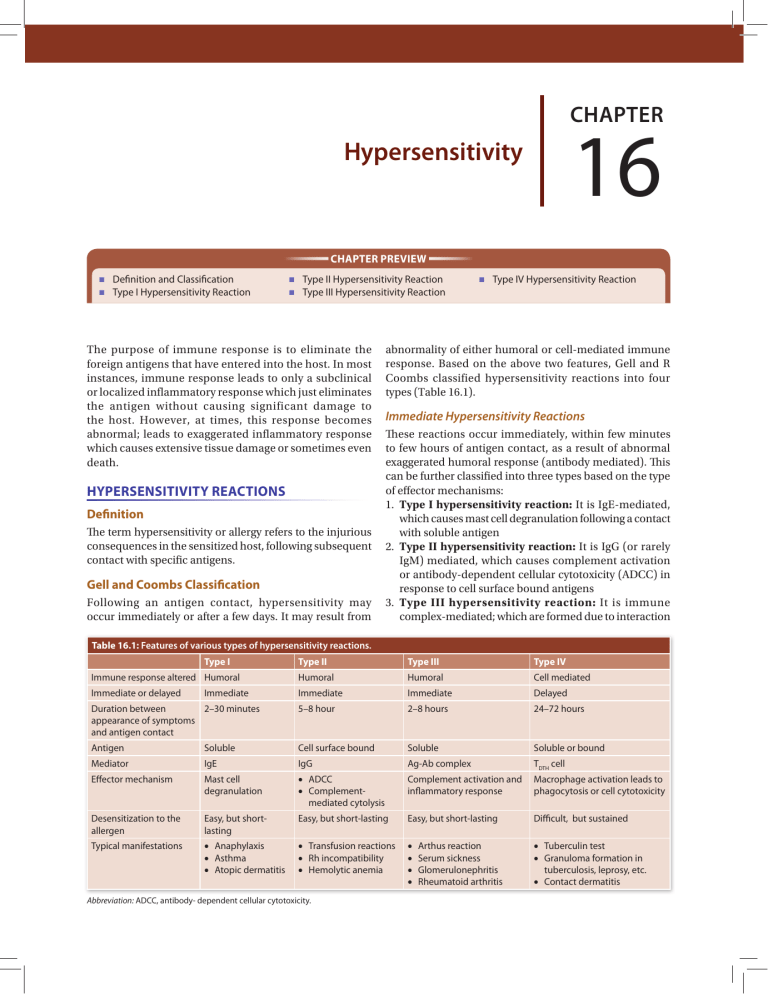
Chapter 16 Hypersensitivity Chapter Preview Definition and Classification Type I Hypersensitivity Reaction Type II Hypersensitivity Reaction Type III Hypersensitivity Reaction The purpose of immune response is to eliminate the foreign antigens that have entered into the host. In most instances, immune response leads to only a subclinical or localized inflammatory response which just eliminates the antigen without causing significant damage to the host. However, at times, this response becomes abnormal; leads to exaggerated inflammatory response which causes extensive tissue damage or sometimes even death. HYPERSENSITIVITY REACTIONS Definition The term hypersensitivity or allergy refers to the injurious consequences in the sensitized host, following subsequent contact with specific antigens. Gell and Coombs Classification Following an antigen contact, hypersensitivity may occur immediately or after a few days. It may result from Type IV Hypersensitivity Reaction abnormality of either humoral or cell-mediated immune response. Based on the above two features, Gell and R Coombs classified hypersensitivity reactions into four types (Table 16.1). Immediate Hypersensitivity Reactions These reactions occur immediately, within few minutes to few hours of antigen contact, as a result of abnormal exaggerated humoral response (antibody mediated). This can be further classified into three types based on the type of effector mechanisms: 1. Type I hypersensitivity reaction: It is IgE-mediated, which causes mast cell degranulation following a contact with soluble antigen 2. Type II hypersensitivity reaction: It is IgG (or rarely IgM) mediated, which causes complement activation or antibody-dependent cellular cytotoxicity (ADCC) in response to cell surface bound antigens 3. Type III hypersensitivity reaction: It is immune complex-mediated; which are formed due to interaction Table 16.1: Features of various types of hypersensitivity reactions. Type I Type II Type III Type IV Immune response altered Humoral Humoral Humoral Cell mediated Immediate or delayed Immediate Immediate Delayed Duration between 2–30 minutes appearance of symptoms and antigen contact 5–8 hour 2–8 hours 24–72 hours Antigen Soluble Cell surface bound Soluble Soluble or bound Mediator IgE IgG Ag-Ab complex TDTH cell Effector mechanism Mast cell degranulation •• ADCC •• Complementmediated cytolysis Complement activation and inflammatory response Macrophage activation leads to phagocytosis or cell cytotoxicity Desensitization to the allergen Easy, but shortlasting Easy, but short-lasting Easy, but short-lasting Difficult, but sustained Typical manifestations •• Anaphylaxis •• Asthma •• Atopic dermatitis •• Transfusion reactions •• Rh incompatibility •• Hemolytic anemia •• •• •• •• •• Tuberculin test •• Granuloma formation in tuberculosis, leprosy, etc. •• Contact dermatitis Immediate Abbreviation: ADCC, antibody- dependent cellular cytotoxicity. Arthus reaction Serum sickness Glomerulonephritis Rheumatoid arthritis 194 Section 2 Immunology between soluble antigen and antibody (usually IgG), resulting in an abnormal inflammatory response. Delayed Hypersensitivity Reaction Delayed hypersensitivity reaction occurs after few days of antigen contact, as a result of abnormal cellmediated immune response. This is also called type IV hypersensitivity reaction. It is mediated by a specific subset of TH cells called delayed hypersensitivity T cells or TDTH cell. TYPE I HYPERSENSITIVITY REACTION The hallmark of type I hypersensitivity reaction is production of IgE by sensitized B cells following a contact with an allergen which inturn induces mast cell degranulation. The pharmacologically active mediators released from these granules cause vasodilation, vascular and smooth muscle contraction and increased vascular permeability. These changes ultimately lead to localized response (called atopy) and systemic response (called anaphylaxis). The wheal and flare response occurs in three stages, as follows: 1. Begins with the appearance of an erythematous area at the site of injury, followed by 2. Development of a flare (erythema) surrounding the site 3. Finally, a wheal (swelling and congestion) forms at the site as fluid leaks under the skin from the surrounding capillaries. Mechanism of Type I Hypersensitivity Type I hypersensitivity reaction occurs through two phases; the sensitization and effector phases, both occurring with an interval of 2–3 weeks (Fig. 16.1). Sensitization Phase This occurs when an individual is exposed for the