Enter your project title here
advertisement

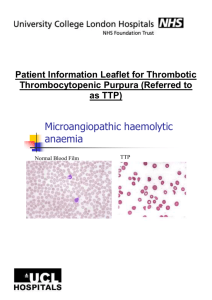
Charles L. Bennett MD PhD MPP Limited size of clinical trials Undetected toxicities at time of FDA approval Many AEs identified after several years on the market Hampton, T. Postmarket “Pharmacovigilance” Program on Alert for Adverse Events from Drugs. JAMA, August 22/29 2007, 298 (8): 851-2. Academic Organizations FDA Pharmaceutical Manufacturers Data Case assessments; Prospective data MedWatch Proprietary databases Science Pathology; histology None None Timeliness 1-2 years post approval 3 years or more 7-12 years Dissemination Manuscripts; presentations Package inserts Dear Doctor letters Network Broad; international Mostly internal Mostly internal Funding R01-based; CERTs Internal Not known Detect ADR signals Investigate possible ADR occurrence Analyze data Disseminate results Bennett CL, Nebeker JR, Lyons EA, et al. The Research on Adverse Drug Events and Reports (RADAR) Project. JAMA 2005, 293:17, 2131-40. Drug ADR N Publication Bisphosphonates Osteonecrosis of the Jaw Review of case series Lancet Oncology 2008 Epoetin/ darbepoetin VTE and Mortality Metaanalysis JAMA 2008 Sirolimus/paclitaxel coated cardiac stents Thrombotic events 139 JAMA 2007 G-CSF/ GM-CSF Acute myeloid leukemia and myelodisplastic syndrome 16 J Natl Cancer Inst 2007 Epoetin/ darbepoetin Venous thromboembolism Metaanalysis J Natl Cancer Inst 2006 Sirolimus/paclitaxel coated cardiac stents Hypersensitivity reactions 6 J Am Coll Cardiol 2006 Thalidomide/ lenalidomide Venous thromboembolism Metaanalysis JAMA 2006 Epoetin Pure Red-Cell Aplasia 9 N Engl J Med 2004 Clopidogrel Thrombotic thrombocytopenic purpura 13 N Engl J Med 2000 Ticlopidine Thrombotic thrombocytopenic purpura 21 Lancet 1998 Mortality and Venous Thromboembolism Associated with Erythropoiesis Stimulating Agents (ESAs) Bennett CL, et al. Venous thromboembolism and mortality associated with recombinant erythropoietin and darbepoetin administration for the treatment of cancer-associated anemia. J Amer Med, 2008; 299(8):914-924. Mortality Meta-analysis Meta-analysis of mortality rates for 51 phase III oncology trials with 13,613 patients for ESAs versus placebo or control HR= 1.10 (1.01, 1.20) Study ID HR(mortality) (95% CI) % Weight AOC Ables_1993 Smith_2003 Charu_2004 Mystakidou_2005 Gordon_2006 Amgen 200010103_2007 Subtotal (I-squared = 0.0%, p = 0.536) 0.89 (0.41, 1.93) 3.96 (0.29, 54.12) 1.38 (0.44, 4.33) 0.50 (0.05, 4.99) 0.67 (0.23, 2.00) 1.43 (1.06, 1.92) 1.29 (1.00, 1.67) 1.13 0.11 0.54 0.14 0.60 5.19 7.72 TRA Case_1993 Rose_1994 Cazzola_1995 Henry_1995 Osterborg_1996 Del Mastro_1997 Oberhoff_1998 Ten Bokkel_1998 Dunphy_1999 Thatcher a_1999 Thatcher b_1999 Throuvalas_2000 Coiffier_2001 Dammacco_2001 Littlewood_2001 Vansteenkiste_2002 Bamias_2003 Hedenus_2003 Henke_2003 Kotasek_2003 EPO-CAN-15_2004 EPO-GBR-7_2004 INT-1_2004 INT-3_2004 Machtay_2004 (RTOG99-03) N93-004_2004 (Grote) P-174-2004 Razzouk_2004 Savonije_2004 Vadhan-Raj_2004 (PR0003-006) DA 232_2005 (Taylor) Leyland-Jones_2005 (INT-76) O'Shaughnessy_2005 Osterborg_2005 STRAUSS_2005 Witzig_2005 WILKINSON_2006 BLOHMER_2007 (AGO/NOGG) Chang_2007 (EPO-CAN-17) DA 145_2007 DAHANCA-10-2007 EPO-GER22-2007 GOG-191_2007 MOEBUS_2007 PREPARE-2007 Wright_2007 (EPO-CAN-20) Subtotal (I-squared = 21.1%, p = 0.108) 1.08 (0.44, 2.66) 1.68 (0.66, 4.29) 0.37 (0.06, 2.27) 0.75 (0.28, 2.01) 1.02 (0.51, 2.04) 0.36 (0.05, 2.56) 0.61 (0.24, 1.55) 1.01 (0.19, 5.31) 0.14 (0.00, 6.88) 0.49 (0.03, 8.71) 1.26 (0.24, 6.60) 0.13 (0.00, 332.66) 1.02 (0.38, 2.73) 0.32 (0.11, 0.95) 0.81 (0.62, 1.06) 0.78 (0.60, 1.01) 1.80 (0.53, 6.12) 1.36 (0.98, 1.89) 1.39 (1.05, 1.84) 0.55 (0.11, 2.71) 2.70 (1.17, 6.23) 1.07 (0.73, 1.57) 1.58 (0.32, 7.82) 1.56 (0.42, 5.79) 1.41 (0.80, 2.49) 1.53 (0.65, 3.61) 0.41 (0.03, 5.76) 0.98 (0.14, 6.90) 0.98 (0.36, 2.67) 0.15 (0.00, 415.90) 0.85 (0.45, 1.60) 1.37 (1.07, 1.75) 7.39 (0.15, 366.10) 1.04 (0.80, 1.35) 1.16 (0.69, 1.95) 1.09 (0.83, 1.43) 4.54 (0.40, 51.20) 0.67 (0.34, 1.33) 0.88 (0.49, 1.59) 0.93 (0.82, 1.05) 1.28 (0.97, 1.69) 1.02 (0.60, 1.74) 1.25 (0.65, 2.41) 1.14 (0.77, 1.69) 1.50 (0.96, 2.34) 1.84 (1.01, 3.35) 1.09 (0.99, 1.19) 0.86 0.80 0.22 0.72 1.38 0.19 0.80 0.26 0.05 0.09 0.27 0.01 0.73 0.59 5.82 6.01 0.48 4.54 5.53 0.29 0.99 3.67 0.28 0.42 1.97 0.94 0.11 0.19 0.70 0.01 1.64 6.39 0.05 5.91 2.28 5.74 0.13 1.43 1.85 10.44 5.59 2.17 1.54 3.50 2.92 1.79 92.28 Heterogeneity between groups: p = 0.133 Overall (I-squared = 19.5%, p = 0.114) 1.10 (1.01, 1.20) 100.00 NOTE: Weights are from random effects analysis 5.1e-05 1 ESA better 19684 Control better Updated Mortality Meta-analysis Meta-analysis of mortality rates for 53 oncology trials