1 LocalAnestheticTechniques
advertisement

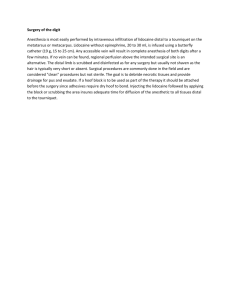
Local Anesthetic Techniques Prepared by Dr. Mahmoud Abdel-Khalek Jan 2015 Local Anesthetic Techniques Local Anesthetic Drugs Regional Anesthesia – Spinal Anesthesia – Epidural Anesthesia – Brachial Plexus Block – Bier’s Block Local Anesthetic Drugs Definition and Mode of Action LA are drugs that block the generation and propagation of impulses in excitable tissues: nerves, skeletal muscle, cardiac muscle, brain LA substances bind to a Na+ channel receptor on the cytosolic side of the Na+ channel (i.e. must be lipid soluble), inhibiting Na+ flux and thus blocking impulse conduction LA must convert to an ionized form to properly bind to receptor Different types of nerve fibres undergo blockade at different rates Mechanism of Action Un-ionized local anesthetic diffuses into nerve axon & the ionized form binds the receptors of the Na channel in the inactivated state Local Anesthetics Esters ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Procaine Chloroprocaine Tetratcaine Cocaine Metabolism ◦ Hydrolysis by pseudocholinesterase enzyme Amides Lidocaine Mepivacaine Bupivacaine Etidocaine Prilocaine Ropivacaine Metabolism ◦ Liver Local Anesthetics & Baracity Hyperbaric – Typically prepared by mixing local with dextrose – Flow is to most dependent area due to gravity Hypobaric – Prepared by mixing local with sterile water – Flow is to highest part of CSF column Isobaric – Neutral flow that can be manipulated by positioning – Very predictable spread – Increased dose has more effect on duration than dermatomal spread Absorption, Distribution, Metabolism LA readily crosses the blood-brain barrier (BBB) once absorbed into the blood stream Ester-type LA (procaine, tetracaine) broken down by plasma and hepatic esterases; metabolites excreted via kidneys Amide-type LA (lidocaine, bupivicaine) broken down by hepatic mixed function oxidases (P450 system); metabolites excreted via kidney Choice of LA depends on Onset of action –influenced by pKa (lower the pKa, the higher the concentration of the base form of the LA and the faster the onset of action) Duration of desired effects – influenced by protein binding (long duration of action when the protein binding of LA is strong) Potency – influenced by lipid solubility (agents with high lipid solubility will penetrate the nerve membrane more easily) Unique needs (e.g. sensory blockade with relative preservation of motor function, for pain management) Potential for toxicity Maximum Dose of LA Always be aware of the maximum dose for the particular LA used Maximum dose usually expressed as (mg of LA) per (kg of body weight) and as a total maximal dose (adjusted for young/elderly/ill) lidocaine maximum dose: 5 mg/kg (with epinephrine: 7mg/kg) chlorprocaine maximum dose: 11 mg/kg (with epinephrine: 14 mg/kg) Bupivacaine maximum dose: 2.5 mg/kg (with epinephrine: 3 mg/kg) Systemic Toxicity Occurs by accidental intravascular injection, LA overdose, or unexpectedly rapid absorption Systemic toxicity manifests itself mainly at CNS and CVS CNS effects first appear to be excitatory due to initial block of inhibitory fibres; subsequently, block of excitatory fibres CNS effects (in approximate order of appearance): Numbness of tongue Perioral tingling Disorientation Drowsiness Tinnitus Visual disturbances Muscle twitching Tremors Convulsions Seizures Generalized CNS depression Coma respiratory arrest Systemic Toxicity Treatment of LA systemic toxicity Use the A, B, C’s for the management of local anesthetic toxicity A= airway Maintain a patent airway, administer 100% oxygen B= breathing May need to be assisted with positive pressure ventilation or intubation C= circulation Check for a pulse If no pulse, initiate CPR Seizures Diazepam in doses of 5 mg, or alternatively sodium pentothal in doses of 50-200 mg will decrease or terminate seizures Treatment of LA systemic toxicity Hypotension: – Rapid infusion of IV fluids – Place the patient in a head down position (Trendelenburg) – Phenylephrine shots or infusion – Ephedrine (typically 5 mg shots) – If refractory treat the patient with