first time to the sensitizing or priming dose of an allergen. Sensitization is most effective when the allergen is introduced parenterally, but may occur by any route, including ingestion or inhalation In susceptible individuals, very minute doses can be sufficient to sensitize the host Allergens Allergens are foreign antigens that induce allergy. List of allergens is given in Table 16.2. Experiments to Demonstrate Type I Reaction Several experiments were conducted in the past to demonstrate type I hypersensitivity reactions; out of which, the most popular was P–K Reaction. P–K Reaction K Prausnitz and H Kustner (1921) were the first to demonstrate that antibody in the serum responsible for the allergy, and named it as P-K antibody or reaginic antibody; which later was known as IgE (in 1960), after its discovery. The experiment was as follows. Serum from an allergic person is injected intradermally into a nonallergic individual. Later when the appropriate allergen is injected at the same site, a wheal and flare reaction is developed at the site Table 16.2: Common allergens associated with type I hypersensitivity reaction. Allergen types Examples Food Nuts, egg, peas, sea food, beans, milk Plants and pollens Rye grass, rag weed Proteins Foreign serum, vaccines Drugs Penicillin, sulfonamides, local anesthetics and salicylates Insect bite products Venom of bee, wasp, ant, cockroach calyx and dust mites Others Mold spores, animal hair and dander Fig. 16.1: Mechanism of type I hypersensitivity reaction. Chapter 16 Hypersensitivity The allergen is processed by the antigen presenting cells and the antigenic peptides are presented to the CD4 helper T cells Activated TH cells are differentiated into TH2 cells which in turn secrete interleukin 4 (IL-4) IL-4 induces the B cells to differentiate into IgE producing plasma cells and memory cells. Many molecules of IgE with specificities against various epitopes of the allergen may be produced Secreted IgE migrate to the target sites, and coat on the surface of mast cells and basophils. Fc region (the CH3 and CH4 domains) of IgE binds to high affinity Fc receptors (e.g. FcεR1) present on mast cell surface Such sensitized mast cells (coated with IgE) will be waiting for interaction with the subsequent antigenic challenge. Effector Phase When the same allergen is introduced subsequently (shocking dose), it directly encounters with the Fab region of IgE coated on mast cells. IgE cross linkage initiates degranulation: Allergen bound to IgE triggers the mast cells (and basophils) activation and degranulation. Granules in turn release a number of pharmacologically active chemical mediators that lead to the various manifestations of type-1 reaction The memory B cells further differentiate into plasma cells that produce IgE Degranulation in two phases: Mast cells and basophils undergo degranulation in two phases 1. Primary mediators: The preformed chemical mediators which are already synthesized by mast cells, are immediately released, e.g. histamine and serotonin (Table 16.3) 2. Secondary mediators: The mast cells synthesize them following stimulation by allergen and release, e.g. prostaglandins and leukotrienes (Table 16.3). Pharmacological actions: The chemical mediators perform several pharmacological actions, such as bronchial and other smooth muscle contraction, increased vascular permeability and vasodilation (Table 16.3) Symptoms: These actions in combinations, produce symptoms such as breathlessness, hypotension and shock leading to death at times. Manifestations of Type I Reaction Manifestations are grouped into immediate and late. Immediate Manifestations Systemic Anaphylaxis It is an acute medical emergency condition, characterized by severe dyspnea, hypotension, and vascular collapse leading to death at times. It occurs within minutes of exposure to allergen and unless treated promptly, may lead to fatality Table 16.3: Mediators of type I hypersensitivity. Primary mediators Action Histamine, heparin and ↑Vascular permeability serotonin ↑Smooth-muscle contraction Eosinophil chemotactic Eosinophil chemotaxis factor (ECF-A) Neutrophil chemotactic Neutrophil chemotaxis factor (NCF-A) Proteases Bronchial mucous secretion Degradation of blood-vessel and basement membrane Secondary mediators Action Platelet-activating factor Platelet aggregation and degranulation; Contraction of pulmonary smooth muscles Leukotrienes ↑ Vascular permeability; contraction (slow reactive substance of of pulmonary smooth muscles anaphylaxis, SRS-A) Prostaglandins ↑Vasodilation; Contraction of