with 14,164 patients for ESAs versus placebo or control (updated to include BRAVE study) HR= 1.09 (95% CI, 1.01-1.18) Study ID HR(mortality) (95% CI) % Weight AOC Mystakidou_2005 Gordon_2006 Ables_1993 Glaspy_2007 (Amgen 200010103) Charu_2007 Smith_2003 Subtotal (I-squared = 0.0%, p = 0.686) 0.51 (0.05, 4.99) 0.67 (0.23, 2.00) 0.89 (0.41, 1.93) 1.22 (1.03, 1.45) 1.38 (0.44, 4.33) 3.96 (0.29, 54.12) 1.19 (1.01, 1.40) 0.11 0.46 0.88 8.23 0.42 0.08 10.18 TRA Throuvalas_2000 Dunphy_1999 Vadhan-Raj_2004 (PR0003-006) Dammacco_2001 Del Mastro_1997 Cazzola_1995 P-174_2004 Thatcher_1999a Kotasek_2003 Oberhoff_1998 Blohmer_2007 (AGO/NOGG) Henry_1995 Vansteenkiste_2002 Littlewood_2001 Rosen_2003(phase II RCT) DA 232_2005 (Taylor) Chang_2007 (EPO-CAN-17) DA 145_2007 Razzouk_2004 EPO-GBR-7_2004 Osterborg_1996 Coiffier_2001 Debus_2007 (EPO-GER22) Osterborg_2005 ten Bokkel Huinink_1998 (Reed_2005) Aapro_2008 (BRAVE) Case_1993 Witzig_2005 Moebus_2007 Savonije_2005 Strauss_2005 Thatcher_1999b DAHANCA-10_2007 Hedenus_2003 Leyland-Jones_2005 (INT-76) Henke_2003 Machtay_2004 (RTOG99-03) PREPARE_2007 N93-004_2004 (Grote) INT-3_2004 INT-1_2004 Rose_1994 Thomas(GOG-191_2007) Bamias_2003 Wright_2007 (EPO-CAN-20) EPO-CAN-15_2004 Wilkinson_2006 O'Shaughnessy_2005 Subtotal (I-squared = 20.4%, p = 0.111) 0.13 (0.00, 332.66) 0.14 (0.00, 6.88) 0.15 (0.00, 415.90) 0.32 (0.11, 0.95) 0.36 (0.05, 2.56) 0.37 (0.06, 2.27) 0.41 (0.03, 5.76) 0.49 (0.03, 8.71) 0.55 (0.11, 2.71) 0.61 (0.24, 1.55) 0.67 (0.34, 1.33) 0.75 (0.28, 2.01) 0.78 (0.60, 1.01) 0.81 (0.62, 1.06) 0.84 (0.45, 1.55) 0.85 (0.45, 1.60) 0.88 (0.49, 1.59) 0.93 (0.82, 1.05) 0.98 (0.14, 6.90) 0.98 (0.62, 1.56) 1.02 (0.51, 2.04) 1.02 (0.38, 2.73) 1.02 (0.60, 1.74) 1.04 (0.80, 1.35) 1.06 (0.20, 5.53) 1.07 (0.87, 1.32) 1.08 (0.44, 2.66) 1.09 (0.83, 1.43) 1.14 (0.77, 1.69) 1.15 (0.87, 1.53) 1.16 (0.69, 1.95) 1.26 (0.24, 6.60) 1.28 (0.97, 1.69) 1.36 (0.98, 1.89) 1.37 (1.07, 1.75) 1.39 (1.05, 1.84) 1.41 (0.80, 2.49) 1.50 (0.96, 2.34) 1.53 (0.65, 3.61) 1.56 (0.42, 5.79) 1.58 (0.32, 7.82) 1.68 (0.66, 4.29) 1.69 (0.76, 3.75) 1.80 (0.53, 6.12) 1.84 (1.01, 3.35) 2.70 (1.17, 6.23) 4.54 (0.40, 51.20) 7.39 (0.15, 366.10) 1.09 (1.00, 1.18) 0.01 0.04 0.01 0.45 0.15 0.17 0.08 0.07 0.22 0.62 1.12 0.56 5.27 5.08 1.35 1.29 1.47 10.32 0.15 2.22 1.08 0.56 1.73 5.16 0.20 6.69 0.66 5.00 2.88 4.71 1.83 0.20 4.85 3.84 5.65 4.79 1.56 2.38 0.73 0.32 0.22 0.62 0.84 0.37 1.42 0.77 0.10 0.04 89.82 Heterogeneity between groups: p = 0.186 Overall (I-squared = 17.1%, p = 0.145) 1.09 (1.01, 1.18) 100.00 NOTE: Weights are from random effects analysis VTE Meta-analysis Meta-analysis of VTE rates in 38 phase III trials with 8,172 patients for ESAs versus placebo or control HR= 1.57 (1.31,1.87) Study ID RR (95% CI) % Weight Bamias_2003 Smith_2003 Case_1993 Henry_1995 Wright_2007 (EPO-CAN-20) N93-004_2004 (Grote) Chang_2007 (EPO-CAN-17) Littlewood_2001 Vansteenkiste_2002 INT-1_2004 Leyland-Jones_2005 (INT-76) Witzig_2005 Osterborg_1996b DA 145_2007 Henke_2003 Ten Bokkel_1998a EPO-GER22_2007 Charu_2007 Rose_1994 Thatcher1999b Osterborg_1996a Abels_1993 Throuvalas_2000 GOG-191_2007 Italian_1998 Razzouk_2004 Welch_1995 Osterborg_2005 Gordon_2006 Ten Bokkel_1998b Vadhan-Raj_2004 (PR0003-006) INT-3_2004 Wilkinson_2006 Savonije_2004 Machtay_2004 (RTOG99-03) EPO-GBR-7_2004 Dammacco_2001 EPO-CAN-15_2004 Rosenzweig_2004 Cascinu_1994 P-174_2004 Thatcher_1999a Overall (I-squared = 0.0%, p = 0.901) 0.33 (0.01, 8.05) 0.34 (0.02, 5.27) 0.63 (0.11, 3.64) 0.73 (0.27, 1.98) 0.75 (0.13, 4.20) 0.97 (0.60, 1.59) 1.36 (0.70, 2.62) 1.38 (0.51, 3.75) 1.44 (0.47, 4.43) 1.46 (0.15, 13.85) 1.47 (0.89, 2.40) 1.47 (0.54, 4.05) 1.53 (0.06, 36.23) 1.53 (1.08, 2.18) 1.58 (0.59, 4.26) 1.96 (0.10, 38.79) 1.98 (0.97, 4.03) 2.36 (0.13, 43.20) 2.50 (0.55, 11.30) 2.56 (0.13, 51.05) 2.71 (0.14, 54.32) 2.73 (0.11, 65.68) 2.79 (0.12, 65.66) 2.84 (0.81, 9.96) 2.93 (0.12, 70.08) 2.95 (0.61, 14.28) 3.00 (0.13, 68.26) 3.05 (0.13, 74.41) 3.15 (0.17, 57.55) 3.56 (0.20, 62.58) 3.74 (0.85, 16.56) 3.85 (0.49, 30.15) 4.09 (0.54, 30.80) 4.44 (0.57, 34.55) 4.93 (0.24, 100.89) 4.93 (0.58, 41.73) 5.51 (0.66, 45.98) 8.00 (1.93, 33.09) 8.40 (0.50, 142.27) . (., .) . (., .) . (., .) 