atypical antipsychotic agent Used in schizophrenia, delirium Blocks multiple receptors D1-4, 5-HT2/3/6, α1adrenergic, H1, M1-4 High affinity for serotonin vs dopaminergic Well tolerated Few drug interactions Olanzepine Has been used in several case studies Recently used in CINV and delayed NV Good results with few problems May also have some appetite benefits Less expensive than 5-HT3 antagonists Navari et al. Support Care Cancer 2007 Mar 21 Navari et al. Support Care Cancer 2005 13:529-34 Passik et al. Cancer Invest 2004 22:383-8 Passik et al. JPSM 2003 25:485-89 Srivastava et al. JPSM 2003 25:578-82 Jackson et al. J Pall Med 2003 6:251-55 Cannabinoids & Nausea • The Nucleus of the Solitary Tract (NTS) receives information about: Blood-borne emetics via the brainstem (BS) CTZ Abdominal irritants via vagal afferents • NTS neurons, in turn, project to a BS central pattern generator, which coordinates emesis behavior Cortex Limbic System • Higher cortical and limbic Brainstem Emetic Circuitry Dorsal Vagal Complex—NTS Stomach Wall regions (governing taste, smell, sight, pain, memory and emotion) can suppress or stimulate nausea and vomiting through descending connections to the BS emetic circuitry • Cannabinoids are thought to exert their antiemetic effects primarily via action on CB1 receptors in the NTS and higher cortical and limbic regions Indirect, partial actions on 5-HT and DA signaling via 5-HT3 and D2 receptors are implicated Cannabinoids in CINV 20 pts, RCT, P vs THC, X-over 10 or 15 mg/m2 po q4h x 3, various tumours Chemotherapy not specified Anti-emetic effect seen in 14/20 THC vs 0/22 P (p<0.001) No patients vomited while “high” Sallan et al, NEJM 1975 293: 795-797 Cannabinoids in CINV 30 RCTs systematically reviewed N=1366 pts; 25 trials X-over design Nabilone, dronabinol, levonantradol (IM) Stemitil, domperidone, metoclopramide Variety of tumours Low to highly emetogenic chemotherapies Studied first 24 h (acute efficacy) Tramer et al, BMJ 2001 323:16-23 Cannabinoids in CINV Oral nabilone (16) Prochlorperazine (7) metoclopramide, alizapride domperidone (2) chlorpromazine, placebo (4) Oral dronabinol (13) prochlorperazine (6) metoclopramide (2) haloperidol, placebo (6) IM levonantradol (1) chlorpromazine Tramer et al, BMJ 2001 323:16-23 Control of N/V with Cannabinoids: Systematic Review Cannabinoid Control (Placebo or Active) Event rate (%) 70% 66% 59% 57% 57% 45% 43% 34% vs. Placebo Nausea vs. Active vs. Placebo vs. Active Vomiting active control= prochlorperazine, metoclopramide, chlorpromazine, thiethylperazine, haloperidol, domperidone, alzapride Tramèr MR, et al. BMJ. 2001;323:1-8. Complete Control of N/V with Cannabinoids Nausea NNT (95% CI) Versus placebo (4 studies) 8.0 (4.0-775) Versus active control (7 studies) 6.4 (4.0-16) Vomiting Versus placebo (4 studies) 3.3 (2.4-5.7) Versus active control (6 studies) 8.0 (4.5-38) 0.5 1.0 1.5 2.0 Relative risk (95% CI) Favors cannabinoids 2.5 NNT= number needed to treat; active control= prochlorperazine, metoclopramide, chlorpromazine, thiethylperazine, haloperidol, domperidone, alzapride. Tramèr MR, et al. BMJ. 2001;323:1-8 Patients’ Preference for Cannabinoids Preference for cannabinoids NNT (95% CI) Versus placebo (4 studies) 1.6 (1.4-1.8) Versus active control (14 studies) 2.8 (2.4-3.3) 0.5 1.0 2.0 4.0 6.0 8.0 Relative risk (95% CI) Favors cannabinoids 10.0 NNT = number needed to treat; active control= prochlorperazine, metoclopramide, chlorpromazine, thiethylperazine, haloperidol, domperidone, alzapride Tramèr MR, et al. BMJ. 2001;323:1-8. Cannabinoids in CINV Cannabinoids may be superior to conventional therapies in low-moderate emetogenic setting Patient preference for cannabinoids ranged from 38-90% (placebo 4-20%) Cannabinoids produced significantly more side effects (good & bad), more pt withdrawals “In selected patients, cannabinoids may be useful as mood enhancing adjuvants for the control of chemotherapy related sickness” Tramer et al, BMJ 2001 323:16-23 Cannabinoids in CINV 8-THC less psychotropic, less $, stable