Foundations in Microbiology
advertisement

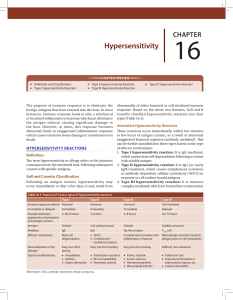
Lecture PowerPoint to accompany Foundations in Microbiology Sixth Edition Talaro Chapter 16 Disorders in Immunity Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Immunopathology • Allergy, hypersensitivity – an exaggerated, misdirected expression of immune responses to an allergen (antigen) • Involves the same types of immune reactions as those at work in protective immunities • Autoimmunity – abnormal responses to self Ag • Immunodeficiency – deficiency or loss of immunity • Cancer – results from a lack of surveillance 2 3 4 Type I Hypersensitivity Two levels of severity: • Atopy – any chronic local allergy such as hay fever or asthma • Anaphylaxis – a systemic, often explosive reaction that involves airway obstruction and circulatory collapse 5 Contact With Allergens • Generalized predisposition to allergies is familial – not to a specific allergy • Allergy can be affected by age, infection, and geographic area. • Atopic allergies may be lifelong or may be “outgrown”; may also develop later in life. 6 Nature of Allergens and Their Portals of Entry • Allergens have immunogenic characteristics. • Typically enter through epithelial portals – respiratory, gastrointestinal, skin • Organ of allergic expression may or may not be the same as the portal of entropy. 7 Mechanism of Type I Allergy Develop in stages: • Sensitizing dose – on first contact with allergen, specific B cells form IgE which attache to mast cells and basophils; generally no signs or symptoms • Provocative dose - subsequent exposure with the same allergen binds to the IgE-mast cell complex • Degranulation releases mediators with physiological effects such as vasodilation and bronchoconstriction. • Symptoms are rash, itching, redness, increased mucous discharge, pain, swelling, and difficulty breathing. 8 9 Role of Mast Cells and Basophils • Mast cells are located in the connective tissue of virtually all organs; high concentration in lungs, skin, GI and genital tract. • Basophils circulate in blood and migrate into tissues. • Each cell can bind 10,000-40,000 IgE. • Cytoplasmic granules contain physiologically active cytokines, histamine, etc. • Cells degranulate when stimulated by allergen. 10 Insert figure 16.3 Cellular reactions 11 Chemical Mediators and Allergic Symptoms • Act alone or in combination; account for scope of allergic symptoms – histamine, serotonin, leukotriene, platelet-activating factor, prostaglandins, bradykinin • General targets include: skin, upper respiratory tract, GI tract, and conjunctiva. – responses: rashes, itching, redness, rhinitis, sneezing, diarrhea, shedding tears • Systemic targets: smooth muscles, mucous glands, and nervous tissue – responses: vascular dilation and constriction resulting in change in blood pressure and respiration 12 13 • Histamine – most profuse and fastest acting; stimulator of smooth muscle, glands, and eosinophils – response to chemical depends on the muscle location: constricts smooth muscles of small bronchi, intestines; relaxes vascular smooth muscles 14 Specific Diseases • Atopic disease – hay fever, rhinitis; seasonal, inhaled plant pollen or mold – asthma – severe bronchoconstriction; inhaled allergen – eczema – dermatitis; ingestion, inhalation, skin contact • Food allergy – intestinal portal can affect skin and respiratory tract – vomiting, diarrhea, abdominal pain; possibly severe – eczema, hives, rhinitis, asthma, occasionally anaphylaxis • Drug allergy – common side effect of treatment; any tissue can be affected; reaction from mild atopy to fatal anaphylaxis 15 Systemic Anaphylaxis • Sudden respiratory and circulatory disruption that can be fatal in a few minutes • Allergen and route are variable. • Bee stings, antibiotics or serum injection 16 Diagnosis of Allergy • Important to determine if a person is experiencing allergy or infection • Skin testing 17 Treatment and Prevention General methods include: 1. Avoiding allergen 2. Use drugs that block the action of the lymphocytes, mast cells, chemical mediators – antihistamines. 3. Desensitization therapy – injected allergens may stimulate the formation of high-levels of allergen-specific IgG that act to block IgE; mast cells don’t degranulate 18 19 20 Type II Hypersensitivity • Reactions that lyse foreign cells • Involve antibodies, complement, leading to lysis of foreign cells • Transfusion reactions – ABO blood groups – Rh factor – hemolytic disease of the newborn 21 Human ABO Antigens and Blood Types • 4 distinct ABO blood groups • Genetically determined RBC glycoproteins; inherited as 2 alleles of A, B, or O • 4 blood types: A, B, AB, or O – named for dominant antigen(s) – type O persons lack both A and B antigens – Tissues other than RBCs also carry A and B antigens. 