1.57 (1.31, 1.87) 0.31 0.42 1.01 3.13 1.06 13.16 7.27 3.16 2.48 0.62 12.93 3.08 0.31 25.84 3.21 0.35 6.23 0.37 1.38 0.35 0.35 0.31 0.32 2.00 0.31 1.26 0.32 0.31 0.37 0.38 1.42 0.74 0.77 0.75 0.35 0.69 0.70 1.56 0.39 0.00 0.00 0.00 100.00 NOTE: Weights are from random effects analysis .1 .2 ESA better .5 1 2 5 10 20 50 Control better Bohlius et al, J Clin Onc 2006 Wilson et al, Health Tech 2007 Seidenfeld et al, BCBS 2006 Bennett et al, JAMA 2008 Bohlius et al, Lancet 2009 No. of trials (No. of patients) 42 (8,167) 28 (5,308) 35 (6,918) 51 (13,611) 53 (13,933) HR for mortality (95% CI) 1.08 (0.99-1.18) 1.03 (0.92-1.16) 1.11 (0.99-1.23) 1.10 (1.01-1.20) 1.17 (1.06-1.30) KDOQI 2007 guideline (non-dialysis patients) KDOQI 2007 guideline (dialysis patients) Phrommintikul 2007 RADAR report (unpublished) No. of trials (No. of patients) 8 (3,038) 4 (2,391) 9 (5,143) 3 (3,300) HR for mortality (95% CI) 1.01 (0.63,1.61) 1.12 (0.91,1.37) 1.17 (1.01, 1.35) 1.25 (1.071.45) Conflicts of Interest in Basic Science Studies: Evaluating Erythropoietin Effects of Solid Tumor Cell Lines Bennett CL, et al. Association between pharmaceutical support and basic science research on erythropoiesis-stimulating agents. Arch Intern Med, 2009; 170(16): 1490-1498. • Senator Charles Grassley (R-IA) recently initiated conflict of interest probes against physicians at Harvard Medical School, Columbia University, and Emory University. • Physician Payments Sunshine Act: requires transparency in relationships between physicians and pharmaceutical companies. • Clinical studies have demonstrated that when investigators have financial relationships with pharmaceutical manufacturers, they are less likely to criticize the safety, efficacy, or costeffectiveness of agents supplied by the manufacturers. • No study has evaluated the effects of these financial relationships in the basic science setting. We investigated the relationship between manufacturer involvement and laboratory results in studies of erythropoietin receptors (EpoRs) in cancer cells. Erythropoietin Stimulating Agents (ESAs) • ESAs were approved in 1993 for use in the treatment of chemotherapy-associated anemia. • Concerns were raised that the off-target effects might include stimulation of erythropoietin receptors (EpoRs) on cancer cells. • Early adverse clinical evidence for ESA use: - BEST 2003 (breast cancer) - ENHANCE 2003 (head and neck cancer) • A MEDLINE database search was conducted (1988-June 2008). • Studies investigating EpoR presence and ESA-induced signaling and/or changes in cellular function, in solid tumors, were evaluated. • Conflicts of interest, laboratory results, funding sources, and affiliations were extracted. • Academic studies without funding from ESA manufacturers; n=64 • Studies led by academic investigators who had received funding from ESA manufacturers; n=7 • Investigators employed by ESA manufacturers; n=3 Gene Protein Signal transduction Function / Activity Erythropoietin Receptors in Solid Tumors: Gene Level Gene Protein Signal transduction Function / Activity • EpoR mRNA is detected in a wide variety of solid tumors. • Studies have demonstrated an increase in EpoR mRNA levels upon stimulation with Epo. Erythropoietin Receptors in Solid Tumors: Protein Level Gene Protein Signal transduction Function / Activity • Cell surface expression of EpoR in solid tumors detected by immunohistochemistry, immunocytochemistry, immunoblot, etc. Erythropoietin Receptors in Solid Tumors: Signaling Gene • EpoR stimulation by Epo induces the phosphorylation of signaling proteins involved in critical pathways regulating cell growth, apoptosis and angiogenesis. • Signal transduction is detected in the PI3KAKT, JAK-STAT and/or NF-kB pathways and varies among tumor types. Protein Signal transduction Function / Activity Erythropoietin Receptors in Solid Tumors: Cellular Function and Activity Gene Protein Signal transduction • Function / Activity Activation of the Epo/EpoR-signaling axis by Epo administration results in changes in proliferation, apoptosis, invasion, and chemosensitivity. Percent of Studies Identifying Conclusion (%) No COI Academics with COIs Investigators employed by ESA manufacturers 100 80 60 p= 0.009 p= 0.001 40 20 0 Presence of the EpoR Erythropoietin-Induced Signaling Events Conclusion Identified Erythropoietin-Induced Changes in Cellular Function p= 0.007 Percent of Studies Identifying Conclusion (%) 70 NO COI Academics with COIs Investigators employed by ESA manufacturers 60 50 40 p= 0.008 30 20 10 0 Qualitative Conclusions “ESAs Harmful” Qualitative Conclusions “ESAs Beneficial” Conclusion Indentified p< 0.04 No COI Percent of Presenters Identifying Conclusions (%) 100 Investigators employed by ESA manufacturers 80 60 40 p<0.01 p<0.04 p<0.01 20 0 EpoR Presence Erythropoietin-Induced Signaling Events Conclusions Identified Erythropoietin-Induced Changes in Cellular function Association between pharmaceutical support and basic science research findings on ESAs: Comparison of findings before and after an NCI workshop on this subject was convened Prior study evaluated associations between pharmaceuticalindustry funding and preclinical research Study of erythropoiesis stimulating agents (ESAs) found