Emergency Care Powerpoint
advertisement

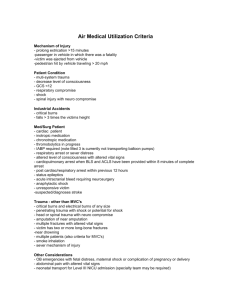
INTRODUCTION TO EMERGENCY CARE EMERGENCIES • Sudden illness or injury that requires an immediate medical response • Emergencies can happen at any time. FIRST AID • In many cases, emergency care may require some form of first aid. • It is important that the general population and all health care workers know how to perform emergency care. • Agencies such as the American Red Cross and the American Heart Association train people to perform these life-saving procedures. EFFECTIVE FIRST AID PROVIDERS Obtain proper first aid training • This includes: ▫ Anyone in the medical field ▫ People in jobs that involve child care ▫ Park guides, camp counselors, life guards, etc. EFFECTIVE FIRST AID PROVIDERS (CONTINUED) Be alert for emergency situations • Unusual sounds • Unusual sights • Unusual odors • Unusual behaviors EFFECTIVE FIRST AID PROVIDERS (CONTINUED) Assess the situation before taking action • The first aid provider should have a reason for every action that is taken. • Treatment depends on multiple factors EFFECTIVE FIRST AID PROVIDERS (CONTINUED) Remain calm in emergency situations and observe safety precautions • If possible, get the patient’s consent • If possible, wash their hands and put on gloves • Make sure supplies are clean. • If possible, explain the procedure • Be careful when lifting heavy objects. • Flush solutions that come into contact with eyes or skin • Only perform care for which trained EFFECTIVE FIRST AID PROVIDERS (CONTINUED) Perform a safety check of the scene before taking action • Some emergency scenes are unsafe to enter. • Call for help immediately. Prioritize tasks and triage • Triage is a way to prioritize treatment. It determines which patient or which injury is treated first. • Life-threatening injuries should always be attended to first. PRINCIPLES OF CARE • Get professional care as soon as possible. • Do not move a patient unless it is required for safety reasons. • Keep the patient calm. • Do not give unconscious or vomiting patients any food or fluids, unless the first aid procedure requires it. • Regulate the patient’s temperature by adding blankets or removing layers of clothing. • Administer first aid quickly and efficiently. • Do not attempt to diagnose the patient or discuss the patient’s condition. • Avoid further injury if possible. EMERGENCY MEDICAL SERVICES • Emergency Medical Services (EMS) provides expert care for serious emergencies. • In many areas of the country, immediate help is available by dialing 911. • When calling for help, be sure to give complete and accurate information. • If you cannot call immediately, ask someone else to call for help. EMERGENCY CARE LEGAL ISSUES • The haste in which emergency care occurs often leaves the caregivers with little or no time to consider the legal consequences of their actions. • Emergency care professionals, other health care workers, and anyone else who has first aid training should be aware of some basic legal issues related to emergency care. THE GOOD SAMARITAN ACTS • State that physicians and first responders are not required to acquire patient consent before performing life-saving procedures in the case of an emergency. • To be protected by these Acts: ▫ Give care in good faith. ▫ Act within the scope of their training and knowledge. ▫ Use as much care as possible according to the circumstances. ▫ Do not bill the patient. SCOPE OF PRACTICE • Even a Good Samaritan Act cannot protect caregivers who perform procedures outside of their scope of practice. • Emergency care providers should only perform tasks for which they have been trained. KEEPING RECORDS • Event report after each emergency • This report includes: ▫ The patient’s name and address ▫ The date and time of emergency ▫ The location of emergency ▫ A description of the emergency and its cause ▫ A description of actions taken ▫ The names, addresses, and