Genital Lesion
advertisement

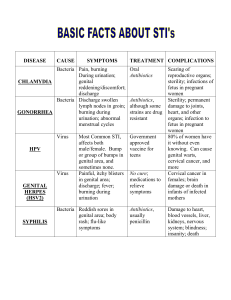
Genital Lesion By: Group B Contents: 1. 2. 3. 4. 5. 6. 7. 8. Introduction Herpes simplex virus (II) Granuloma inguinalae Soft chancer Candidiasis Human papilloma virus Syphilis Management and prevention Introduction: • Genital sores may be painful, itchy, produce a discharge, or cause no symptoms at all. • Because genital lesions or sores can have a negative affect on a person's self-image, many people do not seek proper medical care. All genital sores should be evaluated by a medical professional. • Itching, painful urination, or painful sexual intercourse often occur with genital lesions. Herpes simplex virus (II) Herpes simplex virus (II) • Associated with genital infections , young sexually active adults mainly. • The primary lesions are: An erythematous plaque which is often noted initially, followed soon by grouped vesicles, which may evolve to pustules; these become eroded. Erosions are punched out and may enlarge to ulcerations. • Incubation period: o 2-7 days • Lesions appear on the: I. Glans or penile shaft in of males II. Uvula in females III. Herpes lesions may found around the anus also (in case of homosexual men) Group of vesicles with early central crusting on a red base arising on the shaft of the penis. • shallow ulcers on the edematous vulva and perineum. Micturition is often very painful. Associated inguinal lymphadenopath y is common. • Anal type of HSV(II) • Lesions are painful associated with: headache, myalgia, Fever, local lymphadenopathy. • Paraesthesiae may develop (urinary retention., constipation). • Skin and mucosal lesions resolves within 2-3 weeks • Recurrent genital herpes: with milder and shorter manifestations and more localized lesions (after exposure to sunlight, UV light, trauma to sensory nerves). Neonatal HSV(II) infection : • Occurs during parturition when the mother has genital herpes (primary type). • Clusters of vesicles , start to appear after few day to several weeks after birth.. • Complications: o Encephalitis o Pneumonia o Hepatitis (with high mortality). Management : • 5 days of oral Acyclovir topical cream or systemic treatment (200 mg, 5 times per day )+ analgesics and saline baths • For recurrence hygiene is all that required, in addition to counseling and prevention of transmission Granuloma inguinalea Granuloma inguinale: • Granuloma: is a nodular type of inflammatory reaction. • Inguinale: refer to inguinal region. • It’s also known as donovanosis after the donovans bodies which are diagnostic sign. • It’s bacterial disease caused by klebsiella granumatis. • Characterized by ulcerative genital lesions and the ulcers ultimately progress to destruction of internal and external tisse with extensive leakage of mucus and blood from highly vascular lesions. • The ulcer can be mistaken for sypillis. Symptoms: 1. Small, painless nodules, later the nodule burst creating open fleshy, oozing lesions. 2. The lesions typically found on the shaft of the penis, the labia, or the perineum. 3. In contrast to syphilitic ulcer there’s no lymphadenopathy. Transmission: • The organism transmitted from one host to another through contact with open sores. • Diagnosis: 1. Patient’s sexual history. 2. Physical examination revealing painless, beefy red ulcer with granulation tissue edge. 3. Tissue biopsy confirm the presence of donovan bodies. Treatment: 1. three weeks of treatment with: erythromycin streptomycin or tetracycline. 2. Or 12 weeks of treatment with: ampicillin. • Prevention: 1. 2. Avoidance of sexual contact in endemic regions. Sexually transmitted disease (STD) testing before beginning of sexual relationship. Chancroid Chancroid: • also known as soft chancre. • Is a bacterial sexually transmitted infection characterized by painful sores on the genitalia. • Chancroid is known to spread from one individual to another through sexual contact • Is a bacterial infection caused by the fastidious Gram – ve Haemophilus ducreyi • It is a disease found primarily in developing countries. Pathogenesis: • H. ducreyi enters skin through microabrasions incurred during sexual intercourse. A local tissue reaction leads to development of erythomatous papule, which progresses to pustule in 4–7 days. It then undergoes central necrosis to ulcerate. Symptoms and signs: These are only local and no systemic manifestations are present The ulcer characteristically : 1. 