academic researchers without industry support were more likely than others to identify detrimental effects of ESAs on tumor cells Concurrently, a meta-analysis identified mortality risks when cancer patients received ESAs 2007 - the National Cancer Institute convened a workshop reviewing research of preclinical effects of ESAs on tumor growth We updated our analyses of associations between funding source and ESA research findings following the workshop Articles identified in MEDLINE and EMBASE databases (2008-2012) investigating preclinical findings for ESAs in the cancer setting were reviewed. Possible outcomes: ◦ ◦ ◦ ◦ EPO receptor detection Signaling events Cellular function Qualitative conclusions Outcomes were reported for the current and the earlier time-period according to funding source ◦ investigators without ESA manufacturer funding [27 and 64 studies, respectively] ◦ investigators with funding from manufacturers or who held an ESA patent [5 and 7 studies, respectively] ◦ investigators employed by ESA manufacturers [2 and 3 studies, respectively] EpoR(s), Epo Receptor(s), OR Erythropoietin Receptor(s) + Cancer, Tumor, Malignancy, OR Carcinoma Performed all combinations and used the search with most results 280 Total Articles 29 Included Articles Erythropoietin Receptor + Cancer For each of the tumor types identified in the above searches, additional searches were run with “tumor type” + “EpoR” variant: EpoR(s) AN D Erythropoietin Receptor(s) Breast Lung Prostate Cervical Endometrial Ovarian Glioma Head and Neck Neuroblastoma Renal Pancreatic Melanoma Mesothelioma Colorectal Colon Ewing’s Sarcoma Family of Tumors The first and last author of each previous article were searched for more recent publications 280 Total Articles 251 Articles were excluded: • Hematologic malignancies • Single case reports • Investigators employed contrived systems • Investigation did not involve cancer • Experiments involved tumor types for which evidence of changes in signaling upon Epo administration was not investigated in the literature • Article was a review 33 Total Articles Erythropoietin + First OR Last Author (from prior study) 4 Included Articles Effect of Impact Factor (</> 4) on Studies 120 100 Percent of Studies 80 60 0-4.00 4.0+ 40 20 0 Academic Investigators without conflicts of interest Investigative teams comprised primarily of Investigative teams comprised primarily of ESA academic investigators, one or more authors has a manufacturer employees conflict of interest Academic Investigators without conflicts of interest: 16/24 and 8/24, respectively Investigative teams comprised of primarily academic investigators, one or more authors has a conflict of interest: 0/3 and 3/3, respectively Investigative teams comprised primarily of ESA manufacturer employees: 1/2 and 1/2, respectively Percent of New Studies Identifying Varying Conclusion 120 100 80 60 40 20 0 Presence of the EpoR Erythropoietin-Induced Signaling Events Erythropoietin-Induced Changes in Cellular Function Qualitative Conclusions *ESAs Harmful* Qualitative Conclusions *ESAs Beneficial* Academic Investigators without conflicts of interest Investigative teams comprised primarily of academic investigators, one or more authors has a conflict of interest Investigative teams comprised primarily of ESA manufacturer employees Presence of the EpoR: 25/26, 5/5, and 2/2, respectively Erythropoietin-induced signaling events: 19/22, 2/2, and 0/2, respectively Erythropoietin-induced chances in cellular function: 19/22, 2/3, and 0/2, respectively Qualitative conclusions that ESAs were harmful: 20/26, 2/5, and 0/2, respectively Qualitative conclusions that ESAs were beneficial: 0/26, 0/5, and 0/2, respectively Qualitative conclusions that ESAs were neutral/no statement: 6/26, 3/5, and 2/2 respectively Qualitative Conclusions *ESAs Neutral/No Statement* Academic Investigators without conflicts of interest Investigative teams comprised primarily of academic investigators, one or more authors has a conflict of interest Investigative teams comprised primarily of ESA manufacturer employees Percent of Studies Identifying Conclusion (%) 120 100 80 60 40 20 0 Presence of the EpoR Erythropoietin-Induced Signaling Events Erythropoietin-Induced Changes Qualitative Conclusions *ESAs Qualitative Conclusions *ESAs in Cellular Function Harmful* Beneficial* Conclusion Identified Presence of the EpoR: 82/83, 8/10, and 3/5, respectively Erythropoietin-induced signaling events: 50/55, 2/4, and 0/3, respectively Erythropoietin-induced chances in cellular function: 49/61, 2/9, and 0/3, respectively Qualitative conclusions that ESAs were harmful: 44/91, 2/12, and 0/5, respectively Qualitative