Miliary TB Meningitis: MRI Findings in Three Patients

Miliary TB Meningitis:
MRI Findings in Three
Patients
1 Kartikasalwah Abd Latif, 1 Mohd Nazri MN, 2 Sobri
Muda
1
Department of Diagnostic Imaging, Kuala Lumpur Hospital, Malaysia
2
Department of Radiology, National University of Malaysia Medical Centre, Kuala Lumpur, Malaysia
INTRODUCTION
Tuberculosis of the central nervous system (CNS) is one of the most serious form of infection caused by
Mycobacterium tuberculosis
It is associated with significant morbidity and mortality.
Increase in immunodeficiency state from various cases is an important contributing factors.
MRI with gadolinium enhancement, is the preferred imaging tool for investigation of CNS tuberculosis:- to differentiate it from other diagnoses and for surveillance during treatment.
A. Be1, Kwang Sik Kim2, William R. Bishai1 and Sanjay K. Jain-Current Molecular Medicine 2009, 9, 94-99 ,G.Alistair Lammie, Richard H.Hewlett, Johan f.Schoeman,
Peter R.Donald .-Journal of Infection S 2009 , 59, 156-166,Richa TRivedi, sona Saksena, Rakesh K Gupta – Indian Journal Imaging Nov 2009, Vol 19,issue, 256-265,
Pieter Janse van Rensburg, Savvas Andronikou ,Ronald van Toorn, Manana Pienaar-PediatrRadiol (2008) 38:1306–1313 , JLS Khoo,1 KY Lau,1 CM Cheung,2 TH Tsoi2-J
HK Coll Radiol 2003;6:217-228
CNS TUBERCULOSIS
Findings on imaging include space occupying lesion(tuberculomas or abscess), abnormal meningeal enhancement , hydrocephalus and vascular complication
Brain tuberculoma, may be single or multiple or miliary in distribution, varying in sizes ranging from
1mm to 8cm
Lesions are called miliary if size is < 2 mm in diameter.
Parenchymal miliary TB is usually associated with
TB meningitis
CASE 1
37 years old businessman whom was previously healthy, presented with one month history of malaise; two weeks history of unsteady gait and scanning speech.
Clinical examination found cerebellar and pyramidal signs with left sided hemiparesis, power of 3/5.
1
st
MR brain
Sagittal contrast T1WI
Coronal contrast T1WI
Miliary leptomeningeal nodules in the subenpendyma area, cerebellar folia and within the sulci
1
st
MR Brain
(Axial contrast T1WI)
Miliary leptomeningeal nodules within the sulci both parietal region
2
nd
MR Brain 2 weeks later
(Axial contrast T1WI)
Miliary nodules in the hemispheric parenchyma
( deep parenchymal location )
2
nd
MR Brain 2 weeks later
(Axial contrast T1WI)
Miliary leptomeningeal and parenchymal nodules,
Few larger nodules (leptomeningeal tuberculomas) were seen
2
nd
MR Brain 2 weeks later
(Gradient Echo Sequence)
Axial GRE Sequence showed punctate microhemorrhages
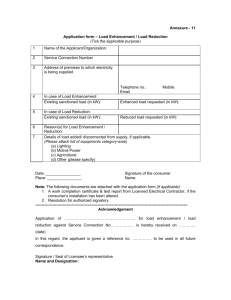
CHEST RADIOGRAPH &
CT-LUNG WINDOW
AP Chest X ray showed diffuse bilateral alveolar opacity and CT showed nodules of
varying sizes including miliary nodules .
CASE 2
47 year old lady, who was on chemotherapy for Diffuse Large B Cell Lymphoma(DBCL), developed acute delirious symptoms.
