Antibiotics: An Overview

Antibiotics: An Overview
Pre-Test
Which statements are true about E.coli?
a) It is a Gram positive bacteria.
b) It is a Gram negative bacteria.
c) It is a bacteria normally found in the colon. d) It is the most common cause of a UTI.
e) It can cause diarrhea.
Pre-Test
The 6 year old boy has high volume watery diarrhea that looks like ‘rice in water’. He is dehydrated. You resuscitate him with IV normal saline. What is the best antibiotic treatment?
a) Penicillin G or Penicillin V b) Ampicillin or Amoxicillin c) Doxycycline or Erythromycin d) Cefalexin or Cefazolin
Pre-Test
A 3-year old child is brought to the emergency. The child is irritable and complains of a headache. On exam, the child has a fever of 39ºC and has neck stiffness. You are worried about meningitis. What antibiotic should you consider?
a) Metronidazole b) Ciprofloxicillin c) Cefazolin d) Cloxicillin e) Ceftriaxone
Pre-Test
What statements are true about rickettesia?
a) Typhus fever is caused by rickettesia.
b) Rickettesia is an atypical bacteria. c) Rickettesia can be treated with doxycycline.
d) Rickettesia can be treated with tetracycline.
e) Rickettesia can be treated with chloramphenicol.
Pre-Test
A 20-year old male comes in with 2 week history of general malaise and recurrent fever. He recently developed a papular rash on his chest. His abdomen is tender and distended. The patient should be treated with: a) Ampicillin for a probable UTI.
b) Levofloxacin for a probable lobar pneumonia.
c) Cloxicillin for a probable Staphylococcus rash.
d) Ceftriaxone for probable Salmonella typhi.
e) No antibiotics.
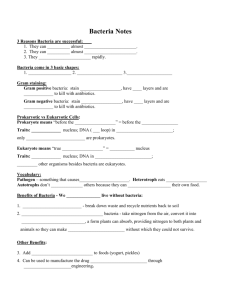
Types of Microorganisms that cause Infectious Disease
Bacteria
Protozoa
Fungi
Helminths
Viruses
Types of Microorganisms that cause Infectious Disease
Bacteria
Single cell organism with cell wall
No nucleus / Has circular DNA within cell
Protozoa (ie. Plasmodium, Entamoeba, Giardia)
Single cell organism with nucleus
Fungi: Yeast (ie. Candida albicans)
Helminths: Worms
Viruses
Not a cell, but are DNA or RNA wrapped in protein coat
They reproduce by taking over an animal cell and reproducing
Types of Microorganisms that cause Infectious Disease
Antibiotics treat bacteria and protozoans
Type of Bacteria
TYPICAL Bacteria
Gram positive
Gram negative
ATYPICAL Bacteria
Acid fast
No cell wall
Intracellular (lives inside host cells)
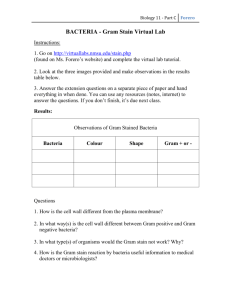
Gram Stains
Divides bacteria into 2 groups
Gram positive
Gram negative
Based on cell wall differences
Detects peptidogylcan which is a part of the cell wall
Gram positive = THICK peptidoglycan layer
Gram negative = Thin petidoglycan layer
Detects shape of bacteria
Cocci - circle
Bacillus - rod (straight or curved)
Spirochete - spiral
What color are the gram positive bacteria on gram stain?
Can you give some examples of
Gram + and Gram –
BACTERIA?
Gram positive Gram negative
Can you give some examples of
Gram + and Gram –
BACTERIA?