conclusions that ESAs were beneficial: 6/91, 3/12, and 0/5, respectively Academic researchers with or without financial conflicts increasingly report detrimental effects of ESAs. Concerns over potential financial conflicts of interest affecting basic science research are less apparent in academic versus pharmaceutical-owned laboratories. • Antibody specificity • Choice of controls; proprietary versus nonproprietary carrier protein • Differences in biological threshold for identifying changes in cellular function of erythropoietinexposed cancer cells In these basic science studies, pharmaceutical sponsorship is associated with a decreased likelihood of identifying: Presence of EpoR on solid cancer cell lines Unfavorable signaling events upon ESA administration Unfavorable changes in cellular function upon ESA administration • These findings are counter to the belief that basic science studies are not subject to variable interpretation. • The observed relationship may extend to other basic science research studies. • Only further analyses can confirm or deny these preliminary findings, but the implications are significant and additional studies in this area are warranted. Rituximab-associated Progressive multifocal leukoencephalopathy (PML) Carson KR, Bennett CL, et al. Progressive multifocal leukoencephalopathy after rituximab therapy in HIV-negative patients: a report of 57 cases from the Research on Adverse Drug Events and Reports project. Blood, 2009; 113(20). 4834-4840. Etiology JC polyomavirus infection >80% of cases seen in patients with HIV Latent JC virus in up to 80% of population Reactivation of JC virus not well understood Non-HIV PML Hematologic malignancy B-cell lymphoproliferative disorders Possible association with stem cell transplant and purine analog therapy Chronic inflammatory diseases, solid organ transplant, sarcoidosis, advanced age June 2004 Warning about Hepatitis B reactivation added to package insert February 2006 Warning about other viral infections added to package insert December 2006 Letter to health professionals from manufacturer and FDA warning: PML seen in two patients with lupus February 2007 Black box warning added to package insert Cases were identified among rituximab-treated patients by clinicians from 12 cancer centers or academic hospitals (22 cases) or by reviewing FDA reports (11 cases), the manufacturer’s database (30 cases), and publications (18 cases; MeSH search terms: leukoencephalopathy, rituximab, immunosuppressed, lymphoma, and leukemia) Unique data sources Clinical observation (n=7) Medical literature (n=14) FDA MEDWatch (n=14) Manufacturer (n= 23) Inclusion criteria: Rituximab treatment AND Brain biopsy confirmation of PML OR Autopsy confirmation OR MRI evidence AND JC virus in CSF by PCR Exclusion Diagnosis of HIV 15 excluded for inadequate evidence of PML, 2 for diagnosis of HIV Patient Information (n=57) Median Age (Years) 61 (range 30-89) Sex (%) M: 48.3 F: 56.2 Median Doses Rituximab 6 (range 1-28) Purine Analogue 26 patients Stem Cell Transplant 6 (4 Auto, 2 Allo) Carson, Blood 2009 Median time course (All patients, n=57) 1st rituximab to PML 16 months (range 1.0-90.0) Last rituximab to PML 5.5 months (range 0.3-66.0) PML diagnosis to death 2.0 months (0.4-122) Previous and concomitant chemotherapy treatments (range) 4 (1-14) Carson, Blood 2009 Mental status changes or confusion Focal motor weakness Loss of coordination Difficulty speaking Vision changes Carson, Blood 2009 54.4% 33.3% 24.6% 21.2% 17.5% Carson, Lancet Oncology 2009 (In press) T- Lymphocyte Selective adhesion molecule inhibitors LFA-1 Mucin VLA-4 BLOOD FLOW Selectins VCAM-1 ICAM-1 Endothelial Basal lamina BRAIN TISSUE Molecules not to scale. Carson, Lancet Oncology 2009 (In press) Myelin internode Node of Ranvier Case No. Rituximab Indication Transplant CD4/CD8 CD4+ Purine analog exposure CD8+ 1 Diffuse large B-cell lymphoma None N/A 68 N/A N 2 Systemic lupus erythematosus None 1.25 71 57 N 3 Non-Hodgkin lymphoma Autologous 2.17 89 41 N 4 Diffuse large B-cell lymphoma None 0.39 94 243 N 5 Mantle cell lymphoma None 0.35 110 310 N 6 Follicular lymphoma None 0.29 152 532 N 7 Follicular lymphoma Autologous 0.23 234 1015 N 8 Chronic lymphocytic leukemia None 0.92 287 311 N 9 Mantle cell lymphoma Allogeneic 0.31 403 1309 N 10 Marginal zone B-cell lymphoma Autologous 0.21 551 2596 N 11 Autoimmune hemolytic anemia None 1.47 562 382 N 12 Follicular lymphoma None 0.30 570 1871 N 13 Autoimmune hemolytic anemia Allogenie 0.31 1059 3453 N 14 Waldenstrom macroglobulinemia None 0.34 2100 6200 Y Carson, Blood 2009 Nine of ten with severe CD4 lymphopenia or low CD4/CD8 ratio Abnormal CD4 counts or CD4/CD8 ratio possibly due to