pulmonary smooth muscles Platelet aggregation Bradykinin ↑Vascular permeability; smoothmuscle contraction Cytokines Systemic anaphylaxis; (IL-1 and TNF-α) ↑ Expression of cell adhesion molecules (CAMs) on venular endothelial cells Allergens: Wide range of allergens have been shown to trigger anaphylaxis in susceptible humans, including the venom (from bee, wasp, and ant stings); drugs (such as penicillin, insulin), antitoxins, seafood and nuts Epinephrine (adrenalin) is the drug of choice for systemic anaphylactic reactions. Localized Anaphylaxis (Atopy) Here, the reaction is limited to a specific target tissue or organ, mostly the epithelial surfaces at the entry sites of allergen. These allergies afflict more than 20% of people. They almost always run in families (i.e. inherited) and are collectively called atopy. Examples include: Allergic rhinitis (or hay fever): It is the most common atopic disorder, affecting 10% of the population. This results from exposure to airborne allergens with the conjunctiva and nasal mucosa leading to appearance of various symptoms such as ↑watery secretions of the conjunctiva, nasal mucosa, and upper respiratory tract, as well as sneezing and coughing Asthma: It is the second most common atopic manifestation. It differs from hay fever in involvement of lower respiratory mucosa, resulting in contraction of the bronchial smooth muscles and airway edema, ↑mucus secretion; all together leading to bronchoconstriction and dyspnea. The stimulus may or may not be an allergen. Accordingly, asthma can be classified as: 195 196 Section 2 Immunology Allergic asthma: It is induced by air-borne or bloodborne allergens, such as pollens, dust, fumes, insect products, or viral antigens Intrinsic asthma: It is independent of allergen stimulation; induced by exercise or cold. Food allergy: Various foods also can induce localized anaphylaxis in atopic individuals. The food allergens (e.g. nuts, egg, seafood, etc.) can either stimulate the mast cells lining gut mucosa to cause GI symptoms such as diarrhea and vomiting or may be carried in the blood stream to distant sites (e.g. when the allergen is deposited on skin, causes local wheal and flare like reaction called atopic urticaria (or hives) Atopic dermatitis (allergic eczema): It is an inflammatory disease of skin that is frequently associated with young children with family history of atopy. It often develops during infancy, manifested as erythematous skin eruptions which are filled with pus.The skin lesions have an increased response of TH2 cells and eosinophils Drug allergy: Various drugs (such as penicillin, sulfonamides, etc.) may produce type I hyper-sensitivity responses which may be either local reactions or even sometimes produce systemic anaphylaxis. Late Manifestations The immediate phase of type 1 reaction is followed, 4–6 hours later, by an inflammatory response. This phase lasts for 1–2 days and leads to tissue damage. Mediators: They are released in acute phase along with cytokines (IL-3, IL-5, IL-8), ECF and NCF; induce recruitment of various inflammatory cells, such as neutrophils, eosinophils, macrophages, and lymphocytes, etc. Among the infiltrates, eosinophils and neutrophils predominate; each accounting for 30% of the total inflammatory cells influx Eosinophil influx: It is favored by ECF (eosinophil chemotactic factor), IL-5 and GM-CSF. Eosinophils express Fc receptors for IgG and IgE and thus bind directly to antibody-coated allergens. This in turn causes release of toxic granules from eosinophils which contribute to the chronic inflammation of the bronchial mucosa that characterizes persistent asthma Neutrophil infiltration: It is induced by NCF (neutrophil chemotactic factor), and other cytokines such as IL-8. Activated neutrophils release various mediators which further potentiate inflammatory tissue damage and thickening of basement membrane. There are several gene loci identified which encode proteins that are involved in the regulation of immune responses towards the allergens It is also observed that if both the parents are allergic there is 50% chance that the child will be allergic and when only one parent is allergic, the chance of the child being allergic drops down to 30%. 2. Allergen Dose The dose of the allergen has a definite impact on the type of immune response produced. It is observed that repeated small doses of allergen induce a persistent IgE response in mice; while higher dosage leads to transient IgE response with a shift towards IgG response. 