signatures of any witnesses ▫ The name and signature of the person preparing the report INJURY CARE TECHNIQUES DRESSINGS • A dressing is a sterile covering for a wound or injury. • Dressings are used to: ▫ ▫ ▫ ▫ stop bleeding prevent infection absorb secretions treat pain • Gauze pads are the most common materials used for dressings. However, in an emergency situation, any clean cloth can be used. BANDAGES • A bandage is material used to secure dressings and splints. • Tight enough to control bleeding and to hold dressings, but do not interrupt blood circulation • Three popular types of bandages are: ▫ Triangular ▫ Roller gauze ▫ Elastic TRIANGULAR BANDAGES • The triangular bandage is a triangular shape of cloth. It is often used for: ▫ Head and scalp injuries ▫ To create slings for shoulder, arm, wrist, and hand injuries • Triangular bandages can also be folded into cravats, which is a long strip of bandage folded to the proper width according to the injury. ELASTIC AND ROLLER GAUZE BANDAGES • Secure dressings and support injured areas. • Elastic bandages stretch and mold to the body. • Elasticity makes it easy to wrap an injury too tightly. SPLINTS • Rigid device that supports and immobilizes • Can be created using anything that will support the injured area. • Do not apply a splint if professional medical help is on the way. SLINGS • Keeps hand, forearm, arm, or shoulder immobilized • In combination with a cast or used in place of a cast or splint • Can be created using a triangular bandage. CRUTCHES • Help a patient ambulate • Used when unable to put weight on an injured or impaired leg, knee, ankle or foot. • Proper fit and use are important TYPES OF CRUTCHES • Axillary crutches • Forearm crutches • Platform crutches ADJUSTING CRUTCHES Crutches must fit patients correctly. CRUTCH GAITS • There are several types of crutch gaits. • • • • • Four-point Three-point Two-point Swing-to Swing-through SHOCK AND BONE/JOINT INJURIES SHOCK • Reduction of blood flow in the body • Often results from physical or emotional trauma • If left untreated, shock can be fatal, even in cases where the initial injury was not fatal. CAUSES OF SHOCK • Trauma causes shock. • Types of trauma that can cause shock include: ▫ ▫ ▫ ▫ ▫ ▫ ▫ ▫ ▫ Hemorrhage Severe pain Infection Heart attack Stroke Poison Lack of oxygen Dehydration Psychological trauma SYMPTOMS OF SHOCK • Shock has many symptoms, including: ▫ Pale, blue-gray skin color, especially under the nails and around the mouth ▫ Cool skin ▫ Rapid, weak pulse ▫ Irregular breathing ▫ Low blood pressure ▫ Anxiety or restlessness • Shock symptoms vary from patient to patient. TYPES OF SHOCK • Anaphylactic Shock • Cardiogenic Shock • Hemorrhagic Shock • Metabolic Shock • Neurogenic Shock • Psychogenic Shock • Respiratory Shock • Septic Shock TREATING SHOCK • Begin treatment immediately • There are several aims for treating shock, including: ▫ Eliminating or controlling the cause of shock ▫ Improving blood flow ▫ Providing oxygen ▫ Regulating body temperature BONE AND JOINT INJURIES • Include: • • • • fractures and breaks Dislocations Sprains strains FRACTURES • Fractures are breaks or cracks in a bone. ▫ Compound facture ▫ Simple fracture • Symptoms: Deformity Limited or loss of motion Pain and swelling Discoloration Protrusion of bone through the skin ▫ Hearing the bone break ▫ Grating sensation ▫ ▫ ▫ ▫ ▫ DISLOCATIONS • A dislocation occurs when a bone separates from a joint or is moved out of place in the joint. • Symptoms: ▫ Deformity ▫ Limited or abnormal movement ▫ Swelling ▫ Discoloration ▫ Pain ▫ Shortening or lengthening of the limb SPRAINS • A sprain is a stretch or tear in the ligaments and tendons around a joint. • Symptoms: ▫ ▫ ▫ ▫ Swelling Discoloration Pain Possibly limited motion STRAINS • A strain occurs when a muscle is overused or overstretched. Strain injuries are common in the back. • Symptoms: ▫ Sudden pain ▫ Swelling ▫ Bruising WOUNDS AND