cytotoxic chemotherapy and not rituximab, based on clinical trial data What about T-cell function after rituximab? Response in ITP associated with changes in T-cell compartment (Stasi et al, Blood 2007) Modification of T-cell phenotype and cytokine profiles in patients with SLE and Evans’ syndrome (Tamimoto et al, Rheumatology Advanced Access 4/8/2008) Rapid effect in multiple sclerosis suggests rituximab targets a process thought to be T-cell mediated (McFarland HF, NEJM 2/14/08) Through inhibition of T- and B-lymphocyte interactions, rituximab is contributing to viral reactivation and PML. Criticism- Latent site of JC virus is in hematopoietic cells and likely B-lymphocytes. This may be how natalizumab causes PML 5/5 bone marrow samples tested for JC in patients with PML, positive 2/86 bone marrow samples from MSD at NIH with no PML, positive Odds-ratio not calculable Rituximab + chemotherapy increases risk of JC reactivation and PML ◦ JC latent in CD34+ cells and early B-cells ◦ Chemotherapy mobilizes stem cells from bone marrow Causes quantitative T-cell depletion ◦ Rituximab Reduces qualitative T-cell response B-cell depletion results in expansion of progenitor cells containing latent JC Retrospective Case-series Hypothesis is speculative and not verified in laboratory model T-cell findings not yet shown to be significant in casecontrol study Case-control study of T-cell markers after exposure to R-chemo and chemo without rituximab Case-control study of marrow specimens from disease and treatment matched controls Cohort study using large EMR or government database (VA, Kaiser, and/or Medicare) Using methods of SONAR project, important hypotheses can be explored Subsequent investigations allow clarification of issues raised by SONAR Rituximab may be associated with multiple viral reactivation syndromes, screening and early detection could be helpful in prevention. Ticlopidine- and clopidogrel-associated Thrombotic Thrombocytopenia Purpura (TTP) Thrombotic Thrombocytopenic Purpura (TTP) Clinical features • Microangiopathic hemolytic anemia • Thrombocytopenia • Microvascular thrombosis • Renal Failure • Neurological abnormalities Epidemiology •Incidence may be rising Increased awareness & diagnosis Increased exposure to TTP-associated agents (ticlopidine, clopidogrel & prasugrel) Drug-Associated Thrombotic Thrombocytopenic Purpura Among all clinically diagnosed TTP, 20% are drug-associated Of all drug-associated TTP • Most frequent: ticlopidine Ticlopidine • Next frequent: clopidogrel Clopidogrel •1991: association of TTP with ticlopidine •2000: association of TTP with clopidogrel Drug-Associated Thrombotic Thrombocytopenic Purpura Incidence & significance of thienopyridine-associated TTP •Ticlopidine •Coronary artery stent: 1 in 1,500 to 1 in 5,000 patients •Cerebrovascular disease: 1 in 100,000 patients •5 cases per year before development of stent procedures •Stents: important contributing factor to occurrence of TTP Used by 100,000 in the U.S. • Clopidogrel •1 in 100,000 to 1 in 250,000 patients Used by 6 million in the U.S. Bennett CL, Davidson CD, et al. 1999. Thrombotic thrombocytopenic purpura associated with Ticlopidine in the setting of coronary artery stents and stroke prevention. Arch Intern Med 159: 2524-2528 Of the 11 patients, 10 received clopidogrel <14 days before TTP onset. Bennett et al. 2000. Thrombotic Thrombocytopenia Purpura Associated with Clopidogrel. NEJM, 342 (24): 1773-77. Study Objectives ◦ To describe clinical and laboratory findings for a large cohort of patients with thienopyridine-associated thrombotic thrombocytopenic purpura (TTP). Methods ◦ Clinical reports of TTP associated with clopidogrel and ticlopidine were identified from medical records, published case reports, and FDA case reports (n=128). ◦ Duration of thienopyridine exposure, clinical and laboratory findings, and survival were recorded. ◦ ADAMTS13 activity and inhibitor were measured for a subset of individuals. Bennett CL, Kim B, Zakarija A, et al. Two mechanistic pathways of thienopyridine-associated thrombotic thrombocytopenia purpura: Results from the SERF-TTP Research Group and the RADAR Project. J Am Coll Cardiol 2007; 50 (12): 1138-43. 