3. TH1 vs TH2 Response The balance between TH1 and TH2 response determines the response of an individual towards an allergen. TH1 response produces cytokine interferon-γ, which is inhibitory to type I hypersensitivity; whereas TH2 response induced cytokine IL-3, IL-4 and IL-5 promotes IgE-mediated allergic response Hence, accordingly atopic and non-atopic individuals would demonstrate a predominant TH2 and TH1 response to an allergen respectively. Detection of Type I Hypersensitivity Skin Prick Test Small amounts of suspected potential allergens are introduced at different skin sites either by intradermal injection or by superficial scratching. If a person is already sensitized to the allergen, a local wheal and flare response develops within 30 minutes at the inoculation sites (Fig. 16.2) Advantage: Skin test is relatively inexpensive and allows screening of a large number of allergens at one go Disadvantage: It may occasionally sensitize the individual to new allergens and in some rare cases may induce late-phase reaction or even systemic anaphylactic shock. Factors Influencing Type I Hypersensitivity 1. Genetic Makeup Host genetic factors play an important role in mounting an immune response against an allergen. Some individuals mount a normal response where as some mount an exaggerated immune response. Allergen to one individual may not be allergic to other individual Fig. 16.2: Skin testing by intradermal testing of allergens into forearm. Chapter 16 Hypersensitivity Total Serum IgE Antibody TYPE II HYPERSENSITIVITY REACTION Quantitative detection of total serum IgE is performed by various formats such as enzyme immunoassay or radiometric assay called radioimmunosorbent test (RIST, now not in use). In type II reactions, the host injury is mediated by antibodies (IgG or rarely IgM) which interact with various types of antigens, such as: Host cell surface antigens (e.g. RBC membrane antigens like blood group and Rh antigens) Extracellular matrix antigens or Exogenous antigens absorbed on host cells (e.g. a drug coating on RBC membrane). After Ag-Ab binding occurs, the Fc region of antibody initiates the type II reactions by the following three broad mechanisms (Figs 16.3A and B). Allergen-specific IgE Detection of allergen-specific IgE is more specific than total IgE detection. Various test formats are available. Multiplex immunoblot assay: Uses a nitrocellulose strip coated with 54 allergens Fluoro-enzyme immunoassay (FEIA): Commercially available as ImmunoCAP assay Automated immunoassay system (Hytec 288 Plus system) Anti-CCD absorbent IgE assay: Detects IgE after absorbing (removing) the nonspecific anti-CCD IgE which are produced against the cross-reactive carbohydrate determinants (CCD) present on the allergens RAST: Earlier, a radiometric assay called RAST (Radioallergosorbent test) was in use. T Reatment Type I hypersensitivity reaction Avoidance of contact with known allergens: The first and foremost step is identification and avoidance of contact with known allergens such as dusts, house pets, allergic food, etc. However, it is not practically possible to avoid all allergens especially airborne allergens, such as pollens Hyposensitization: Repeated exposure to increased subcutaneous doses of allergens can reduce or eliminate the allergic response to the same allergen ¾¾ This occurs probably due to either (1) a shift of IgE response towards IgG or (2) a shift of TH2 response towards TH1 response, which secrete IFN-γ that in turn can suppress the IgE response ¾¾ Here, the IgG acts as blocking antibody because it competes with IgE for binding to the allergen. The IgG-allergen immunocomplex can be removed later by phagocytosis. Monoclonal anti-IgE: Humanized monoclonal anti-IgE can bind and block the IgE; but useful only if the IgE is not already bound to high affinity Fc receptors Drugs: Several drugs are useful in suppressing type 1 response through various mechanisms (Table 16.4). Table 16.4: Drugs used in type I hypersensitivity. Drugs Mechanism of action Antihistamines Block H1 receptors on target cells; hence antagonize the effects of histamine released Epinephrine (adrenaline) Stimulates cAMP production in mast cells; thereby prevents mast cell degranulation Also it causes bronchial smooth muscle relaxation and ionotropic effect Cortisone Blocks conversion of histidine to histamine and stimulates cAMP levels in mast cells Theophylline Prolongs high cAMP levels in mast cells Cromolyn sodium Blocks Ca2+ influx into mast cells Abbreviation: cAMP, cyclic adenosine monophosphate. Complement-dependent Reactions The Fc region of antibody (bound with antigen) can activate the classical pathway of complement system. Activation of classical pathway leads to host cell injury which is mediated by the following three mechanisms (Fig. 16.3A). 