Chapter 7 The Patellofemoral Articulation
advertisement

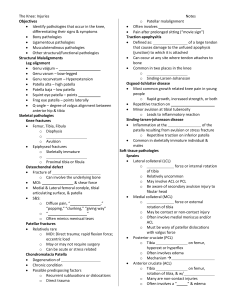
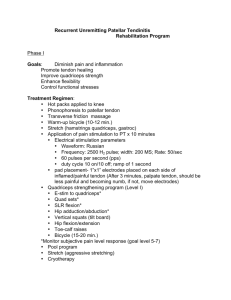
Chapter 7 The Patellofemoral Articulation Introduction Separated from the knee chapter because of differences in the mechanisms and onset of injury Injury is usually due to overuse, congenital malalignment, or structural insufficiency Clinical Anatomy Patella is largest sesamoid bone in body Anatomical design allows for: – – – Increased efficiency of quadriceps muscle group Protection of anterior portion of knee joint Absorption and transmission of patellofemoral joint reaction forces (forces transmitted through articular surfaces) Shape of patella – Figure 7-1, page 244 Clinical Anatomy Articular surface of patella – Figure 7-2, page 244 Patella tracks medially during range of 45o to 18o as knee moves from flexion to extension During final 18o of extension, patella tracks laterally During flexion and extension – patella tracks within femoral trochlear groove (between the 2 femoral condyles lined with articular cartilage) Clinical Anatomy Articulation of patellofemoral joint – Compressive forces – – Table 7-1, page 245 Walking: .5 times body weight Walking up/down stairs or running hills: 3.3 times body weight Lateral retinaculum – From vastus lateralis and IT band to lateral border Clinical Anatomy Medial retinaculum – Vastus medialis and adductor magnus to medial border Medial and lateral patellofemoral ligaments – Superior portion on fibrous capsule thickens and inserts on patella’s superior border Muscular Anatomy and Related Soft Tissue Quadriceps muscles – – Flexion – patella is pulled inferiorly by patella tendon’s attachment to tibial tuberosity Extension – quadriceps femoris and its tendon pull patella superiorly Length of patella is approximately same length as the long axis of the patella – Figure 7-4, page 245 Muscular Anatomy and Related Soft Tissue Vastus lateralis – pulls patella laterally Vastus medialis (VMO) – guides patella medially and prevents lateral patellar subluxation Tight IT band can accentuate the lateral tracking of patella, resulting in subluxations or patellar malalignment Muscular Anatomy and Related Soft Tissue Alignment of foot and normal flexibility of triceps surae and hamstring muscles are needed for adequate knee ROM and normal patellofemoral mechanics – Example: increased foot pronation = increased internal tibial rotation = rotation of tibial tuberosity toward midline Bursa of the Extensor Mechanism Varying numbers of bursa being directly involved with extensor mechanism 4 found consistently in population: – – – – – Suprapatellar bursa Prepatellar bursa Subcutaneous infrapatellar bursa Deep infrapatellar bursa Figure 7-5, page 246 Clinical Evaluation of the Patellofemoral Articulation Dysfunction of joints superior to or inferior to knee may manifest themselves as patellofemoral pain Patient preparedness Clinician preparedness History Mechanism and onset of injury – – Acute vs. chronic or insidious onset Chondromalacia Patella Softening and wearing away of patella’s hyaline cartilage; grinding Box 7-1, page 247 Clarke’s sign - Box 7-5, page 253 When pain occurs Location of pain History Level of activity Prior surgery Relevant past history Inspection Patella alignment – Patellar alignment – Patellar malalignment Figure 7-6, page 247 Box 7-2, page 248 Figure 7-7, page 247 Posture of knee – Genu varum, valgum, recurvatum Inspection Q angle – – – Tubercle sulcus angle – Relationship between line of pull of quadriceps and the patellar tendon Box 7-3, page 250 Box 7-4, page 251 Relationship between tibial tuberosity and inferior patellar pole Leg length difference Foot posture Areas of scars Palpation Refer to clinical proficiencies Utilize pages 249 – 253 Range of Motion Testing AROM – – – Flexion to extension = patella glides superiorly and somewhat laterally Tightness of lateral structures may accentuate lateral displacement Flexion = patella glides inferiorly and medially RROM – – Pain during movement may indicate malalignment Open and closed kinetic chain Range of Motion Testing Lower extremity flexibility – – Quadriceps, hamstrings, IT band, triceps surae Tightness may: Result in decreased functional ROM Force the quadriceps to exert more pressure on patella Cause patellar tracking deficits Ligamentous Testing Evaluate knee ligaments – Laxity in knee joint can result in abnormal patellar tracking, secondary to uniplanar or rotatory shifting of tibia or femur, causing patellofemoral pain Ligamentous and capsular stability of patella is based on presence of patellar tilt and amount of glide available to patella Ligamentous Testing Patellar Glide – – Patellar Tilt – Figure 7-9, page 254 Box 7-6, page 255 Box 7-7, page 256 Synthesis of Findings – Relationship between patellar glide and tilt Neurologic Testing Same as described in Chapter 6 Pathologies and Related Special Tests “patellofemoral dysfunction” and “patellofemoral pain syndrome” used to describe wide range of symptoms Onset may occur during inactivity (theater knee) and/or during or after activity Differentiation between meniscal and patellar pain – Table 7-2, page 257 Evaluation Map – page 257 Patellofemoral Pain Syndrome All-inclusive diagnosis for pain in and around the joint that cannot be explained by a specific pathology Signs and symptoms – – – – Insidious onset; occasionally caused by trauma Primary complaint of anterior knee pain caused by activity, pain may be constant Stair climbing, sitting for long periods swelling Patellofemoral Pain Syndrome Signs and symptoms continued – – – Pain increased with AROM and RROM Surrounding tissues evaluate for tightness and hyperlaxity by assessing