279 articles identified in MEDLINE, EMBASE, the public website of the FDA and abstracts from national scientific conferences from 1991 to 2010 using terms: TTP, ticlopidine, clopidogrel, TTP 215 articles reviewed 138 articles on ticlopidineassociated TTP Articles were excluded if they were in a language other than English and if there were duplicates (N=64) 67 articles on clopidogrelassociated TTP 29 articles reviewed Articles were excluded if they did not include details on pharmacology, epidemiology, laboratory or basic science studies (N=176) Time on Onset Differences in thienopyridine-associated TTP Time to Onset 70 60 50 40 30 30 40 ADAMTS13 deficient n=26 Clopidogrel n=35 Ticlopidine n=93 0 0 10 10 20 Percentage of patients with TTP 70 60 50 ADAMTS13 Non deficient n=13 20 Percentage of patients with TTP 80 80 90 90 Time to Onset 0 5 10 15 20 25 30 35 40 45 50 0 5 10 days 15 20 25 30 35 40 45 50 days ▲Figure 1. Left ▲Figure 1. Right Thienopyridine-Associated TTP Onset: ADAMTS13 Deficient versus ADAMTS13 Non-Deficient (p>0.05). Thienopyridine-Associated TTP Onset: Ticlopidine versus Clopidogrel (p=0.0016). Bennett CL, Kim B, Zakarija A, et al. Two mechanistic pathways of thienopyridine-associated thrombotic thrombocytopenia purpura: Results from the SERF-TTP Research Group and the RADAR Project. J Am Coll Cardiol 2007; 50 (12): 1138-43. Outcomes for Thienopyridine-Associated TTP Cases Based on Access to Therapeutic Plasma Exchange therapy (TPE). Survival with TPE Survival without TPE All Patients (N=128)* 81.6 % 50.0 % Ticlopidine (N=93) * 85.5 % 45.8 % Ticlopidine Rx < 14 days (N=9) 100.0 % 100.0 % Ticlopidine Rx > 14 days (N=84) 84.1 %* 38.1 %* Clopidogrel (N=35) 72.4 % 66.7 % Clopidogrel Rx < 14 days (N=26) 70.0 % 66.7 % Clopidogrel Rx > 14 days (N=9) 77.8 % Thienopyridine Rx < 14 days (N=35) 76.9 % 77.8 % Thienopyridine Rx > 14 days (N=93) 83.3 %* 38.1 %* Bennett CL, Kim B, Zakarija A, et al. Two mechanistic pathways of thienopyridine-associated thrombotic thrombocytopenia purpura: Results from the SERF-TTP Research Group and the RADAR Project. J Am Coll Cardiol 2007; 50 (12): 1138-43. ADAMTS13 activity and clinical characteristics of idiopathic and thienopyridine-associated TTP cases ADAMTS13 Activity (≤10%) Normal ADAMTS13 Activity (>10%) Idiopathic (n=30) Thienopyridine (n=26) Idiopathic (n=24) Thienopyridine (n=14) Age (years) 40** 67** 46** 62** Sex (%female) 83%* 54%* 96%** 43%** 20,900** 9,269** 51,458 37,000 60%** 96%** 29% 36% 1.4** 2.2** 3.7 2.9 Creatinine >2.5 mg/dl 7% 19% 48% 36% Neurologic Dysfunction 53% 69% 52% 43% Total IgG autoantibodies to ADAMTS13 (prior to TPE) 100% N/A 65% (n=23) N/A Platelet count (mean) Platelet count <20,000/mm3 Creatinine (mean) *p<0.05; **p< 0.001 for comparisons between idiopathic and thienopyridine associated TTP in each ADAMTS13 cohort. Note: Total numbers of patients (n) are provided where information are not available for the entire cohort. Idiopathic vs. Thienopyridine Associated TTP ADAMTS13 Activity (≤10%) Idiopathic (n=30) Thienopyridine (n=26) Normal ADAMTS13 Activity (>10%) Idiopathic (n=24) Thienopyridine (n=14) Neutralizing autoantibodies to ADAMTS13 (prior to TPE) Ticlopidine Clopidogrel 79%* 39% Neutralizing autoantibodies to ADAMTS 13 (measured at remission) 46% N/A 29% N/A % cases ADAMTS13 level 1150% 0% 0% 33% 79% 30-day survival 97% 85% 96% 57% 1-year relapse 33% 8% 13% 0% 100%* (n=23) 100% (n=2) N/A 0% (n=6) *p<0.05; **p< 0.001 for comparisons between idiopathic and thienopyridine associated TTP in each ADAMTS13 cohort. Note: Total numbers of patients (n) are provided where information are not available for the entire cohort. Clinical characteristics of ticlopidine vs clopidogrel associated TTP Cases Ticlopidine (n=30) Clopidogrel no relapse (n=8) Age (years) 68 58 Platelet count <20,000/mm3 90% 13% Creatinine >2.5 mg/dl 20% 50% Neurologic Dysfunction 60% 50% Neutralizing autoantibodies to ADAMTS 13 (at presentation) 100% 0% % cases ADAMTS13 ≤10% 80% 0% % cases ADAMTS13 level 11-50% 20% 63% Percent < 2 weeks 0% 50% Percent 2-12 weeks 100% 25% Percent > 12 weeks 0% 25% Percent received TPE 83% 100% Survival after TPE 85% (n=26) 50% (n=8) 30-day survival 80% 50% 1-year relapse 0% 0% Duration of Thienopyridine Use: ADAMTS13 Activity (≤10%) ADAMTS13 Activity (>10%) Neutralizing Antibody at Presentation Present (n=23) Not Present (n=6) Present (n=10) Not Present (n=14) Age (years) 38 43 48 45 Sex (%female) 87% 67% 100.0% 92.3% Platelet count (mean) 19,261 24,000 38,400 60,786 Platelet count <20,000/mm3 65% 50% 30.0% 28.6% Creatinine (mean) 1.27 1.70 3.66 10.49 Creatinine >2.5 mg/dl 4% 20% 50.0% 42.9% Neurologic Dysfunction 52% 67% 40.0% 61.5% Neutralizing autoantibodies to ADAMTS 13 (measured at remission) 60%* (n=20) 0%* 50.0% 18.2% % cases ADAMTS13 level 11-50% 0% 0% 50.0% 21.4% 30-day survival 95%(n=22) 100% 100.0% 92.9% 1-year relapse 57% 17% 25.0% 0.0% Most ticlopidine-associated TTP cases” - occur after 2 weeks of drug exposure, - ADAMTS13 deficient, - 100% have ADAMTS13 autoantibodies at presentation but do not relapse - immune-mediated involving neutralizing antibodies to ADAMTS-13. Clopidogrel-associated TTP cases: - occur within days of drug