She had history of necrotising fascitis of her right eye
Clinical examination found left sided hemiparesis
1
st
MR Brain
(Axial & coronal contrast T1WI)
Enhancement of leptomeninges at the cerebelllar folia, larger heterogenously enhancing lesions in right basal ganglia
1
st
MR Brain
(Gradient Echo Sequence)
Axial GRE Sequence showed punctate microhemorrhages
2
nd
MR Brain 3 weeks later
(Axial contrast T1WI)
Increasing miliary parenchymal nodules, leptomeningeal nodules were more confluent
2
nd
MR Brain 3 weeks later
Coronal contrast T1WI Sagittal contrast T1WI
Increasing of milliary nodules in the hemispheric parenchymal ( deep parenchymal location )
CASE 3
A 20 year old male, presented with abnormal behaviour
This was preceded by two weeks history of cough, fever and headache.
He also complained of loss of weight and loss of appetite.
Neurological examination showed evidence of lower limbs weakness, left side with power of 0/5 and right side with power of 3/5
There was associated left seventh cranial nerve palsy.
CT BRAIN
(contrast)
Enhancement in the right basal ganglia and left occipital horn region .
1
st
MR Brain
(Axial contrast T1WI)
Nodular enhancement of leptomeninges in the temporal horn, interpeduncular , prepontine and left choroid plexus areas.
Miliary parenchymal and leptomeningeal nodules in over the right parietal
2
nd
MR Brain 3 months later
(Axial contrast T1WI)
Leptomeninges enhancement were more confluent with thick intense enhancement of basal cisterns, anterior hemispheric and sylvian fissures. Miliary leptomeningeal nodules at parietal region.
2
nd
MR Brain 3 months later
Coronal contrast T1WI Sagittal contrast T1WI
Nodular enhancement of leptomeninges and miliary leptomeningeal nodules
Cranio-spinal meningeal extension
MR cervical Sagittal contrast T1WI thick intense meningeal enhancement at prepontine, over the cerebellum, surrounding brainstem at foramen magnum and meningeal of cervical spinal cord
Cerebral infarct
1 st CT Brain 2 nd CT Brain ( 3 months later)
Acute right internal capsule infarction Old right internal capsule infarction
Chest radiograph
Milliary pattern in both lung fields
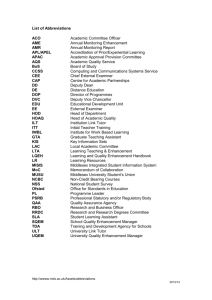
Summary (clinical)
Age (year) /Gender
Constitutional symptoms
Altered mental state
Focal neurological signs
Cranial nerve palsy
Pre-existing medical condition
Chest XR suggestive of pulmonary TB
CSF analysis changes
Case #1
37/Male
+
+
+
-
-
-
Lympocystic pleocytosis,
↑protein, ↓glucose,
↓Cl -
Case #2
47/Female
+
-
+
malignancy
N/A
Lympocystic pleocytosis,
↑protein,
↓glucose, ↓Cl -
Positive M. tuberculosis microscopy
Outcome
Bronchoalveolar lavage fluid
Died
CSF
Died
Case #3
20/Male
+
+
+
+
Hepatitis B
+
Lympocystic pleocytosis,
↑protein,
↓glucose, ↓Cl -
Sputum
Defaulted
Summary (MRI findings)
Miliary nodules distribution
Leptomeningeal
Deep parenchymal
Tuberculoma ( >2mm)
Abnormal meningeal enhancement
Vasculopathy Micro hemorrhages
Case #1
++
+++
+
+
+++
Case #2
+
++
+
+
+
Case #3
+++
+
+
+++
-
Infarction +
Hydrocephalus
Abscess
Cranio-spinal meningeal enhancement
-
-
-
-
-
-
-
-
+
CONCLUSION
Early diagnosis of CNS TB remains challenging due to the insidious onset of nonspecific symptoms.
A high index of suspicion in the appropriate clinical setting may promote early diagnosis and treatment that can prevent unnecessary morbidity and mortality
MRI is an excellent tool to evaluate patients with suspected CNS TB
Miliary nodules (parenchymal and leptomeningeal) is one of the presenting pattern for CNS TB that need to be recognized
Parenchymal miliary TB is usually associated with TB meningitis