Gram positive
Staphylococcus
Streptococcus
Enterococcus
Clostridium
Gram negative
E. coli
Klebsiella
Hemophilus
Pseudomonas
Niesseria
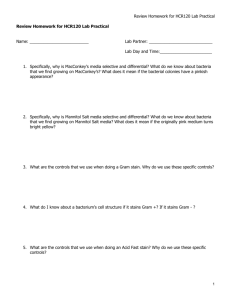
Classification of Bacteria
Typical Bacteria Atypical Bacteria
Gram + Gram -
Cocci Rod Cocci Rod
Acid fast
No cell wall
Spiral
Mycobacterium
Treponema Mycoplasma
Intracellular
Clostridium
(anaerobic)
Niesseria
Staphylococcus
Streptococcus
Enterococcus
Straight Curved
E.coli
Salmonella /Shigella
Proteus / Enterobacter
Klebsiella
Hemophilus
Bordetella
Pseudomonas
Bacteroides (anaerobic)
Vibrio
Campylobacter
Helicobacter
Rickettsia
Chlamydia
Protozoans
Examples:
Plasmodium: malaria
Entamoeba histolytica: dysentery and liver abscesses
Giardia intestinalis: diarrhea
Trichimonal vaginalis: STI
Types of Antibiotics
Beta-Lactams
Sulpha drugs
Fluroquinolones
Aminoglycocides
Tetracyclines
Macrolides
Beta-Lactam Antibiotics
Detects peptidogylcan which is a part of the cell wall
Gram positive = thick peptidoglycan layer
Gram negative = thin petidoglycan layer
Inhibit the synthesis of peptidoglycan cell wall of bacteria
The peptidoglycan layer is important in cell wall structure, especially in Gram positive bacteria
Can you give some examples of beta-lactam antibiotics?
Beta-Lactam Antibiotics
Types of beta-lactam antibiotics
Penicillins
Cepalosporins
Penicillins
There are different kinds of penicillins
Each kind has slightly different bacterial coverage
Can you give me some names of penicillins that you have heard of?
Penicillins
Natural penicillins
Penicillin G (IM or IV)
Penicillin V (PO)
What bacteria do the natural penicillins cover?
Penicillins
Natural penicillins
Penicillin G (IM or IV)
Penicillin V (PO)
What bacteria does it cover?
Some Gram +
Streptococci
Enterococci
Few Gram -
Neisseria
Penicillins
Aminopenicillins
Ampicillin
Amoxicillin
What bacteria does it cover?
Penicillins
Aminopenicillins
Ampicillin
Amoxicillin
What bacteria does it cover?
Some Gram +
Streptococcus
Enterococci
More Gram – than natural penicillins
E. Coli, Salmonella, Shigella, Hemophilus
Penicillins
Anti-staphylococcal penicillins
Cloxacillin
Methicillin
What bacteria does it cover?
Penicillins
Anti-staphylococcal penicillins
Cloxacillin
Methicillin
What bacteria does it cover?
More Gram +
Staphylococcus
Streptococcus
No enterococcus
No Gram - coverage
Penicillins
Extended Spectrum
Piperacillin
What bacteria does it cover?
Penicillins
Extended Spectrum
Piperacillin
What bacteria does it cover?
Some Gram +
Streptococcus
Enterococcus
Staphylococcus if tazobactam added
Most Gram –
E. coli, Klebsiella, Proteus, Pseudomonas
Anaerobic bacteria
Cephalosporins
Divided into 4 generations
As generation increases
Decreasing Gram + activity
Increasing Gram – activity
3 rd generation cephalosporins can penetrate the CNS
(so use these for meningitis)
What cephalosporin antibiotics do you know?
Cephalosporins: Examples
1 st generation
Cefalexin, Cephalothin, Cefazolin, Cefadroxil
2 nd generation
Cefuroxime, Cefaclor, Cefprozil, Cefoxitin
3 rd generation
Ceftriaxone, Ceftazidime, Cefotaxime, Cefixime
Cephalosporin coverage
Gram + Staph
Strep
Gram Proteus
E. coli
Klebsiella
Hemophilus
Enterobacter
Neisseria
Pseudomonas
1 st gen. 2 nd gen 3 rd gen
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
Y
(Y)
Trimethoprim-Sulfamethoxazole
What bacteria does it cover?