exposure, - do not exhibit ADAMTS13 deficiency, - does not have ADAMTS13 autoantibodies at presentation but do not relapse - less responsive to TPE - may be a direct result of endothelial damage, Bennett CL, Kim B, Zakarija A, et al. Two mechanistic pathways of thienopyridine-associated thrombotic thrombocytopenia purpura: Results from the SERF-TTP Research Group and the RADAR Project. J Am Coll Cardiol 2007; 50 (12): 1138-43. Bennett CL, Georgantopoulos P, Matsumoto M, Rock G, Fujimura Y, et al. Thrombotic thrombocytopenic purpura (TTP) patients associated with ticlopidine: A review of 22 cases in Japan. (Under Review). Matsumoto (n= 186) Bennett (n=22) Bennett this paper (n= 98) Tsai (n=7) Steinhubl (n=19) Country Japan Japan United States United States United States % female 55.1% 45.50% 46.6% 70.0% 30.0% Median Age (yrs)* 54 (8 mos87)* 69 (41- 89)* 64.2 (11.1= SD) 57 (42-89) 62 (38-75) 96.0% (23/24) 71.9% 100.0% 89.4% Plt < 20k/mm3 100.0% Hgb < 9 g/dl 75.0% 72.7% 26.9% 42.3% 66.7% Cr > 2.5 mg/dl* Neurologic abnormality 75.8% 18.1% 30.1% NA 47.0% 79.0% 63.6% 73.1% 70.0% 73.7% Median days ticlopidine (range) Not applicable 27.5 (14 -36) 21 (7-112) 21 (14-56) 21 (14-28) *p<0.05 for comparison between acquired idiopathic TTP Matsumoto (n= 186) Bennett (n=22) Bennett this paper (n= 98) Tsai (n=7) Steinhubl (n=19) Survival 84.3% 91.03% 84.9% 100.0% 78.9% % Therapeutic plasma exchange (TPE) Not available 63.6% 74.2% 100.0% 68.4% Survival w/o TPE Not available 66.70% 42.1% Not available 33.3% Survival w/ TPE* 83.9%* 100.0%* 81.7% 100.0% 100.0% % w/ ADAMTS13:AC deficiency (<10%) 100.0% 100.0% 100.0% 83.3% Not available % with ADAMTS13 inhibitors 97.8% 100.0% Not available 100.0% Not available *p<0.05 for comparison between acquired idiopathic TTP Idiopathic TTP and thienopyridine-associated TTP represent distinct clinical syndromes. Ticlopidine- and clopidogrel-associated TTP are also distinct clinical syndromes. Measurement of ADAMTS13 activity as well as ADAMTS13 auto-antibodies provides important information that characterizes the two different mechanistic pathways for thienopyridine-associated TTP syndromes. Gadolinium-Associated Nephrogenic Systemic Fibrosis Bennett CL, Qureshi ZP, Sartor AO, Norris LB, Murday A, Xirasagar S, Thomsen HS. Gadolinium Induced Nephrogrenic Systemic Fibrosis, the Rise and Fall of an Iatrogenic Disease. Clinical Kidney Journal, 2012; 5: 82-88. Overview: ◦ The first cases of nephrogenic systemic sclerosis were initially identified by Cowper et al. in 1997 and published in 2000. ◦ Fifteen patients on hemodialysis presented with thickening and hardening of the skin and scleromyxedema-like features. ◦ This condition can be quite disabling because the skin tightening and musculo-tendinous involvement result in joint contractures that can reduce the range of motion of joints. Subtype Description 1 New-onset acute renal failure or acute decompensation in CKD Pneumonia like disorder, followed by acute renal failure Surgical procedure (often vascular) or acute blood loss, followed by acute renal failure Kidney transplant 2 3 4 5 6 7 Chronic kidney disease, unknown trigger Thrombotic event, renal failure may prewdate or follow the event Brain tumor Percentage of previously reported patients (n=100) 25 6 18 34 3 12 1 NFD progression May be transient Usually transient May be transient May be transient Usually chronic May be transient Unknown Number of Cases * Indicates a linear chelating agent Key Events (US): •Grobner’s report (2005) •First FDA report: summarizes Danish findings and indicates that the FDA is investigating (2006) •FDA advisory warns of GBCA administration to persons with CKD stage 4-5 (2007) •Black-box warnings issued (2008) Swift but uncoordinated efforts led to identifying and disseminating information GBCA-associated NSF Nearly a 70% drop in US cases from 1997 to 1998 ◦ The US still accounts for the vast majority of NSF cases worldwide The absence of a centralized registry of NSF cases resulted in variable quality and quantity of case reports The individual safety databases in this study will be derived from: ◦ FDA’s MedWatch: European Medicines Agency ; Published case reports and case series ◦ International Registry maintained at the Yale University School of Medicine ◦ Medical record reviews ◦ Safety reports collated by 23 product safety law firms ◦ Safety reports obtained from two of the manufacturers of GCCAs Report on the long-term outcome of persons with NSF. We hope to adjudicate weather NSF is a class- or product-specific toxicity (as we did with Epo-associeated PRCA) Bennett CL, Luminari S, Nissenson AR, et al. Pure red-cell aplasia and epoetin therapy. N Engl J Med 2004; 351:1403-8.