Less psychomimetic effects in children Phase II trial, 8 pts (3-13 yrs) Variety of cancers, chemotherapy Starting dose of 5 mg/m2 Nausea and vomiting eliminated No psychotropic effects seen Abrahamov et al, Life Sci 1995 56:2097 Experimental Emesis Linda Parker et al, Wilfred Laurier U. Series of studies with rats/shrews Model for anticipatory nausea THC or CBD >> ondansetron THC/CBD maybe most effective Limebeer and Parker Neuroreport 1999 Parker et al Neuroreport 2002 Parker et al Psychopharm 2004 Limebeer et al Physiol Behav 2006 Cannabinoids in CINV Several RCTs in chemotherapy-induced emesis (CINV) Pre 5-HT3 antagonist era (ondansetron) Oral or IM meds vs best treatment No comparison with 5-HT3 antagonist No controlled trials of inhaled marijuana Inhaled Marijuana Cross-over CINV study, placebo control, marijuana vs dronabinol n= 20 (15 men), 14 NSCLC 25% no vomiting, 15% no nausea 35% hallucinations or time perception changes Preference: 20% marijuana, 35% dronabinol, 45% no pref THC > marijuana therapeutic potency Levitt et al, JCO 1984 abstract C-354 Inhaled Marijuana CINV, open trial, no control n=74, chronic users, 25% dropped out Preference: 18 (34%) v effective, 26 (44%) mod effective 12 (22%) no benefit Side Effects: sedation 88%, dry mouth 77%, dizziness 39% 13% no A/E Vinciguerra et al, N Y State J Med 1988, 88:525 Special Situations Constipation Obstruction Symptom Prevalence Pain Fatigue/Asthenia Constipation Dyspnea Nausea Vomiting Delirium Depression/suffering 80 – 90+% 75 - 90% 70% 60+% 50 - 60% 30% 30 - 90% 40 - 60% Malignancy Direct effects obstruction by tumor in wall external compression by tumor neural damage L/S spinal cord cauda equina/pelvic plexus hypercalcemia Malignancy Secondary effects poor po intake dehydration weakness/inactivity confusion depression unfamiliar toilet arrangements Medications Opioids Ileocecal & anal sphincter tone Peristaltic activity (SI & C) Impaired defecation reflex sensitivity to distension internal anal sphincter tone Water, electrolyte absorption (SI & C) Concurrent Disease Diabetes Hypothyroidism Hypokalemia Hernia Anal fissure/stenosis Hemorrhoids Autonomic neuropathy diabetes spinal cord disease chemotherapy Parkinson’s disease ALS/MS Dementia Treatment Prophylaxis good symptom control activity adequate hydration recognize drug effect create a favorable environment Treatment: Laxatives >80% pts on opioids need laxatives Little research to guide choice Softener and stimulant best first choice May require oral/rectal routes Enemas useful in impaction Bulk forming agents worsen situation Treatment: Laxatives Surfactants: docusate Contact cathartics: senna, bisacodyl Osmotic laxatives: lactulose Saline osmotics: MgOH, Phosphasoda Enemas: oil, saline, soap suds, Fleet Other Approaches Prokinetic agents: domperidone, metoclopramide Antibiotics: erythromycin Herbal preparations: mulberry, rhubarb, licorice, prune juice New Agents Selective opioid antagonists Active in periphery, esp. gut Methylnaltrexone, Alvimopan Studies used IV and oral application S/E abd cramping, flatulence, nausea, dizziness Bowel Obstruction Common problem Associated with advanced cancers GI, ovarian, lymphoma Relapse / local spread of intrabdominal tumour Diffuse peritoneal carcinomatosis, encasement by tumour Multiple partial bowel occlusions (delaying or preventing propulsion of intestinal contents) Symptoms of nausea/vomiting abdominal pain, distention Pandha et al. Anti-Cancer Drugs, 1996; 7:5-10 Bowel Obstruction: Etiology Mechanical obstruction causes: secretions, gas proximal to the obstruction distention from gas, ingested fluids, digestive secretions in turn causes secretions secretion distention Mercadante et al. JPSM 1997 Bowel Obstruction Standard Therapy NG tube/IV fluids (“drip & suck”) Bowel rest Pain control (opioids) Radiological assessment Surgical intervention Bowel Obstruction Palliative Therapy Opioid analgesics, dexamethasone Promotility agents metoclopramide/domperidone Octreotide (Sandostatin) Hyoscine butylbromide (Buscopan) Somatostatin