epinephrine (5-10 mcg shots) – Repeat and escalate the dose as necessary The use of lipids in the treatment of local anesthetic toxicity has shown promise There are currently no established methods and research continues Neuraxial Blocks Anatomy The vertebrae are 33 number, divided by structural into five region: cervical 8, thoracic 12, lumber5, sacral 5, coccygeal3 Anatomy The vertebrae are joined together by strong anterior and posterior longitudinal ligaments Anatomy The spinal cord lies within the spinal canal surrounded by meninges; Dura mater, subarachnoid space, then pia matter, end by Cauda equina (Hoarse tail) The spinal cord receives blood supply from anterior and posterior spinal arteries Spinal cord extends to L2, Dural sac to S2 Nerve roots (Cauda equina) from L2 to S2 Needle inserted below L2 should not encounter cord, thus L3-L4 and L4-L5 interspace are commonly used for spinal anesthesia Spinal Meninges Dura Mater ◦ Outer most layer ◦ Fibrous Arachnoid ◦ Middle layer ◦ Non-vascular Sub Arachnoid Space ◦ Lies between the arachnoid and pia Pia ◦ Inner most layer ◦ Highly vascular CSF Indications of Spinal/ Epidural Full stomach Anatomic distortions of upper airway TURP surgery Obstetrical surgery (T4 Level for CS) To relieve post-operative pain Absolute Contraindications to Spinal/ Epidural Anesthesia Lack of proper equipment or properly trained personnel Patient refusal Lack of IV access Allergy to LA Infection at puncture site or underlying tissues Uncorrected hypovolemia Coagulation abnormalities Raised ICP Relative Contraindications to Spinal/ Epidural Anesthesia Bacteremia Preexisting neurological disease Aortic/mitral valve stenosis Previous spinal surgery Back problems Severe/unstable psychiatric disease or emotional instability (Uncooperative) Spinal Anesthesia Technique Preparation & Monitoring ◦ EKG ◦ NBP ◦ Pulse Oximeter Patient Positioning ◦ Lateral decubitus ◦ Sitting ◦ Prone (hypobaric technique) Spinal Anesthesia Technique Midline Approach – – – – – – – – Skin Subcutaneous tissue Supraspinous ligament Interspinous ligament Ligamentum flavum Epidural space Dura mater Arachnoid mater Paramedian or Lateral Approach – Same as midline excluding supraspinous & interspinous ligaments Spinal Anesthesia Levels Spinal Injection Sympathetic block is 2-6 dermatomes higher than sensory block Motor block is 2 dermatomes lower than sensory block Complications of Spinal Anesthesia Failed block Backache Hypotension, bradycardia if block reaches T2-T4 (sympathetic nervous system block) Post-spinal headache More common in women ages 13-40 Larger needle size increase severity (use G23 or smaller) Onset typically occurs first or second day post-op Treatment: Bed rest, Fluids, Caffeine, Blood patch Complications of Spinal Anesthesia Extensive spread of anesthetic ("high spinal") Persistent paresthesia (usually transient) Epidural or subarachnoid hematoma Spinal cord trauma Infection Complications of Spinal Anesthesia Failed block Back pain (most common) Spinal headache – – – – More common in women ages 13-40 Larger needle size increase severity Onset typically occurs first or second day post-op Treatment: Bed rest Fluids Caffeine Blood patch Blood Patch Effective treatment for postspinal headache Increase pressure of CSF by placing blood in epidural space If more than one puncture site, use lowest site due to rostral spread May be done more than one time 95% success with first patch Second patch may be done 24 hours after first Epidural Anesthesia Larger dose of LA used (1220 mL) LA deposited in epidural space (potential space between ligamentum flavum and dura) Widest at Level L2 (56mm)& Narrowest at Level C5 (1-1.5mm) Safest point of entry is midline lumbar Epidural Anesthesia Solutions injected spread in all directions of the potential space; SG of solution does not affect spread Initial blockade is at the spinal roots followed by some degree of spinal cord anesthesia as LA diffuses into the subarachnoid space through the dura Epidural Anesthesia Test Dose: 1.5% Lidocaine with Epinephrine 1:200,000 ◦ Tachycardia (increase >30bpm over resting HR) ◦ High blood pressure ◦ Light