22 23 Antibodies Against A and B Antigens • Serum contains pre-formed antibodies that react with blood of another antigenic type-agglutination; potential transfusion complication • Type A contains Abs that react against B antigens. • Type B contains Abs that react against A antigens. • Type O contains Abs that react against A and B antigens. • Type AB contains no Abs that react against A or B antigens. 24 25 26 Rh Factor and Hemolytic Disease of the Newborn • RBC antigen – type results from combination of 2 alleles • Inheriting one dominant gene results in the production of the Rh antigen; no pre-formed antibodies exist; must have exposure. • Hemolytic Disease of the Newborn (HDN) – an Rh mother forms antibodies to her Rh+ fetus; usually requires subsequent exposure to the antigen to be hemolytic • Prevention requires the use of passive immunization with antibodies against the Rh antigen; prevents sensitization of mother. 27 Insert figure 16.12 Development and control of Rh 28 Type III Hypersensitivity • A large quantity of soluble foreign Ag stimulates Ab that produce small, soluble Ag-Ab complexes. • Immune complexes become trapped in tissues and incite a damaging inflammatory response. – arthus reaction – local reaction to series of injected Ag to same body site – serum sickness – systemic disease resulting from repeated injections of foreign proteins 29 30 Type IV Hypersensitivity • T cell-mediated • Delayed response to Ag involving activation of and damage by T cells • Delayed allergic response – skin response to allergens – tuberculin skin test, contact dermititis from plants, metals, cosmetics • Graft rejection – reaction of cytotoxic T cells directed against foreign cells of a grafted tissue; involves recognition of foreign HLA 31 32 T Cells and Organ Transplantation • Graft/transplantation rejection – host may reject graft; graft may reject host • MHC markers of donor tissue (graft) are different; T cells of the recipient recognize foreignness. • Release interleukin-2 which amplifies helper and cytotoxic T cells which bind to donor tissue and release lymphokines that begin the rejection 33 Classes of Grafts Classified according to the degree of MHC similarity between donor and host: autograft – recipient also serves as donor isograft – tissue from identical twin is grafted allograft – genetically different individuals but of the same species (humans) xenograft – individuals of different species • Rejection can be minimized by tissue matching HLA antigens, immunosuppressive drugs, and use of tissue that does not provoke a type IV response. 34 35 Autoimmunity • In certain type II & III hypersensitivities, the immune system has lost tolerance to autoantigens and forms autoantibodies and sensitized T cells against them. • More common in females • Disruption of function can be systemic or organic specific: – – – – – systemic lupus erythematosus rheumatoid arthritis endocrine autoimmunities myasthenia gravis multiple sclerosis 36 37 38 Immunodeficiency Diseases • Components of the immune response system are absent. Deficiencies involve B and T cells, phagocytes, and complement. • 2 general categories: – primary immunodeficiency – congenital; usually genetic errors – secondary diseases – acquired after birth; caused by natural or artificial agents 39 • Primary immunodeficiency - lack of Bcell and/or T cell activity – B cell defect – agammaglobulinemia – patient lacks antibodies – T cell defect – thymus is missing or abnormal – severe combined immunodeficiency (SCID) - both limbs of lymphocyte system are missing or defective; no adaptive immune response 40 41 • Secondary diseases - due to damage after birth – caused by: infection, organic disease, chemotherapy, or radiation – AIDS most common – T helper cells are targeted; numerous opportunistic infections and cancers 42 The Immune System and Cancer • Overgrowth of abnormal tissue arises due to malfunction of immune surveillance. • Tumors may be benign (nonspreading) selfcontained; or malignant that spreads from tissue of origin to other sites. • Cancers occur in nearly every cell type. • Appear to have genetic alteration that transforms a normal cell • Possible causes include: errors in mitosis, genetic damage, activation of oncogenes, or retroviruses. 43