Trimethoprim-Sulfamethoxazole
Gram positive
Staphylococcus
Weak Streptococcus coverage
Gram negatives
E. coli, Klebsiella, Proteus
Salmonella, Shigella
Hemophilus
Side effects: Rash, allergy, Bone marrow suppression
Fluoroquinolones
2 types
Ciprofloxacin
Good Gram -
Good atypical coverage: Mycoplasma, Chlamydia
No Gram +
Respiratory Fluoroquinolones (levofloxacin, moxifloxacin)
Good Gram –
Better Gram +, especially Streptococcus
Moxifloxacin also good for anaerobes
Good antibiotic choice for respiratory infections
Aminoglycosides
Gentamicin, Tobramycin
Activity
Good Gram –
No Gram + or Anaerobic coverage
Side effects
Hearing loss (permanent)
Renal failure (reversible)
Tetracyclines
Tetracycline, Doxycycline
Activity
Better Gram + than Gram –
Good for atypical bacteria: Rickettsia, Chlamydia
Good for protozoans: Plasmodium, Entamoeba
In children (<8 years old) can cause permanent teeth staining
Macrolides
Erythromycin, Clarithromycin, Azithromycin
Activity
Some Gram +: Streptococci
Some Gram -: Hemophilus, Neisseria, Campylobacter
Atypicals: Mycoplasma, Chlamydia, Rickettsia
Mostly for respiratory and soft tissue infections
Antibiotics against anaerobes
Clindamycin
Good Gram positive coverage:
Staphylococcus
Streptococcus
Good Gram negative anaerobic coverage:
Bacteroides
Poor Gram negative aerobic coverage
Used for:
Skin and soft tissue infections
Pelvic and Intraabdominal infections (in combination with other antibiotics that cover Gram negative bacteria)
Antibiotics against anaerobes
Metronidazole
Good anaerobic coverage
Bacteroides, Clostridium
Good protozoal coverage
Entamoeba, Giardiasis
Use: Intraabdominal and pelvic infections (in combination with other antibiotics to cover anaerobic Gram -)
Good for Clostridium difficile (diarrheal infection especially in patients who have received antibiotics for another reason)
Chloramphenicol
Activity
Gram +: Staphylococci, Streptococci, Clostridium
Gram -: Hemophilus, Neisseria, E. coli, Vibrio, Salmomella
Side effects
Bone marrow toxicity; Pancytopenia
Common uses
Typhoid fever
Scrub typhus / Rickettsia
Meningitis
Summary
Antibiotics should be chosen based on what the most likely bacteria are causing the disease and what antibiotics will target those bacteria
Case 1
Diagnosis?
Common Bacteria?
Case 1
Diagnosis?
Common Bacteria?
Streptococci
Staphylococci
Treatment?
Case 1
Diagnosis?
Common Bacteria?
Streptococci
Staphylococci
Treatment?
Penicillins
Amoxicillin
Cloxacillin
1 st gen cephalosporin
Case 2: Meningitis
What are common bacteria?
Case 2: Meningitis
What are common bacteria?
Streptococcus pneumoniae
Neisseria meningitidis
Hemophilus influenzae
Listeria monocytogenes
Treatment?
Case 2: Meningitis
What are common bacteria?
Streptococcus pneumoniae
Neisseria meningitidis
Hemophilus influenzae
Listeria monocytogenes
Treatment?
High dose Ceftriaxone (2g IV q12 h)
Add Ampicillin if age > 50 for Listeria
Case 2: Quality Assurance
A 20year old male presents with fever, chills, severe headache, and neck stiffness
He traveled 6 hours to get to the hospital
When he arrives, he is drowsy and BP is 100/60. He waits in the emergency room for another 2 hours
A medical student sees him first, but is not sure what to do, so waits to discuss with the teacher who arrives 1 hour later
In the meantime, the patient becomes hypotensive, has a seizure, and loses consciousness
Case 2: Quality Assurance
Why did the patient deteriorate so quickly?
Case 2: Quality Assurance
Why did the patient deteriorate so quickly?
Delaying antibiotics in meningitis increases risk of death and irreversible neurologic deficits
Case 2: Quality Assurance
What could have been done differently to improve patient care?
By the student?
By the teacher?
By the hospital/ health care system?
Case 3
Probable Diagnosis?
Case 3
Probable Diagnosis?
Lobar Pneumonia
Common bacteria?
Case 3
Common bacteria?