1. Complement-dependent cytolysis: The membrane attack complex (C5-C9) formed by the activation of classical pathway can produce pores which lead to lysis of the target cells 2. Complement-dependent inflammation: The byproducts of complement pathways such as C3a and C5a are chemoattractants; hence can induce inflammatory response leading to tissue injury 3. Opsonization: By-products of complement pathway, such as C3b and C4b act as opsonins. They deposit on the target cells. Phagocytes, such as macrophage and neutrophil can engulf such C3b and C4b coated target cells via complement receptors. Complement Mediated Type II Reactions Antibody-dependent complement mediated type II hyper­ sensitivity is observed in various clinical conditions such as: Transfusion reaction (ABO incompatibility): RBCs from an incompatible donor are destroyed after being coated with recipient antibodies directed against the donor’s blood group antigens (Fig. 16.3A) Erythroblastosis fetalis (Rh incompatibility): Rh negative mother having anti-Rh antibodies due to prior exposure to Rh positive blood (due to previous pregnancy or blood transfusion), can cross the placenta and cause destruction of Rh-positive fetal RBCs Autoimmune hemolytic anemia, agranulocytosis, or thrombocytopenia: All these result due to production of autoantibodies to individual’s own membrane antigens of RBCs/granulocytes/platelets respectively Drug-induced hemolytic anemia: Drug or its metabolic products may get adsorbed onto RBC membrane. If antibodies are formed against the drug, these antibodies will bind with the adsorbed drug on RBC surface and lead to complement activation and lysis of RBCs. For example, following quinine therapy used for malaria (resulting in black water fever) and penicillin therapy (Fig. 16.3A) Pemphigus vulgaris (autoantibodies against desmosomal proteins that lead to disruption of epidermal intercellular junctions). 197 198 Section 2 Immunology A B Figs 16.3A and B: Different mechanisms of antibody mediated type II hypersensitivity reactions: A. Complement-dependent reactions; B. Antibody-dependent cellular cytotoxicity (ADCC). Abbreviations: RBC, red blood cell; NK, natural killer. Antibody-dependent Cellular Cytotoxicity (ADCC) IgG antibodies can coat on the target cells by interacting with the surface antigens through Fab region. The Fc portion of IgG in turn binds to Fc receptors on various effector cells such as NK cells which result in destruction of the target cells (Fig. 16.3B). ADCC is involved in destruction of the targets that are too large to be phagocytozed, e.g. parasites, tumors or graft rejection Although ADCC is typically mediated by IgG antibodies, in certain instances (e.g. eosinophil-mediated killing of parasites) IgE antibodies are used. Autoantibody Mediated (Antibody-dependent Cellular Dysfunction or ADCD) In this condition, the host produces certain autoantibodies which bind and disturb the normal function of human selfantigens. Anti-receptor Ab: Antibodies may be directed against human receptors, resulting in either inhibition or excessive activation of the receptors leading to host injury Activation of receptor, e.g. Graves’ disease: Here, the autoantibodies produced are called LATS (longacting thyroid stimulators), which stimulate the thyroid cells to upregulate the production of thyroid hormones Inhibition of receptor, e.g. myasthenia gravis: In this condition, anti-acetylcholine (ACh) receptor antibodies are produced; which block the ACh receptors, leading to profound muscular weakness. Other examples of ADCD: Goodpasture syndrome (antibody produced against type IV collagen) Pernicious anemia (antibody directed against intrinsic factor) Rheumatic fever (antibody against streptococcal antigens cross reacting with heart) Myocarditis in Chagas disease. TYPE III HYPERSENSITIVITY REACTION Type III hypersensitivity reactions develop as a result of excess formation of immune complexes (Ag-Ab complexes) which initiate an inflammatory response through activation of complement system leading to tissue injury (Fig. 16.4). Antigen involved: Immune complexes can involve exogenous antigens such as bacteria and viruses or endogenous antigens such as DNA Removal of immune complexes: Mere formation of immune complexes does not result in type III hypersensitivity reaction Under normal circumstances, the immune complexes are rapidly cleared by