2. 3. 4. 5. 6. 7. 8. Ranges in size dramatically from 3 to 50 mm (1/8 inch to two inches) across Is painful Has sharply defined, undermined borders Has irregular or ragged borders Has a base that is covered with a gray or yellowish-gray material Has a base that bleeds easily if traumatized or scraped Painful lymphadenopathy occurs in 30 to 60% of patients. Dysuria (pain with urination) and dyspareunia (pain with intercourse) in females • The initial ulcer may be mistaken as a "hard" chancre, the typical sore of primary syphilis, as opposed to the "soft chancre" of chancroid. • Approximately one-third of the infected individuals will develop enlargements of the inguinal lymph nodes • Half of those who develop swelling of the inguinal lymph nodes will progress to a point where the nodes rupture through the skin, producing draining abscesses. The swollen lymph nodes and abscesses are often referred to as buboes. Diagnosis: By laboratory findings : 1. From bubo pus or ulcer secretions , H.ducreyi can be identified 2. PCR-based identification of organisms is available 3. Simple, rapid, sensitive and inexpensive antigen detection methods for H. ducreyi identification are also popular. 4. Serologic detection of H. ducreyi is and uses outer membrane protein and lipooligosaccharide. Comparison with syphilis: Chancroid lesion typical of infection with the bacterium Haemophilus ducreyi Chancre lesion typical of infection with the bacterium that causes syphilis, Treponema pallidum typically painful typically painless have a grey or yellow purulent exudate non-exudative have a soft edge have a hard (indurated) edge CHANCROID CHANCRE Treatment: • Single oral dose (1 gram) of Azithromycin, or a single IM dose of Ceftriaxone, or oral Erythromycin for seven days. • Abscesses are drained. Genital Candidiasis Candidiasis: • Candidiasis or thrush is a fungal infection (mycosis) of any species from the genus Candida , Candida albicans is the most common agent of Candidiasis in humans. • Candidiasis may be divided into: 1. Mucosal candidiasis 2. Cutaneous candidiasis 3. Invasive candidiasis Candidal vulvovaginitis: Up to 75% of women will have this infection at some point in their lives, and approximately 5% will have recurring episodes , It is the second most common cause of vaginal inflammation after bacterial vaginosis. • The Candida species of fungus is found naturally in the vagina, and is usually harmless, Symptoms of thrush can also be caused by Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis. • Symptoms: 1. 2. 3. 4. 5. Vulval itching. Vulval soreness and irritation. Superficial dyspareunia. Dysuria. vaginal discharge, which is usually odourless,This can be thin and watery, or thick and white, like cottage cheese. Diagnosis Candidal balanitis: • Not common. • Candidal balanitis, infection of the glans penis, almost exclusively occurring in uncircumcised males. • Symptoms of infection of the male genitalia include red, patchy sores near the head of the penis or on the foreskin, severe itching, or a burning sensation. Candidiasis of the penis can also have a white discharge, although uncommon. Treatment: • Candidiasis is commonly treated with antimycotics; these antifungal drugs include topical clotrimazole, topical nystatin, fluconazole, and topical ketoconazole. • A one-time dose of fluconazole is 90% effective in treating a vaginal yeast infection, Local treatment may include vaginal suppositories or medicated douches. Prevention: General advice: 1. Routine recommendation of use of vulval moisturisers as soap substitute and regular skin conditioner . 2. Loose-fitting, natural fibre underwear. 3. Avoidance of topical irritants. 