Streptococcus pneumoniae
Mycoplasma, Chlamydia
Hemophilus (if chronic lung disease)
Treatment?
Outpatients
In patients
Case 3
Common bacteria?
Streptococcus pneumoniae
Mycoplasma, Chlamydia
Hemophilus (if chronic lung disease)
Treatment?
Outpatients
Doxycycline
Amoxicillin
2 nd gen cephalosporin
In patients
Ceftriaxone + macrolide
Levofloxacin or Moxifloxacin
Case 4: Urinary Tract Infection
What are common bacteria?
Case 4: Urinary Tract Infection
What are common bacteria?
E. coli** (Most common)
Proteus
Klebsiella
Treatment?
Case 4: Urinary Tract Infection
What are common bacteria?
E. coli** (Most common)
Proteus
Klebsiella
Treatment?
TMP-SMX
Ciprofloxacin
Amoxicillin/Clavulanate
Ceftriaxone if severe
Aminoglycosides if severe
Case 5: Bloody Diarrhea
Common bacteria?
Case 5: Bloody Diarrhea
Common bacteria?
Salmonella
Shigella,
Campylobacter
E. coli
These are all Gram negatives
Treatment?
Case 5: Bloody Diarrhea
Salmonella Fluoroquinolone , Ceftriaxone
More resistance to TMP-SMX, Macrolides, and Amoxicillin
Shigella Fluoroquinolone , Ceftriaxone
More resistance to TMP-SMX, Macrolides, and Amoxicillin
Campylobacter Fluoroquinolone
All are resistant to TMP-SMX, Penicillins, and Cephalosporins
E. coli No antibiotics
Case 6
Diagnosis?
Case 6
Diagnosis?
Bacteria?
Scrub typhus
Rickettsia family
Treatment?
Case 6
Diagnosis?
Bacteria?
Scrub typhus
Rickettsia family
Treatment?
Doxycycline
Chloramphenicol
Tetracycline
Case 7
Patient presents with:
Fever, Relative bradycardia
Develops abdominal pain and rash
Diagnosis?
Case 7
Patient presents with:
Fever, Relative bradycardia
Develops abdominal pain and rash
Diagnosis?
Bacteria?
Salmonella typhi (Gram negative)
Treatment?
Case 7
Patient presents with:
Fever, Relative bradycardia
Develops abdominal pain and rash
Diagnosis?
Bacteria?
Salmonella typhi (Gram negative)
Treatment?
Ciprofloxacin
Ceftriaxone
Post Test
Which statements are true about E.coli?
a) It is a Gram positive bacteria.
b) It is a Gram negative bacteria.
c) It is a bacteria normally found in the colon. d) It is the most common cause of a UTI.
e) It can cause diarrhea.
Post Test
A 6 year old boy has high volume watery diarrhea that looks like ‘rice in water’. He is dehydrated. You resuscitate him with IV normal saline. What is the best antibiotic treatment?
a) Penicillin G or Penicillin V b) Ampicillin or Amoxicillin c) Doxycycline or Erythromycin d) Cefalexin or Cefazolin
Post Test
A 3-year old child is brought to the emergency. The child is irritable and complains of a headache. On exam, the child has a fever of 39ºC and has neck stiffness. You are worried about meningitis. What antibiotic should you consider?
a) Metronidazole b) Ciprofloxicillin c) Cefazolin d) Cloxicillin e) Ceftriaxone
Post Test
What statements are true about rickettesia?
a) Typhus fever is caused by rickettesia.
b) Rickettesia is an atypical bacteria. c) Rickettesia can be treated with doxycycline.
d) Rickettesia can be treated with tetracycline.
e) Rickettesia can be treated with chloramphenicol.
Post Test
A 20-year old male comes in with 2 week history of general malaise and recurrent fever. He recently developed a papular rash on his chest. His abdomen is tender and distended. The patient should be treated with: a) Ampicillin for a probable UTI.
b) Levofloxacin for a probable lobar pneumonia.
c) Cloxicillin for a probable Staphylococcus rash.
d) Ceftriaxone for probable Salmonella typhi.
e) No antibiotics.
Questions