activation of complement system Immune complexes coated with complements are either directly phagocytosed by macrophages/ monocytes or are bound to RBCs and carried to liver and spleen where they are phagocytosed. However, in some situations, the immune system may be exposed to excess dose of antigen over long period of time such as in chronic infection, autoimmune diseases, Chapter 16 Hypersensitivity secretory granules (through frustrated phagocytosis) which causes extensive tissue damage. Platelet Activation Immune complexes bind to the Fc receptors on platelets leading to their activation. Platelet aggregation (leads to microthrombi formation) and vasoactive amines released from activated platelets, both together cause tissue ischemia leading to further tissue damage. Activation of Hageman Factor Activation of Hageman factor leads to activation of kinin, which in turn causes vasodilatation and edema. Types of Type III Hypersensitivity Reaction Type III reactions are either localized or generalized. Localized or Arthus Reaction Fig. 16.4: Mechanism of systemic type III hypersensitivity reaction. and repeated exposure to environmental pollutants. This leads to formation of excessive immune complexes. Soluble vs Insoluble Immune Complexes Balance between level of antigen and antibody decides the nature of immune complex that is going to be formed. In case of antibody excess or antigen-antibody equivalence, immune complexes formed are large and insoluble; which tend to localize near the site of antigen administration to produce a localized type III reaction However, in situations when the antigen is in excess (particularly monovalent antigens), small soluble complexes are formed which tend to travel through blood and get deposited in various sites producing a generalized type III reaction. Mechanism of Tissue Injury Classical Complement Activation The Ag-Ab-immune complexes stimulate the classical pathway of complement; the products of which mediate the tissue injury in type III reaction. Anaphylatoxin: Complement by-products C3a and C5a being anaphylatoxins, induce localized mast cell degranulation with consequent increase in vascular permeability Chemoattractant: C3a and C5a also act as chemo­ attractants, causing recruitment of neutrophils to the site of immune complex deposition Role of neutrophils: Neutrophils attempt to phagocytose the large immune complexes, but fail in doing so. Instead, they release large number of lytic enzymes from the Arthus reaction is defined as localized area of tissue necrosis due to vasculitis resulting from acute immune complex deposition at the site of inoculation of antigen. The reaction is produced experimentally (NM Arthus, 1903) by injecting an antigen into the skin of a previously immunized animal, e.g. rabbit (i.e. excess of preformed antibodies against the injected antigen are already present in the circulation). The circulating antibodies bind with the antigen in the dermis and form immune complexes. These immune complexes fix the complement, resulting in localized immune complex mediated inflammatory response called Arthus reaction. In humans, localized Arthus reaction is seen in some situations, such as: In skin: (1) following insect bites or (2) during allergic desensitization treatment wherein repeated injections of the same antigen is given for long periods In lungs, following inhalation of bacteria, fungi, spores or proteins may produce intrapulmonary lesions. Examples include conditions causing extrinsic allergic alveolitis, such as: Farmer’s lung: It develops following inhalation of actinomycetes (Saccharopolyspora species) from mouldy hay Bird-Fancier’s disease: This develops following inhalation of serum proteins in dust derived from dried pigeon’s feces. Generalized or Systemic Type III Reactions The pathogenesis of systemic immune complex disease can be divided into two phases: 1. Formation of small sized soluble Ag-Ab complexes in the circulation, which occurs following the entry of a large dose of antigen into the body 2. Induces inflammatory reaction: Deposition of the immune complexes in various tissues, thus initiating 199 200 Section 2 Immunology Table 16.5: Diseases associated with generalized type III hypersensitivity reactions. Connective tissue disorders: Result due to autoantibodies forming immune complexes with self-antigens •• SLE (systemic lupus erythematosus): Anti-DNA Ab •• Rheumatoid arthritis: Ab against human immunoglobulin •• PAN (polyarteritis nodosa) Parasitic diseases: Resulting from immune complex deposition •• Nephrotic syndrome in