4. Good hygiene. Human papilloma virus Human papilloma virus: • Genital warts may occur singly but are more often found in clusters. • They may be found anywhere in the anal or genital area, and are frequently found on external surfaces of the body, including the penile shaft, scrotum, labia majora of the vagina, or around the anus • They can also occur on internal surfaces like the opening to the urethra, inside the vagina, on the cervix, or in the anus. In males they are frequently found on or around the head of the penis. • They can be as small as 1-5mm in diameter, but can also grow or spread into large masses in the genital or anal area. In some cases they look like small stalks. • They may be hard ("keratinized") or soft. Their color can be variable, and sometimes they may bleed. In most cases, there are no symptoms of HPV infection other than the warts themselves • Sometimes warts may cause itching, redness, or discomfort, especially when they occur around the anus. Although they are usually without other physical symptoms, an outbreak of genital warts may cause psychological distress, such as anxiety, in some people Syphilis Definition: • Syphilis is an infectious disease caused by the spirochete Treponema pallidum. • It is almost always transmitted by sexual contact with infectious lesions. • But can be transmitted in utero and via blood transfusion. The Great Pox • Epidemic in late 15th century Europe • Rapid spread and severe symptoms in early stages • Epidemic coincided with Columbus’ return from America in 1493 o ? A gift from the new world Treponema pallidum Clinical Presentation Syphilis Acquired Primary Secondary Congenital Tertiary Primary Syphilis: • Chancre: o Appears 10-90 days after infection o Typically single, painless, clean-based lesion with rolled edges Secondary Syphilis: • Signs and Symptoms: o Usually occurs 3-6 weeks after primary chancre: 1. 2. 3. 4. 5. 6. 7. 8. Rash (75-90%). Generalized lymph node swelling (70-90%). Constitutional symptoms (50-80%). Mucous patches (5-30%). Condyloma lata (5-25%). Patchy alopecia or hair loss (10-15%). Symptoms of neurosyphilis (1-2%). Less common: meningitis, hepatitis, arthritis, nephritis. Tertiary Syphilis: • 70% of untreated patients remain asymptomatic. • 30% of untreated patients progress to tertiary stage in 520 years: 1. Gummas: destructive lesions of soft tissue, cartilage, internal organs and bone. 2. Cardiovascular involvement: aortic aneurysm, aortic insufficiency. 3. Central nervous system involvement: general paresis, tabes dorsalis, optic atrophy. • Progressive inflammatory disease. Diagnostic Tests for Syphilis: 1. Darkfield / DFA-TP 2. VDRL/RPR 3. FTA-abs Treatment of Syphilis: • PCN is drug of choice for treatment of all stages of syphilis. • HIV testing is recommended in all patients • PCN-allergic; Tetracycline 500mg for 14 days Management and prevention: Management: • Prevention offers the best approach to managing STIs. • Not all genital ulcer cause by STIs there for; there are specific tests for evaluation of the genital ulcer. • The specific tests include: 1. Syphilis serology for T.pallidum. 2. Culture or antigen test for HSV. 3. Biopsy of genital ulcers that are un usual or that don't respond to initial therapy. 4. HIV/AIDS test. • the health care providers frequently must treat patient before test results are available. Prevention: • The most effective way to prevent transmission of STIs is to avoid sexual intercourse with an infected partner. • Ideally both new partner should get test for STIs before initiating sexual intercourse. • • • • • • • Correct use of condom and safer sex practice. Immunization: against hepatitis B. Reduce mother to child transmission . Ensure safety of the blood for transfusion. Vaccination: HPV vaccine Avoid sharing the under clothes. Education about STIs. Thank you Group members: • • • • • • • • • • عمرو عبدالعزيز بابكر امير مكي عوض اواب محمد عيد اشرف ادم صالح عمار احمد علي ايمن سليمان برهان علي تكريم داليا احمد بابكر ابتهال كمال ابتهال كرار • • • • • • • • • • دعاء االمين فاطمة النور ايماء احمد دالل نورالدين امنة عبدالسالم امتثال محمد حسين ايمان الفاضل فاتن احمد ايناس حسن اليمامة اسحق