BURNS LESSON 1– WOUNDS • Injury that damages the body’s tissues • Watch for excessive bleeding and infection LESSON 1– SIGNS OF INFECTION • Redness • Swelling • Pain • Heat • Fever • Pus • Red streaks coming from the wound LESSON 1– CLOSED WOUNDS • Damage to the tissue under the skin • Caused when the body hits against a blunt object, such as in a bump or fall • Usually heal on its own in a few weeks LESSON 1– OPEN WOUNDS • Incisions - clean wounds with regular, smooth edges • Lacerations - rough, irregular wounds caused by jagged or blunt objects that crush or rip the skin • Abrasions - wounds in which the top layer of skin is rubbed or scraped off by a rough surface • Punctures - caused when a sharp object, such as a nail or needle, pierces a hole in the skin • Avulsions - wounds in which tissue is torn and separated from the body • Amputations - wounds in which a body part is completely cut off of the body. LESSON 1– MINOR OPEN WOUNDS • Shallow and produce very little blood • Not life-threatening and can be treated at home • Untreated, or improperly treated, minor wounds can become infected or can cause tetanus LESSON 1– MAJOR OPEN WOUNDS • It is important to act quickly when treating a patient with a major wound because a patient can bleed to death in a short period of time • Care for a major wound includes stopping the bleeding and then cleaning and covering. • When caring for major wounds, the health care worker should also check the patient’s vital signs, and watch for signs of shock. LESSON 2– BURNS • A burn is an injury caused by fire, heat, chemicals, radiation, or electricity. • Burns are traumatic in that they can cause extreme pain, permanent disfigurement, psychological problems, and even death. LESSON 2 – TYPES OF BURNS • Thermal • Chemical • Electrical LESSON 2– FIRST-DEGREE BURNS • First-degree burns: ▫ Superficial burns ▫ Most mild burn ▫ Damages only the epidermis • Symptoms: ▫ Hot, red, dry skin ▫ Mild Swelling ▫ Pain • Causes: ▫ Sunburn ▫ Brief contact with hot objects, steam, or weak acids LESSON 2– SECOND-DEGREE BURNS • Second-degree burns: ▫ Partial-thickness burns ▫ Affects the epidermis and the dermis • Symptoms: ▫ Blister or vesicle ▫ Skin appears wet and mottled ▫ Swelling • Causes: ▫ Boiling liquid and fire ▫ Extreme sunburn ▫ Artificial radiation LESSON 2– THIRD-DEGREE BURNS • Third-degree burns: ▫ Full-thickness burns ▫ Affects the epidermis, dermis, the tissue beneath the skin, and possibly the muscles and bones • Symptoms: ▫ White or charred skin • Causes: ▫ Fire and flames ▫ Extended contact with hot objects ▫ Exposure to electricity ▫ Immersion in a boiling substance LESSON 2– EXTENT AND SEVERITY OF BURNS • Burns are also categorized based on the extent and severity of the injury • The Rule of Nines ▫ Adults should get medical care if burns cover more than 15% of the body ▫ Children should get medical care if burns cover more than 10% of the body. • Another method for categorizing burns is a combination of the burn’s depth and its size. FOREIGN BODIES AND POISON LESSON 1– FOREIGN BODIES • Objects or substances that have entered the body and do not belong there • Range in seriousness from a simple splinter in a foot or finger to the lifethreatening situation of an object blocking a person’s airway • The location determines type of care LESSON 1– FOREIGN BODIES IN THE EYE • Common objects that can get into the eye include soap, beauty products, dirt, eyelashes, and insects. • Sharp objects that are lodged in the eye should be removed by a doctor. LESSON 1– FOREIGN BODIES IN THE EAR • Common objects that can get into the ear include insects, small objects, and chemicals. • Generally, objects in the outer part of the ear do not cause significant damage, and they often fall out when the head is gently shaken . • More stubborn objects can usually be removed with blunt tweezers or forceps. LESSON 1– FLUSHING OBJECTS FROM THE EAR • If an object cannot be