Plasmodium malariae •• Katayama fever in schistosomiasis •• African trypanosomiasis Bacterial diseases: Resulting from immune complex deposition •• Streptococcus pyogenes: Post-streptococcal glomerulonephritis •• Mycobacterium leprae (Lepra reaction type 2) Viral diseases: With immune complex deposition •• Hepatitis B (arthritis) •• Hepatitis C (arthritis) •• Infectious mononucleosis (Epstein-Barr virus) •• Dengue (arthritis) Others: •• Hyperacute graft rejection •• Subacute bacterial endocarditis •• Serum sickness Mechanism of Type IV Reactions Type IV hypersensitivity reactions occur through two phases—(1) sensitization and (2) effector phases (Figs 16.5A and B). Sensitization Phase This is the initial phase of 1–2 weeks occurring following antigenic exposure (Fig. 16.5A). During this period, the antigen presenting cells (APCs) process and present the antigenic peptides along with MHC-II to the helper T cells. TH cells are differentiated to form TDTH cells Most TDTH cells are derived from TH1 cells; but occasionally other T cells, such as CD8+ T cells and CD4+ TH17 can also act as TDTH cells. Effector Phase The TDTH cells, on subsequent contact with the antigen, secrete variety of cytokines which attract and recruit various inflammatory cells (e.g. macrophages) at the site of DTH reaction (Fig. 16.5B). an inflammatory reaction in various sites throughout the body such as; blood vessels (vasculitis), glomerular basement membrane (glomerulonephritis), and synovial membrane (arthritis). This has been linked to the pathogenesis of various diseases (Table 16.5). Serum Sickness This is another historical example of type III reaction. This condition is not seen nowadays, it was seen in the past, following serum therapy, i.e. administration of foreign serum, e.g. horse anti-tetanus serum, to treat tetanus cases. The horse serum proteins being foreign can induce antibody formation in the host, leading to generation of large number of immune complexes Typically, after 7–8 days, the individuals begin to show various manifestations which are collectively called serum sickness. The symptoms include fever, weakness, vasculitis, edema, erythema and rarely lymphadenopathy and glomerulonephritis It subsides gradually once the immune complexes are cleared and free antibodies accumulate. TYPE IV HYPERSENSITIVITY REACTION Type IV hypersensitivity reactions differ from other types in various ways: It is delayed type (occurs after 48–72 hours of antigen exposure) It is cell-mediated; characteristic cells called TDTH cells (delayed type of hypersensitivity T cells) are the principal mediators of type IV reactions Tissue injury occurs predominantly due to activated macrophages. Figs 16.5A and B: Mechanism of delayed type hypersensitivity: A. Sensitization phase; B. Effector phase. Abbreviations: APCs, antigen presenting cells; MHC, major histocompatibility complex; TNF, tumor necrosis factor; IFN, interferons; DTH, delayed type hypersensitivity; MCAF, monocyte chemotactic and activating factor; MIF migration inhibitory factor; GM-CSF, granulocyte monocyte colony stimulating factor. 201 Chapter 16 Hypersensitivity Cytokines Secreted from TDTH Cells Interferon-γ: It is the key cytokine of type IV reaction. It activates the resting macrophages into activated macrophages which are highly competent for microbial killing; mediated through several mechanisms such as: ¾¾ ↑ Expression of MHC-II molecules so that they can act as efficient APCs ¾¾ ↑ TNF receptors ¾¾ ↑ Levels of oxygen radicals and nitric oxide. Interleukin-2 (IL-2): It acts in autocrine manner; stimulates the proliferation of TDTHcells MCAF (Monocyte chemotactic and activating factor) and TNF β–Help in migration of monocytes from blood to the site of DTH and transforming them into tissue macrophages MIF (migration inhibitory factor): It further inhibits migration of macrophages from the site of DTH IL-3 and GM-CSF (granulocyte-monocyte colony stimulating factor)-help in local synthesis of monocytes. Role of DTH: Protective vs Tissue Damage Response Through type IV hypersensitivity reactions, host attempts to provide defense against many intracellular microorganisms such as M. tuberculosis as well as several chemicals and nickel salts (Table 16.6). Always, the attempts do not result in protection. Protective Response Under normal circumstances, the pathogens are usually cleared with little tissue damage; mediated by the enhanced microbicidal potency of activated macrophages. Tissue Damage Response However, in conditions, when the intracellular microbes escape the macrophage