ISQUA Webinar_December 2013_Peter Carter
advertisement

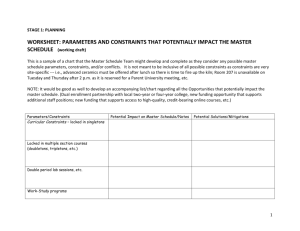
Physician Heal Thyself Peter Carter Chief Executive Officer International Society for Quality in Health Care Agenda Definitions Introduction Why Regulate (Self or Imposed) Scale of Challenges Case Studies The Beauty and the Beast of Self Regulation Big Brother (Imposed Regulation) Questions for you 2 Definitions Professional Self Regulation: the arrangement by which practitioners exercise authority and maintain control over the practice, self discipline, working conditions and professional affairs as they contribute to the mission of their organisation* Imposed Regulation: control governed by law and oversighted by some public official (judge, bureaucrat or legislator) Regulation by Private Parties e.g. Litigation- can be effective if on a large scale, as it has the power to punish the profession & thereby force changes in behaviour 3 * Aydelotte(1981) Choice Self Regulation OR Imposed Regulation OR WHAT??? Hybrid?? 4 Why Regulate Market Failure Public Interest Private Interest 5 Market Failure(Asymmetry of Information) Consumer less informed about nature & quality of service Relies on expertise of the professional Potential for supply induced demand So need… Protection of consumer through regulation 6 Public Interest Cartel like behaviour Control of supply to ↑prices 7 Private Interest Improve market equilibrium through efforts to promote greater and evenly distributed social welfare 8 The scale of the challenges 140,000+ different ways the human body can go wrong 6000+ medicines for treating diseases BNF ICD10 codes and we wonder why things go wrong…. 9 The scale of the challenges 1 in 10 patients admitted experience an adverse event Half of adverse events are judged to be preventable 5% of deaths in English acute hospitals had at least a 50% chance of being prevented Principal problems associated with preventable deaths poor clinical monitoring (31.3%), diagnostic errors (29.7%), and inadequate drug or fluid management (21.1%) Most preventable deaths (60%) occurred in elderly patients with multiple comorbidities and less than 1 year of life left 72% of all patient safety incidents are from the acute sector, 13% from Mental Health, 11% from Community, 2% from Learning Disability,10 0.6% from Community Pharmacy and 0.4% from General Practice. Case Study 1 Jayant Patel Who is Dr Patel Nature of his appointment Under the Radar Problems Emerge Inquiries Criminal Charges What went wrong Is there a bright side? ( Lessons learned) Questions 11 Case Study 1(Continued) 1. 2. 3. Would Self Regulation have prevented this (or similar episodes)? Did the existence of a self regulation regime prevent more effective regulatory practices being invoked? Is imposed regulation alone sufficient or is it likely to marginalise the profession? 12 Case Study 2 “The Beautiful Hospital” Chelsmford Hospital Harry Bailey 13 Chelmsford Private Hospital Facts Conducted Deep Sleep Therapy in the 1960s and 1970 Many patients died directly or indirectly as a result over many years Failures of Self Regulation and Imposed Regulation allowed this 14 Why? Self Regulation • Unresponsive • Lacked sanctions • Influenced by peer colleagues’ intimidation • Feared being sued Imposed Regulation • Unresponsive • Poor mechanisms • Was also intimidated And • Confusion between the professional body & the government regulator in connection to responsibilities 15 Statutory Protection Protection for quality assurance activities to encourage their use Disclosure of morbidity & mortality Information and the disclosure of information Disclosure in peer review meetings cannot result in legal action against health professionals This has the effect of making Self Regulation more effective & responsive 16 Key arguments for imposed regulation Information Asymmetry The professional services consumers’ gaps in knowledge Obligation to fill the consumers’ knowledge gaps 17 Hybrid The DoH(1997) stresses that in order to achieve the aims of clinical governance: i.e. control, responsibility, regulation, it expects individual health professionals to be more responsible for the own clinical practice and professional self regulation( individual and organisational).It must remain an essential element in the delivery of quality patient services 18 The Last Word goes to….. Professor Avedis Donabedian Systems awareness and systems design are important for health professionals, but they are not enough. They are enabling mechanisms only. It is the ethical dimensions of individuals that are essential to a system’s success. Ultimately, the secret of quality is love 19 Questions Would self regulation alone have presented the deaths & injuries in the two case studies? Would imposed regulation have done so? Both were present in both case studies - what went wrong? Is there a system/process that can ensure the public they will not be injured or killed by those in whom they put their trust? “All you need in Love” is Donabedian right? 20 Thank you Peter Carter pcarter@isqua.org 21