removed from the ear using tweezers, the ear can be flushed with a few drops of warm oil or water. • If flushing the ear does not remove the object, then the patient should seek medical help. LESSON 1– FOREIGN BODIES IN THE NOSE • Common objects that can get into the nostrils include insects and chemicals that are accidentally inhaled. • Children are also famous for placing objects such as coins, buttons, pebbles, marbles and other small toys in their noses. • In most cases, the foreign body can be safely removed without medical help. LESSON 1– FOREIGN BODIES IN THE SKIN • Common objects that can get into the skin include splinters, insect stingers, and fish hooks. • In most cases, the foreign body can be safely removed without professional medical help. LESSON 2– POISONS • Any substance that causes injury, illness, or death when it enters or comes in contact with the body. • Poison may be swallowed, injected, inhaled, or absorbed through the skin. • Exact treatment for poisoning varies according to the substance, the amount, the way it enters the body, and whether the patient is conscious or unconscious. LESSON 2– THE POISON CONTROL CENTER • In most cases, poison does not enter the bloodstream right away, so fast action can prevent injury or death. • If a patient has swallowed or inhaled poison, the health care worker should call EMS or the local Poison Control Center immediately. • The Poison Control Center is prepared to help treat poison cases by giving specific instructions over the phone. LESSON 2– SIGNS OF POISONING • Symptoms of poisoning: ▫ Burns or redness around mouth and lips ▫ Breath that smells like chemicals ▫ Vomiting ▫ Difficulty breathing ▫ Sleepiness or confusion ▫ Dramatic changes in appearance or behavior LESSON 2– GATHER INFORMATION • What is the poisonous agent? • How did the poison enter the body? • How much poison entered the body? • What time did the poison enter the body? EXTREME TEMPERATURES LESSON 1– EXPOSURE TO HEAT • Overexposure can cause a chemical imbalance that prevents the body’s cooling system from working properly • Causes include: ▫ Being in extreme heat for too long ▫ Working or exercising on a hot day ▫ Illnesses, such as heart conditions, diabetes, and high blood pressure LESSON 1– HEAT CRAMPS • Heat cramps occur when a person perspires a lot, usually through working or exercising on a hot day. • A heat cramp is essentially a muscle cramp. • Symptoms: ▫ Muscle pain ▫ Muscle spasm LESSON 1– HEAT EXHAUSTION • Similar to heat cramps, heat exhaustion also occurs when the body loses too much water and salt through perspiration. • Symptoms: ▫ ▫ ▫ ▫ ▫ ▫ ▫ Pale and clammy skin Excessive perspiration Weakness and tiredness Headache Heat cramps Nausea and dizziness Vomiting or fainting LESSON 1– HEAT STROKE • A heat stroke occurs when heat causes high blood pressure and very high body temperature. • Symptoms: ▫ ▫ ▫ ▫ ▫ ▫ ▫ Red, dry, flushed skin Rapid, shallow breathing High temperature Fast, strong pulse Seizure Irritability and confusion Unconsciousness LESSON 2– EXPOSURE TO COLD • Cold temperatures cause the body to shiver, which helps to keep it warm. However, even shivering is unable to keep the body warm in some conditions. • Causes of exposure to cold include: ▫ Improper dress ▫ Immersion in very cold water ▫ An affect of illnesses LESSON 2– HYPOTHERMIA • A patient with hypothermia will have a temperature reading below 95°F. • Hypothermia can be caused by submersion in extremely cold water. It can also result from spending too much time in cool, damp environments. • Symptoms: ▫ ▫ ▫ ▫ ▫ ▫ Shivering Numbness Drowsiness Confusion Poor coordination Unconsciousness LESSON 2– FROSTBITE • Frostbite occurs when skin and the tissues and fluids beneath it freeze from exposure to extremely cold temperatures. • Symptoms: ▫ Redness and tingling ▫ Numbness and white or gray/yellow, glossy skin ▫ Blisters ▫ Confusion ▫ Fatigue and weakness ▫ Unconsciousness