killing mechanisms; the enhanced phagocytic activity and release of various lytic enzymes by the activated macrophages in an attempt to kill the pathogen leads to nonspecific tissue destruction. Table 16.6: Examples of delayed-type hypersensitivity (DTH). Intracellular pathogens inducing DTH Intracellular bacteria •• Mycobacterium leprae •• M. tuberculosis •• Listeria monocytogenes •• Brucella abortus Intracellular fungi •• Pneumocystis jirovecii •• Candida albicans •• Histoplasma capsulatum •• Cryptococcus neoformans Intracellular viruses •• Herpes simplex virus •• Variola (smallpox) •• Measles virus Skin test to demonstrate DTH •• Tuberculin test (Mantoux test) •• Lepromin test •• Montenegro test (leishmaniasis) •• Frei test—done in LGV Contact dermatitis Following exposure to contact antigens: Nickel, poison ivy, poison oak, picryl chloride Other examples of DTH Noninfectious conditions •• Diabetes mellitus type 1 •• Multiple sclerosis •• Peripheral neuropathies •• Hashimoto’s thyroiditis Granuloma formation seen in Tuberculosis, sarcoidosis, schistosomiasis and other trematode infections •• Crohn’s disease •• Chronic transplant rejection •• Graft-versus-host disease Other example Lepra reaction type I Abbreviation: LGV, lymphogranuloma venereum. and a peripheral rim of fibroblasts and connective tissue (Fig. 16.6). Tuberculin Test Tuberculin test is the prototype of delayed hypersensitivity. In sensitized individuals, (i.e. who possess sensitized TDTH cells due to prior contact with M. tuberculosis); when a preparation of tuberculin antigen (glycerol extract of the tubercle bacillus) is injected intradermally, a local reaction develops after 48–72 hours consisting of induration surrounded by erythema. Pathology of DTH Reaction (Granuloma Formation) Continuous DTH reaction for killing the intracellular microbes (especially persistent and/or nondegradable antigens) leads to formation of granuloma (e.g. tubercles in leprosy and tuberculosis). The initial TH cell infiltrate is progressively replaced by macrophages in 2–3 weeks. Macrophages transform into two type of cells: 1. They become large, flat, and eosinophilic; denoted as epithelioid cells 2. The epithelioid cells occasionally fuse (induced by IFN-γ) to form multinucleated giant cells. Granuloma consists of an inner zone of epithelioid cells, typically surrounded by a collar of lymphocytes Fig. 16.6: Structure of granuloma. 202 Section 2 Immunology Contact Dermatitis This hapten-skin protein complex is internalized by skin Many antigens such as nickel, poison oak, etc. (Table 16.6) act by producing DTH response: Most of these substances are haptens; they complex with skin proteins, which act as carrier to make the haptens immunogenic APCs (e.g. Langerhans cells), then presented to TH cells to induce a TDH reaction Activated macrophages release lytic enzymes which result in skin lesions (e.g. redness and pustule seen following contact with poison oak). EXPECTED QUESTIONS I.Write essay on: 1. Define and classify hypersensitivity reactions. Write in detail about type IV hypersensitivity reaction. 2. Neha, a 17-year student who has recently joined MBBS, has come back to the hostel after the first vacation. After entering to her hostel room, she suddenly developed an episode of severe sneezing, and dyspnea. She had to be admitted to the casualty and when asked, she told that she has faced similar episodes since her childhood. a. What type of immune reaction is this? b. Describe the pathogenesis of this condition and management. II.Write short notes on: 1. Type II hypersensitivity reaction. 2. Immune complex mediated hypersensitivity reaction. III. Multiple Choice Questions (MCQs): 1. Type I hypersensitivity is mediated by which of the following immunoglobulins? a. IgA b. IgG c. IgM d. IgE 2. The type of hypersensitivity reaction in myasthenia gravis is: Answers 1. d 2. b 3. d 4. a 5. d a. Type I b. Type II c. Type III d. Type IV 3. A positive tuberculin test is an example of: a. Type I hypersensitivity b. Type II hypersensitivity c. Type III hypersensitivity d. Type IV hypersensitivity 4. Example of antibody-dependent cellular dysfunction or ADCD: a. Graves’ disease b. Hemolytic anemia c. Pemphigus vulgaris d. Transfusion reaction 5.Which of the following statement is wrong about type III hypersensitivity reaction? a. Antibody excess—produce a localized type III reaction b. Antigen excess—produce a systemic type III reaction c. Antigen-antibody equivalence—produce a localized type III reaction d. Soluble immunocomplexes—produce a localized type III reaction