headedness ◦ Metallic taste in mouth ◦ Ring in ears ◦ Facial numbness ◦ Note: if beta blocked will only see increase in BP not HR Bolus Dose: Preferred Local of Choice ◦ 10 mL for labor pain ◦ 20-30 mL for C-section Epidural Anesthesia Distances from Skin to Epidural Space – Average adult: 4-6cm – Obese adult: up to 8cm – Thin adult: 3cm Assessment of Sensory Blockade – Alcohol swab Most sensitive initial indicator to assess loss of temperature – Pin prick Most accurate assessment of overall sensory block Complications of Epidural Anesthesia Inadvertent dural puncture Inadvertent IV administration Hypotension (nausea & vomiting) Headache Backache Infection Caudal Epidural Anesthesia Anatomy – Sacrum Triangular bone 5 fused sacral vertebrae Needle Insertion – Sacrococcygeal membrane – No subcutaneous bulge at site of injection after 2-3ml Caudal Epidural Anesthesia Dosages – S5-L2: 15-20ml – S5-T10: 25ml Post Operative Problems – Pain at injection site is most common – Slight risk of neurological complications – Risk of infection Brachial Plexus Block Musculocutaneous Nerve Median Nerve Ulnar Nerve Radial Nerve Axillary approach of BPB Advantages – Provides anesthesia for forearm & wrist – Fewer complications than a supraclavicular block Limitations – Not for shoulder or upper arm surgery – Musculocutaneous nerve lies outside of the sheath and must be blocked separately Complications – Intravascular injection – Elevated bleeding time increases risk for hematoma Axillary Approach Position – Head turned away from arm being blocked – Abduct to 90º – Forearm is flexed to 90º – Palpate axillary artery for pulse The needle is inserted adjacent to the artery Axillary Block Dosing – Lidocaine 1% 30-40ml – Etidocaine 1% 30-40ml – Bupivacaine 0.5% 30-40ml Note 40mL is most common vollume Local Intravenous Anesthesia (Bier’s Block) Suitable for upper limb below elbow& lower limb below knee surgeries Advantages: Easy to administer, rapid onset, muscle relaxation and rapid recovery Limitation Time! Ideal for procedures lasting 40-60 minutes Maximum time limit is 90 minutes Tourniquet pain generally starts after 20-30 minutes Contraindications Raynaud’s disease Sickle cell disease Crush injuries Young Children Must have a reliable/operative tourniquet! If this can not be guaranteed then this technique should not be used due to risk of toxicity! Mechanism of Action Not clearly understood Local anesthetics, ischemia, asphyxia, hypothermia, and acidosis all may play a role Equipment Operative and reliable double tourniquet Running IV in non-operative arm Resuscitation equipment Eschmarch bandage Local Anesthetic Choice 0.5% lidocaine or 0.5% prilocaine Max dose is 3 mg/kg for either NEVER USE EPINEPHRINE CONTAINING SOLUTIONS Complication of prilocaine is methemoglobinemia in doses of > 10 mg/kg Treat with 1-2 mg/kg of 1% methylene blue given over 5 minutes Technique IV catheter in operative arm as distally as possible Technique IV catheter in operative arm as distally as possible Double tourniquet on the operative arm Proximal Cuff Distal Cuff Technique Have patient hold arm up Use Eschmark bandage to exsanguinate the arm Exsanguinate the arm from distal to proximal Inflate the proximal tourniquet to 100 mmHg over the patients systolic pressure Proximal Cuff Distal Cuff Confirm the absence of a radial pulse Inject your local (0.5% lidocaine or prilocaine in a dose of 3 mg/kg) Remove IV catheter, hold pressure and have OR staff prepare arm Onset of anesthesia should occur in 5 minutes When the patient complains of pain you can inflate the distal tourniquet and then deflate the proximal tourniquet 2n Proximal Cuff d 1s Distal Cuff t Minimum time for tourniquet inflation The tourniquet should be up for at least 25 minutes…releasing it before this may result in toxicity Releasing the tourniquet in cyclic deflations (10 second intervals) will decrease peak levels of local anesthetic Complications Tourniquet discomfort Rapid return of sensation after tourniquet release and subsequent surgical pain Toxic reactions from malfunctioning tourniquets or deflating the tourniquet prior to the 25 minute limit Thank You