Open - The Scottish Government
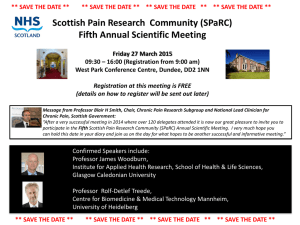
advertisement

MENTAL HEALTH (SCOTLAND) ACT 2015 - IMPLEMENTATION REFERENCE GROUP MEETING 1 MONDAY 14 DECEMBER 2015, 9:30AM - NOON, CONFERENCE ROOM 7-8, VICTORIA QUAY MINUTES Attendees Drew McFarlane (Chair) Nicola Paterson Eleanor Stanley Stephanie Virlogeux Annette Pyle Andrew Strong Trisha Hall Dr Joe Morrow Shaben Begum David Smith Charlene Tait Beth Hall Dr David Cumming Prof Lindsay Thomson Andrew Strachan Alison Robertson Chris Evans Karen Martin Linda Mitchell Scottish Government Scottish Government Scottish Government Scottish Government Scottish Government The ALLIANCE Scottish Association of Social Workers Mental Health Tribunal for Scotland Scottish Independent Advocacy Alliance Scottish Courts Service Scottish Autism CoSLA Royal College of Psychiatrists Forensic Network NHS Greater Glasgow and Clyde British Psychological Society VoX Carers Trust Scotland Scottish Commission for Learning Disability 1. Introductions Drew welcomed everyone to the first meeting of the Group. The aim of the meeting was to begin implementation of the Act – it is important that this draws on the detailed knowledge and different perspectives that members of the reference group have. 2. Remit and membership – paper 2 Drew introduced the remit paper. The focus of the group is on implementing the Act’s provisions. It will not look at other issues such as the review of learning disability etc as part of the mental health legislation that was a commitment made around the Bill. Papers will be placed on the Scottish Government website and therefore can be shared. There was a commitment to share papers at least a week in advance of meetings taking place. It was agreed that the remit should refer to the Government seeking views rather than advice. In relation to membership it was suggested that it should include an academic/MHO training representative (Pearce McCusker was suggested); a CAMHS representative; someone representing the needs of elderly patients; and include sufficient local authority representation. Actions: Beth to investigate a representative who could cover both local authority interests and the needs of elderly patients. Views on the need for a CAMHS representative would be welcome, together with who that could be. 3. Implementation timescales Nicola talked to the paper tabled at the meeting. There was support for the proposed timescales. It was noted that it was important to take a measured approach, to ensure that benefits for service users were fully realised and that excessive burdens were not placed on those who would operate the provisions on the ground. There would remain a need to estimate and refine estimates of resources needed to implement the Act and the timescale will be relevant to 2017/18 budgets. Dr Morrow provided an update on the operation of the new excessive security provisions. There had been around 2 applications a week mainly supported by RMO. It was noted that there could be impacts on demand for low-secure beds and that a short-term working group had been established by the Government to look at provision of beds more broadly. 4. Ways of working and Knowledge Hub Eleanor introduced and demonstrated the Knowledge Hub as a way to share information and have discussions between meetings, which it is proposed only take place at key points. It was felt that this approach will be key to broadening those that can be involved considering implementation matters. The Mental Health Law Team will be moderating the Hub and will draw up ground rules to ensure participants are comfortable sharing views. There needs to be an awareness, however, that individuals may be representing their own views rather than the views of organisations or networks and that needs to be clear. Action: Mental Health Law Team to draft rules for use of the Hub for the group’s views and provide invitation and joining details for members. Members can nominate people to join the Knowledge Hub to the Mental Health Law team. 5. Communications planning – paper 3 Eleanor introduced a communications planning paper. The group noted that structures are changing and therefore communications may be more complicated in the new integrated world, but having a single point of contact at an appropriate level in Health Boards and Integration Joint Boards could be a useful approach to the sharing of information. It was suggested that the Mental Health Law Team discuss communication contacts with the Mental Welfare Commission and Health and Social Integration team’s communication officer; liaise with Communications Directorate in SG; and that contact be made with Social Services Strategic Forum. In terms of sharing information there was a request from members for a common digest produced by the mental health law team that members can use with their own networks. Action: Mental Health Law Team to discuss communications with SG colleagues and produce common digest for members to use with their own networks. 