Analogues Octreotide, vapreotide, lanreotide Receptor activity brain, pituitary, pancreas, GI tract, immune cells Used in many conditions Prolongs GI transit time fluid secretion in jejunum water/electrolyte absorption decreases peristasis reduces GI blood flow Inhibits exocrine pancreatic secretion Bowel Obstruction in Ovarian Cancer 13 pts, advanced ovarian cancer, inoperable GI obstruction Octreotide dose of 300 - 600 µg/day Octreotide controlled vomiting in all cases Vomiting stopped in 2-3 days of starting tx Mangili et al., Gynecologic Oncology 1996 Bowel Obstruction in Ovarian Cancer NG drainage from 2000 to <100 ml/day Complete relief of symptoms within 3 days (range 1-6 days) 8/13 pts D/C from hospital, continued treatment at home Mangili et al., Gynecologic Oncology 1996 Delivery Routes for Medications Standard Oral Intravenous Inhalation (nebulized) Subcutaneous GH Alternative Sublingual transmucosal mouthwashes Intranasal Transdermal (topical) Rectal Vaginal Intraosseus Think “Outside the Box” Alternative Routes of Drug Administration Alternative delivery routes transmucosal transdermal (topical) rectal Review of the science Oral Mucosal Delivery Advantages: High vascular permeability Avoids “first pass” hepatic elimination High potency of drug (small volumes) Less intimidating/ “low-tech” administration easier in home, PCH, LTC Alternate administration route pt NPO, difficulty swallowing, SBO, etc. Oral Mucosal Delivery Barriers: Lipophilic Rx: needs intact mucosal cell membrane Hydrophilic Rx: poor absorption Volume of dose Ideally 0.5 ml; > 1-2 ml swallowed Excessive salvation swallowing of dose Acceptable delivery vehicle/taste Oral Mucosal Delivery Oral transmucosal drugs Lorazepam Olanzapine wafers (Zyprexa Zydis®) Proclorperazine buccal tabs (Stemetil®) Mirtazapine (Remeron® RD) Highly lipophilic better than oral absorption?? Oral Mucosal Delivery Haloperidol (Haldol®) Protect from light & freezing Store below 40ºC discoloration & grayishred precipitate Methotrimeprazine (Nozinan®) 25 mg/ml injectable (store room temp, protect from light) Topical Route Oral route not desirable Mucositis Inability to swallow Nausea/vomiting Obstruction Poor taste of product Dry mouth More localized action Topical Route: Advantages Avoids the GI tract and hepatic first-pass metabolism Delivers to a specific site Controls absorption rate Provides constant dosing depot effect with anhydrous gels Reduces systemic side effects Heir, Gary DMD, et al. IJPC 2004; 8:337-343 Topical Route: Advantages Improves compliance Allows ↑ concentration of Rx at site of application Plasma concentrations of <10% compared to oral route Heir, Gary DMD, et al. IJPC 2004; 8:337-343 Topical Route: Drawbacks Variations in the stratum corneum barrier Delivery dosing may require adjustment Rate of absorption may vary Rash most common SE Heir, Gary DMD, et al. IJPC 2004; 8:337-343 Topical Route Mouthwash/rinses Misoprostol, Diphenhydramine, Lidocaine, Triamcinolone, Sucralfate, Dry Mouth Formulations Transdermal Route Fentanyl, Oxybutinin, Estrogen, Nitrate patches Transdermal gels Buccal spray Morphine, Fentanyl, Triamcinolone, Lidocaine Medicated lollipops Fentanyl, Nicotine, Tetracaine, Dextromethorphan, Diphenyhydramine, Nystatin Topical Anti-Nauseant Gels Scopolamine 0.25mg/0.1ml Transderm V patch releases ~1mg over 72 hr ~0.1mg Q8H vs 0.25mg Apply 0.1 – 0.2ml Q8H Expiry date about 6 months Topical Anti-Nauseant Gels ABHR Ativan/Benadryl/Haldol/Reglan Lorazepam 2- 4 mg higher brain (cortex) Diphenhydramine 50-100 mg vestibular Haloperidol 2-4 mg CTZ Metoclopramide 40-80 mg/ml afferent impulses from periphery Dose 0.25ml inner wrist QID Moon RB Intl J Pharm Compound 2006 10:95-8 Subcut Antiemetics Haloperidol 0.5 - 1 mg po/sq/iv q4-12h MTMZ 5 - 10 mg po/sl/sq q4-8h Metoclopramide 10 - 20 mg po/sq/pr q4-8h Ondansetron 8 -16 mg q 12 h po/sq/iv Granisetron 1- 2 mg q 12 h po/sq Dexamethasone 4-16 mg po/sq/iv daily Dimenhydrinate 25 - 100 mg po/pr/sq q4-8h Scopolamine 0.3-0.6 mg sq Promethazine (Not sq) Case: Maria de J. 35 y o, mother of 3, works in textiles Lower abdominal pain, nausea Investigations reveal ovarian mass, resection: adenocarcinoma Chemo with platinum/paclitaxel, nausea with first 2 cycles, N/V subsequently Admitted for IV hydration, pt wants to stop tx gh Case: Maria de J. 4th cycle delayed x 1 week, P & S clinic Full assessment reveals anticipatory nausea, constipation on AXR Oral and PR laxatives given, BZD prechemo No vomiting, still nauseated, avoids po route Refuses hospital stay gh Case: Maria de J. Use of triple suppository advised (tid – qid) dexamethasone 2 mg metoclopramide 10 mg diphenhydramine 25 mg Nausea controlled for final 2 cycles, no hydration necessary Rectal Route Drug absorption Limiting factors Conditions/methods of administration Care Beyond Cure: A Pharmacotherapeutic Guide to Palliative Care; Andree Neron Editor, 2000 Rectal Drug Absorption First 6-8cm of rectum drain directly into systemic circulation Drugs admin by this route: no hepatic first-pass effect Rx high hepatic extraction may in bioavailability; variable due to: Patient Absorption site Drug formulation, penetration of mucosa Care Beyond Cure, 2000 Rectal Drug Absorption Rectum vs upper GI tract: Absorption area rectal mucosa: 200-400 cm² (no villi in rectum) small intestine: 2,000,000 cm² pH Fluid content Absorption mechanisms same (passive diffusion) Formulation of drug is critical factor May have to increase dosage interval i.e. Q8H vs Q12H Care Beyond Cure, 2000 Rectal Limiting Factors Drug insertion level 6-8cm (lower rectum) systemic circulation 15-20cm (upper rectum) portal vein hepatic first-pass effect Solutions: Aqueous & alcohol solutions are the best and most rapidly absorbed Fecal matter in rectum Defecation reflex, involuntary expulsion Care Beyond Cure, 2000 Rectal Administration Use liquid formulations whenever possible Use volumes <10-25 ml >80 ml ↑ risk of spontaneous expulsion Administer liquids with a small lubricated syringe Rectal canula or catheter tip syringes beneficial Cut a NG tube (#14) to 5 cm; attach to prefilled syringe reduces chance of portal vein absorption Care Beyond Cure, 2000 Rectal Administration Administer capsules and tablets directly into the rectum Compounding pharmacy: “designer” rectal suppositories Administration a lot easier Hepatic absorption usually not a problem with the use of suppositories Care Beyond Cure, 2000 Rectal Administration Lorazepam Use parenteral preps or tablets Bioavailability of injection > 80% Serum concentrations < ½ of IV route Metoclopramide Tablets or suspensions Phenobarbital Excellent bioavailability 90-100% Peaks at ~ 4 hours Baines, MJ BMJ 1997;315:1148-1150 Rectal Administration For refractory cases, use combinations that act at different receptor sites Cerebral cortex CTZ GI tract Severe or refractory nausea may benefit from corticosteroid Care Beyond Cure, 2000 Triple Suppository Metoclopramide 10 - 20mg Dimenhydrinate 25 - 75mg Prochloperazine 10 - 25mg Use a formulation with a single medication or combinations of up to 3 medications Other Antinauseant Suppositories Dimenhydrinate 75mg/Metoclopramide 15mg/Prochloperazine 10mg Dimenhydrinate 25mg/Metoclopramide 10mg/ Prochloperazine 15mg Metoclopramide 10mg/Haloperidol 1mg Dimenhydrinate 25mg/ Metoclopramide 20mg/ Prochloperazine 10mg/ Dexamethasone 2mg Summary GI symptoms in palliative care varied Assessment important Tailor therapy to meet pt needs Research in area lacking Help is available WRHA Pall Care pgm: 237-2400 Physician on call: 237-2053 (24 hrs) Case example Young woman, chronic pain Compression of C6 root, migraine, constant, rated 8/10 Attempted pain control using methadone, not tolerated Lost to F/U until Jan 07, returned on meperidine (Demerol®) Case example GP requested IV anti-nauseants Good effect but cumbersome Topical compound (/ml, in PLO): metoclopramide 20 mg dimenhydrinate 25 mg Benefit, but required adjustment to (/ml): dimenhydrinate 100 mg haloperidol 4 mg metoclopramide 80 mg
![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)