23-2
advertisement

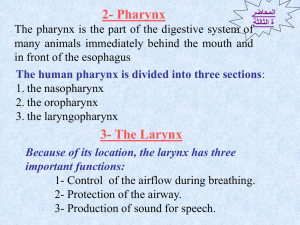
The Respiratory System • Cells continually use O2 & release CO2 • Respiratory system designed for gas exchange • Cardiovascular system transports gases in blood • Failure of either system – rapid cell death from O2 starvation Human Lungs 23-2 Respiratory System Anatomy • • • • • • • Nose Pharynx = throat Larynx = voicebox Trachea = windpipe Bronchi = airways Lungs Locations of infections – upper respiratory tract is above vocal cords – lower respiratory tract is below vocal cords Trachea • Size is 5 in long & 1in diameter • Extends from larynx to T5 anterior to the esophagus and then splits into bronchi • Layers – mucosa = pseudostratified columnar with cilia & goblet – submucosa = loose connective tissue & seromucous glands – hyaline cartilage = 16 to 20 incomplete rings • open side facing esophagus contains trachealis m. (smooth) • internal ridge on last ring called carina (cough reflex) – adventitia binds it to other organs Histology of the Trachea • Ciliated pseudostratified columnar epithelium • Hyaline cartilage as C-shaped structure closed by trachealis muscle 23-5 Trachea and Bronchial Tree Airway Epithelium • Ciliated pseudostratified columnar epithelium with goblet cells produce a moving mass of mucus. Bronchi and Bronchioles • • • • Primary bronchi supply each lung Secondary bronchi supply each lobe of the lungs (3 right + 2 left) Tertiary bronchi supply each bronchopulmonary segment Repeated branchings called bronchioles form a bronchial tree Histology of Bronchial Tree • Epithelium changes from pseudostratified ciliated columnar to nonciliated simple cuboidal, and finally to simple squamous as pass deeper into lungs • Incomplete rings of cartilage replaced by rings of smooth muscle & then connective tissue – sympathetic NS & adrenal gland release epinephrine that relaxes smooth muscle & dilates airways – asthma attack or allergic reactions constrict distal bronchiole smooth muscle Lobules 23-10 Structures within a Lobule of Lung • Branchings of single arteriole, venule & bronchiole are wrapped by elastic CT • Respiratory bronchiole – simple squamous • Alveolar ducts surrounded by alveolar sacs & alveoli – sac is 2 or more alveoli sharing a common opening Histology of Lung Tissue Photomicrograph of lung tissue showing bronchioles, alveoli and alveolar ducts. Cells Types of the Alveoli • Type I alveolar cells – simple squamous cells where gas exchange occurs • Type II alveolar cells (septal cells) – free surface has microvilli – secrete alveolar fluid containing surfactant • Alveolar dust cells – wandering macrophages remove debris Alveolar-Capillary Membrane • Respiratory membrane = 1/2 micron thick • Exchange of gas from alveoli to blood • 4 Layers of membrane to cross – – – – alveolar epithelial wall of type I cells alveolar epithelial basement membrane capillary basement membrane endothelial cells of capillary • Vast surface area = handball court Details of Respiratory Membrane Double Blood Supply to the Lungs • Deoxygenated blood arrives through pulmonary trunk from the right ventricle • Bronchial arteries branch off of the aorta to supply oxygenated blood to lung tissue • Venous drainage returns all blood to heart Breathing or Pulmonary Ventilation • Air moves into lungs when pressure inside lungs is less than atmospheric pressure – Increase volume of lungs, Boyle’s law • Air moves out of the lungs when pressure inside lungs is greater than atmospheric pressure – Passive process • Atmospheric pressure = 1 atm or 760mm Hg Boyle’s Law • As the size of closed container decreases, pressure inside is increased, inverse relationship • The molecules have less wall area to strike so the pressure on each inch of area increases. Dimensions of the Chest Cavity • Breathing in requires muscular activity & chest size changes • Contraction of the diaphragm flattens the dome and increases the vertical dimension of the chest • Contraction of external intercostal muscles elevates ribs and increases diameter of chest Inspiration • Diaphragm moves 1 cm & ribs lifted by muscles • Intrathoracic pressure falls and 2-3 liters inhaled Expiration • Passive process with no muscle action • Elastic recoil & surface tension in alveoli pulls inward • Alveolar pressure increases & air is pushed out Summary of Breathing • Alveolar pressure decreases & air rushes in • Alveolar pressure increases & air rushes out Alveolar Surface Tension • Thin layer of fluid in alveoli causes inwardly directed force = surface tension – water molecules strongly attracted to each other • Causes alveoli to remain as small as possible • Detergent-like substance called surfactant produced by Type II alveolar cells – lowers alveolar surface tension – insufficient in premature babies so that alveoli collapse at end of each exhalation Pneumothorax • Pleural cavities are sealed cavities not open to the outside • Injuries to the chest wall that let air enter the intrapleural space – causes a pneumothorax – collapsed lung on same side as injury – surface tension and recoil of elastic fibers causes the lung to collapse 23-24 Lung Volumes and Capacities • Tidal volume = amount air moved during quiet breathing • MVR= minute ventilation is amount of air moved in a minute • Reserve volumes ---- amount you can breathe either in or out above that amount of tidal volume • Residual volume = 1200 mL permanently trapped air in system • Vital capacity & total lung capacity are sums of the other volumes Dalton’s Law • Each gas in a mixture of gases exerts its own pressure – as if all other gases were not present – partial pressures denoted as p • Total pressure is sum of all partial pressures – atmospheric pressure (760 mm Hg) = pO2 + pCO2 + pN2 + pH2O External Respiration • Gases diffuse from areas of high partial pressure to areas of low partial pressure • Exchange of gas between air & blood • Deoxygenated blood becomes saturated • Compare gas movements in pulmonary capillaries to tissue capillaries Internal Respiration • Exchange of gases between blood & tissues • Conversion of oxygenated blood into deoxygenated • Observe diffusion of O2 inward – at rest 25% of available O2 enters cells – during exercise more O2 is absorbed • Observe diffusion of CO2 outward Hemoglobin 4 heme molecules each bind one oxygen molecule 23-29 Oxygen Transport in the Blood • Oxyhemoglobin contains 98.5% chemically combined oxygen and hemoglobin – inside red blood cells • Does not dissolve easily in water – only 1.5% transported dissolved in blood • Only the dissolved O2 can diffuse into tissues • Factors affecting dissociation of O2 from hemoglobin are important Carbon Dioxide Transport • 100 ml of blood carries 55 ml of CO2 • Is carried by the blood in 3 ways – dissolved in plasma – combined with the globin part of Hb molecule forming carbaminohemoglobin – as part of bicarbonate ion • CO2 + H2O combine to form carbonic acid that dissociates into H+ and bicarbonate ion Smokers Lowered Respiratory Efficiency • Smoker is easily “winded” with moderate exercise – – – – – nicotine constricts terminal bronchioles carbon monoxide in smoke binds to hemoglobin irritants in smoke cause excess mucus secretion irritants inhibit movements of cilia in time destroys elastic fibers in lungs & leads to emphysema • trapping of air in alveoli & reduced gas exchange 23-32