6. Named persons – paper 4 Eleanor introduced the paper on named persons and the changes brought about in the Mental Health (Scotland) Act 2015. Provisions on named persons will feature significantly in the consultation paper early in the new year and Eleanor invited members to consider two key questions: How will the limited right of appeal work in practice? There was general agreement with the view that listed persons should have the status of relevant persons under the Tribunal rules giving a right of representation to the Tribunal but not a right to paperwork. The underlying principle is to retain appropriate participation but avoid providing information that the service user may not want the listed person to have. It was suggested that related paperwork be kept simple to ensure that practitioners have time for engagement with the affected persons. It was agreed that amendment to Tribunal Rules need to be clear about what is required but avoid the possibility of cases being thrown out due to purely technical matters. The definition of capacity is a relevant issue for decisions around listed persons. Consideration also needs to be given to issues around children and their carers, corporate parents and the named persons under the Children and Young Persons Act 2014, as default named persons are retained for those under 16. What transitional provisions are required? Eleanor talked through three options that had been identified. The group noted that any solution set out in the transitional provisions would have to factor in the resource implications, including difficulties of identifying which service users had named persons by default and which had chosen theirs. It was also important that it was not brought in in a way which gave the impression that people’s current rights were being taken away suddenly. There was agreement that it would be sensible to stagger the approach. There was general support for a suggested approach which would see : New Tribunal applications dealt with under the new arrangements. Existing named persons continuing until the next review of the order, when the service user would then choose whether to continue to have a named person. Service users also being able to say they no longer want a named person at any point after the implementation date. In discussion it was noted that there was an enormous information component to the changes to named persons and a change to the ethos of practitioners who up to now have been focussed on there being a named person. It will be important that there is clear information for service users and carers about the new roles. This should include consideration of what best practice guidance would be useful in the Code of Practice in relation to the discussions that should be had with service users and carers about deciding whether to have a named person or a listed person . There is a need therefore for education and training. Ensuring those that provide advocacy, in particular, have the information they need to have useful discussions with patients will be key. In addition, consideration of supported decision making should underpin the development of the policy on named persons. 7. Further policy papers: i. Conflict of interest regulations – paper 5 Eleanor referred to the existing conflict of interest regulations and the changes brought about by the Act. The proposal for the group’s view was to largely replicate existing arrangements. Comments in writing prior to the meeting had noted that the need to ensure that the regulations allow for situations where NHS consultants are requested to provide a second opinion, attracting a fee. It was suggested that the regulations need to retain permissible conflicts to ensure the arrangements are workable. It was noted that the regulations could increase burdens on NHS practitioners, as they would become responsible for conducting the medical examination for mandatory review of CTO, COs and COROs. It was noted that this could bring helpful NHS scrutiny to the process. There was a suggestion that there needs to be discussions with practitioners in rural areas such as Highland and Grampian as getting alternative doctors can be harder. It was also agreed it was worth exploring whether reference should be made to doctors in different management structures rather than hospitals, particularly for larger hospitals where there can be several mental health services within the same hospital. Action: Mental Health Law Team to make contact with Highland practitioners. ii. Safeguards for certain informal patient regulations – paper 6 Eleanor informed the Group that this issue was raised by the Mental Welfare Commission and invited comments. The general view was that arrangements for artificial nutrition should be the same as for ECT but there was a need to avoid creating a barrier to commencing treatment, where necessary and appropriate, as artificial nutrition is usually urgent life-saving treatment. Consideration has to be given to interaction with children’s legislation. iii. Advance statements – paper 7 Eleanor invited commented on transitional arrangements around advance statements and what should be reflected in the code of practice. The Mental Welfare Commission are taking forward a project on advance statements and this should help share best practice, such as the peer support work taking place in Glasgow. Members requested that there be clarity about what needs to be provided so that structures can be put in place to provide what is required – would welcome clarity and simplicity around the information that Health Boards will be required to provide around publicising support for making advance statements. iv. v. Communications at medical examination – paper 8 Services and accommodation for mothers – paper 9 There was insufficient time to discuss papers 8 and 9. The questions in them will be set out in Knowledge Hub and members were invited to consider after the meeting. Action: Members to join Knowledge Hub and provide their views on questions placed on the site. Meeting dates will be issued for 2016-17. The meeting drew to a close. Mental Health Law Team 14 December 2015