BIO 121 * Molecular Cell Biology Lecture Section IV A. Cells in the
advertisement
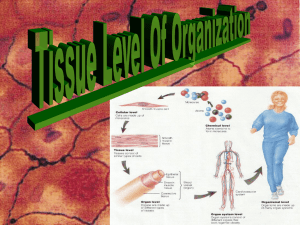
BIO 121 – Molecular Cell Biology Lecture Section IV A. Cells in the Context of Tissue, Organ and Organismal Architecture B. Wound Healing Four Types of Vertebrate Tissue 1.Epithelium 2.Connective Tissue 3.Muscle 4.Nervous Tissue 1. Architecture of Epithelium • Simple, Stratified, Pseudostratified, Transitional • Squamous, Cuboidal, Columnar • Ciliated or not • Examples: – – – – Small Intestine = Simple Columnar Epithelium Trachea = Ciliated Pseudostratified Columnar Epithelium Blood Vessel = Simple Squamous Epithelium Skin = Stratified Squamous Epithelium Structure equals Function – Small Intestine: Simple Columnar Epithelium = absorption – Trachea: Ciliated Pseudostratified Columnar Epithelium = filtering debris – Blood Vessel: Simple Squamous Epithelium = gas exchange – Skin: Stratified Squamous Epithelium = protective physical barrier Simple, Columnar Epithelium Function: 1. absorption of nutrients 2. enzymatic digestion at neutral pH 3. multiple defensive mechanisms 4 Cell types in Small Intestine Small Intestine Cellular Adhesion in Small Intestine Desmosomes Hemidesmosomes Adherens Junctions Occluding Junctions Tracheal Epithelium Ciliated Pseudostratified Columnar Epithelium with Goblet Cells 1. Mucus traps dust and airborne microorganisms 2. Ciliar waving gets rid of unwanted material The Vasculature: Simple, Squamous Epithelium Gas Exchange Fluid Exchenge Epidermis of Skin Stratified Squamous Epithelium Creates tough, waterproof barrier Differentiation and Direction of Movement in Epidermis Cornification is the overproduction of cytokeratins, ECM and the adhesions to a degree that stops cellular metabolism. 2. Mesenchymal Cell Types and Connective Tissues Figure 23-52 Molecular Biology of the Cell (© Garland Science 2008) The Fibroblast Loose Connective Tissue Dense Regular CT Dense Irregular CT Elastic Connective Tissue The dermis is as complex as the epidermis and contributes greatly to skin function Cartilage and the Chondrocyte Lacunar Structure of the Hyaline Cartilage Extremely low blood flow Osteoblasts Lacunar structure of the long bones Cortical Bone vs. Spongy Bone Cell Types of the Bone Marrow of Long Bones has Stem Cells Start out as cartilage models built by chondrocytes Chondrocytes hypertrophy, calcify and die Osteoblasts and osteoclasts finish up The Adipocyte Mesenchymal Stem Cells are a continuous source of adipocytes 3. Contractile Tissue Figure 23-47a Molecular Biology of the Cell (© Garland Science 2008) Arteries, veins Lymphatic vessels Gastrointestinal tract Respiratory tract Urinary bladder Reproductive tract Urinary tract Iris of the eye Erector pili of skin 4. Nervous Tissue Nerve Bundles Cutaneous Wound Healing The skin is a complex organ... Many cells and activities involved Many cells and activities involved in Healing Clotting Scarring Re-establishing Function • Four overlapping stages to wound healing – Hemostasis – Inflammation – Proliferation – Maturation Blood flows into the exposed ECM of the injured tissue. RBC and Platelets Trapped in Fibrin Clot Clotting factor VII from the blood contacts tissue factor on cells in the damaged tissues to activate clotting Platelet activation in the. clot makes them sticky and releases their signal storage vesicles ©2000 by Lippincott Williams & Wilkins Camacho A , Dimsdale J E Psychosom Med 2000;62:326-336 Positive feedback activates even more Platelet activation releases growth factors by regulated secretion Inflammation is a process mediated primarily by WBC as part of our innate immunity - Resident mast cells and macrophages - Recruited monocytes and neutrophils Resident mast cells also degranulate rubor = redness calor = heat tumor = swelling dolor = pain Activated mast cell activities Figure 1 Development and differentiation of macrophages. Rickard A J , Young M J J Mol Endocrinol 2009;42:449-459 © 2011 Society for Endocrinology Activated macrophage activities Neutrophil Diapedesis Activated neutrophils are phagocytic Proliferation re-establishes tissue function • Reconnection of the dermal connective tissue • Integrity of the epidermal layers • Re-establishment of blood flow Reconnection of the dermal CT Cell Migration or “Crawling” • The Basic Mechanism – – – – Triggered by signals from outside the cell Actin-myosin based movement Requires attachments to outside to pull against Gotta’ drag all of the cell contents along for the ride Chemotaxis Circumferential receptors Rho-family GTPases (monomeric) Rho-dependent kinases 1. Actin monomer nucleotide exchange 2. Actin fiber polymerization and disassembly 3. Myosin motor ATPase activity Figure 17-62 (part 1 of 3) Molecular Biology of the Cell (© Garland Science 2008) Formation of the scar matrix 1. 2. 3. 4. glycosaminoglycans proteoglycans fibrous proteins elastic proteins Re-establishment of the epidermal epithelium involves both mitosis and epithelial migration Also must reform the basal lamina Re-epithelialization below the scab scar Fi Model depicting α3β1-integrin-mediated functions of epidermis that contribute to wound healing. Mitchell K et al. J Cell Sci 2009;122:1778-1787 ©2009 by The Company of Biologists Ltd Figure 23-34 Molecular Biology of the Cell (© Garland Science 2008) Maturation Phase Wound contraction by myofibroblasts Stitches Perform Wound Contracture Collagen Remodeling A scar never reaches the strength of undamaged tissue Healing Abnormalities • Failure to heal: Excessive Inflammation • Excessive scarring: Wound Fibrosis – Hypertrophic Scarring – Keloid Scarring Biofilms May Block Healing Hypertrophic scars result from failed fibroblast contracture Don’t extend beyond the original wound edge Keloid scars result from excessive TGF-b receptors on fibroblasts Extend to fibroblasts outside the wound People have exploited these conditions to create the ‘keloid tattoo’