Assessment_Protocol
advertisement
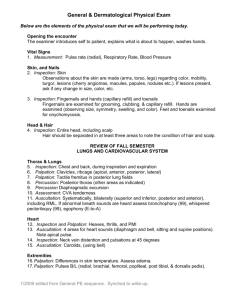
Assessment Protocol Dr. Michael Gillespie Doctor of Chiropractic Anatomic and Biomechanical Principles It is necessary to understand normal anatomy and healthy biomechanical relationships to accurately evaluate orthopedic and neurological conditions. Understand the relationship between structure and function. Anatomical and biomechanical variants can be present with a particular patient. Clinical Assessment Protocol Patient History Inspection / observation Palpation Range of Motion Orthopedic and Neurologic Testing Diagnostic Imaging Functional Testing Documentation Evaluate progress. Share information with other practitioners. Insurance records. Malpractice. SOAP Notes Subjective – Patient History Objective – Observation and Testing Assessment – Based on compilation of findings Plan – Further testing and / or treatment Patient History A thorough patient history can often lead to a proper diagnosis with no further testing. Emphasize the aspect of the patient history with the greatest clinical significance. Acquire all of the patient’s history whether or not something seems relevant at the time. Patient History Keep the patient focused on the problem. Listen carefully. Do not lead the patient towards answers. Closed-Ended History Question and Answer Format. Written Forms Open-Ended History Dialogue between patient and examiner. Identify other problems that are either directly or indirectly related to the presenting complaint. Address the patient’s fears and concerns. Develop rapport. Keep the patient focused on the presenting problem. OPQRST Mnemonic Onset of complaint Provoking or Palliative concerns Quality of pain Radiation to particular areas Site and Severity of complaint Time frame complaint History – Other Factors Family History Occupational History Social History Observation / Inspection General Appearance Functional Status Body Type Postural deviations Gait Muscle guarding Compensatory movements Assistant devices Inspection – three layers Skin Subcutaneous tissue Bony structure Skin Inspection Bruising Scarring Trauma or surgery Changes in color Vascular changes of inflammation Vascular deficiency – pallor or cyanosis Pigmented areas / Hairy areas Change in texture Open wounds – traumatic or insidious Detection of Malignant Melanoma Asymmetry MM lack symmetry Irregular Borders MM have notched, indented, scalloped, or indistinct borders Color Changes MM have uneven coloration, may contain several colors Diameter MM are typically greater than 6mm (0.25 in) Elevation Subcutaneous Soft Tissue Inspection Evaluate for inflammation and swelling Atrophy Increase in size Edema, articular effusion, muscle hypertrophy Nodules, lymph nodes, or cysts Compare b/l symmetry, utilize circumferential measurements Bony Structure Inspection Evaluate bony structure when gait or range of motion is altered. Evaluate the spine Scoliosis Kyphosis Lordosis Pelvic tilt Shoulder height Evaluate for congenital and traumatic bone deformities Genu Varus Genu Valgus Palpation Palpate the patient in conjunction with inspection. Begin with a light touch. Dysesthesia. Hypoesthesia. Hyperesthesia. Anesthesia. Skin Palpation Evaluate skin temperature High – inflammation Low – vascular insufficiency Adhesions Subcutaneous Soft Tissue Palpation Subcutaneous soft tissue – fat, fascia, tendons, muscles, ligaments, joint capsules, nerves, blood vessels. Palpate with more pressure than with skin. Palpate for tenderness and swelling or edema. Tenderness Grading Scale Grade I - Patient complains of pain Grade II - Patient complains of pain and winces Grade III - Patient winces and withdraws the joint Grade IV – Patient will not allow palpation of the joint Types of Swelling Immediately after injury, hard and warm Contains blood 8 to 24 hours after an injury, boggy or spongy Contains synovial fluid Tough and dry Callus Types of Swelling Thickened and leathery Chronic swelling Soft and fluctuating Acute Hard Bone Thick and slow moving Pitting edema Pulse Palpate for pulse rate, rhythm, and amplitude Normal healthy resting pulse rate for an adult is 60 – 100 bpm Palpating Bony Structures Detection of alignment problems Dislocations, luxations, subluxations, fractures Identify ligaments and tendons that attach to the bones Detect bony enlargements Range of Motion Passive Active Resisted Passive Range of Motion The examiner moves the body part without the patient’s help. Note normal, increased, or decreased movement. Note pain. Capsular or ligamentous lesion on side of movement and / or muscular lesion on side opposite of movement. Six Range of Motion Pain Variations 1. Normal mobility with no pain. No lesion – normal joint. 2. Normal mobility with pain. Minor ligament sprain or capsular lesion. 3. Hypomobility with no pain. Adhesion. Six Range of Motion Pain Variations 4. Hypomobility with pain. Acute ligament sprain or capsular lesion. Guarding from muscle spasm. 5. Hypermobility with no pain. Complete tear with no fibers intact where pain can be elcited. 6. Hypermobility with pain. Partial tear with some fibers still intact. Sprain Vs. Strain Sprain - A sprain is an injury involving the stretching or tearing of a ligament (tissue that connects bone to bone) or a joint capsule, which help provide joint stability. Strain - Strains are injuries that involve the stretching or tearing of a musculo-tendinous (muscle and tendon) structure. End Feel Evaluate for end feel after determining the degree of passive range of motion. Passively move the joint to the end of its range of motion and then apply slight overpressure to the joint. Active Range of Motion Yields information regarding the patient’s general ability and willingness to use a body part. Assessment value is limited. Note the degree of motion as well as pain elicited. Crepitus should be noted. Inclinometers and goniometers are used to measure range of motion. Inclinometer Goniometer Resisted Range of Motion Resisted range of motion assesses musculotendinous and neurologic structures. Musculotendinous injuries tend to be more painful than they are weak. Neurologic injuries tend to be more weak than they are painful. Muscle Grading Scale 5 – Complete range of motion against gravity with full resistance. 4 – Complete range of motion against gravity with some resistance. 3 – Complete range of motion against gravity. 2 – Complete range of motion with gravity eliminated. 1 – Evidence of slight contractility. 0 – no evidence of contractility. Resistant Range of Motion Reactions Strong with no pain – Normal. Strong with pain – lesion of muscle or tendon. Weak and painless – neurological lesion or complete rupture of a tendon or muscle. Weak and painful – partial tear of muscle or tendon. Fracture, neoplasm, and acute inflammation are possibilities.