patellar glide and tilt Assess subtalar joint Treatment – – Modify activity, NSAIDs, ice, patellar mobilization and passive stretching, flexibility and strength training Orthotics, patellar taping Patellar Maltracking Normal tracking depends on relationships between: – – – – – Alignment of femur on tibia Q angle Integrity of soft tissue restraints Foot mechanics Flexibility of triceps surae, quads, hamstrings, IT band Table 7-3, page 258 Patellar Maltracking Predisposing factors: – – – – Congenital dysfunction Injury to patella or knee Increased body weight Gait mechanics Gradual onset of symptoms Redistribution of forces along patellar facets – Pain during ADLs Patellar Subluxation and Dislocation Acute, chronic, or congenital laxity of medial patellar restraints or abnormal tightness of lateral retinaculum results in increased lateral glide of patella – Predisposes patient to subluxation or dislocation Subluxations can occur without patient knowing it Dislocations shift patella laterally and lock out of place, obvious deformity and quadriceps spasm – Figure 7-10, page 259 Patellar Subluxation and Dislocation Most apt to dislocate or subluxate within 20 to 30 degrees of knee flexion or after valgus blow to knee May result in fractured patella, osteochondral damage, bone bruises, osteochondritis dissecans Multiple incidences result in wearing of articular cartilage Patellar Subluxation and Dislocation Predisposing factors – – – – Hypomobile medial glide Flattened posterior articulating surface External tibial rotation and hyperpronated feet increase Q angle Family history Patellar Subluxation and Dislocation Evaluative Findings – Apprehension Test – Table 7-4, page 260 Box 7-8, page 261 Radiographic examination Rule out MCL sprain Treatment – Conservative vs. surgical Patellar Tendinitis Insidious onset – Acute onset – Jumping activities, running sports, weight lifting Blow to tendon Repetitive motions on a biomechanically malaligned extensor mechanism can result in unequal loads on the extensor mechanism – Microtearing of fibers Patellar Tendinitis Most common site of pain = inferior pole – Evaluative Findings – Pain at superior pole = quadriceps tendinitis (jumpers knee) Table 7-5, page 262 MRI may be useful Conservative vs. surgical treatment Patellar Tendon Rupture Predisposing factors – – – Rheumatoid arthritis, diabetes, lupus, chronic renal disease, gout Chronic inflammation of tendon Corticosteroid medications Tension developed within quadriceps unit overloads the patellar tendon, resulting in rupture in midsubstance or avulsion from patella or patellar tuberosity Patellar Tendon Rupture Evaluative Findings – Table 7-6, page 262 No ligamentous stability tests should be performed until examined by physician Treatment – – – Immediate immobilization and transport Surgical intervention within 7 to 10 days Rehabilitation to restore knee function; full return to activity in 12 months Patellar Bursitis Bursa inflamed secondary to: – – – – Evaluative Findings – – Single traumatic blow Repeated low-intensity blows Overuse Infection (redness, warmth, refer to physician) Table 7-7, page 264 Figure 7-11, page 263 Treatment – modify activity & control inflammation Synovial Plica Fold of the fibrous membrane that projects into joint cavity During maturation, folds are absorbed into capsule; however, in majority of population, a thickened area or crease remains Remains asymptomatic until area is traumatized Most commonly affects medial joint capsule Synovial Plica When symptomatic, plica loses elastic properties and alters biomechanics of patellar gliding mechanism Evaluative Findings – Test for medial plica syndrome – Table 7-8, page 264 Box 7-9, page 265 Stutter Test – Box 7-10, page 266 Synovial Plica Confirmed through MRI Treatment – – – Modify activity Control inflammatory response Strengthen VMO to lessen symptoms by reducing tensile forces placed on plica Osgood-Schlatter Disease Adolescent inflammatory condition that strikes the tibial tuberosity’s growth plate where patellar tendon attached Onset due to repeated avulsion fractures of tendon from its attachment; caused by rapid growth and/or increased quad strength – Results in osteochondritis of tubercle Osgood-Schlatter Disease Evaluative Findings – Table 7-9, page 267 Figure 7-12 page 266 Conservative treatment by reducing activity, controlling inflammation – Surgical intervention if conservative treatment fails Sinding-Larsen-Johansson Disease Found at attachment of tendon into inferior patellar pole (or quad tendon at proximal pole) Caused by stress fracture or avulsion because of repetitive forces associated with running and jumping Affects males more often, ages 10-14 yrs Sinding-Larsen-Johansson Disease Evaluative Findings – Treatment – – – – Table 7-10, page 268 Rest, immobilization Decrease inflammation Modalities, NSAIDs Stretching and strengthening May be symptomatic until maturation Patellar Fracture Blunt trauma May rupture of bursa; palpation reveals crepitus or false joint – Figure 7-13, page 268 Active knee extension and passive knee flexion produce severe pain Resisted knee extension cannot be performed due to pain On-Field Evaluation of Patellofemoral Injuries Equipment considerations On-field History On-field Palpation On-field Functional Tests – – Willingness to move the involved limb Willingness to bear weight Initial Management of On-Field Injuries Patellar Tendon Rupture – – Gross deformity, immediate loss of function Splint in extension and transport Patellar Dislocation – – – Obvious deformity Reduction should not be attempted; spontaneous reduction may occur Splint in position if not reduced, in extension if reduced; transport Figure 7-14, page 270