Chapter 43
advertisement

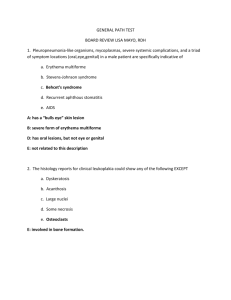
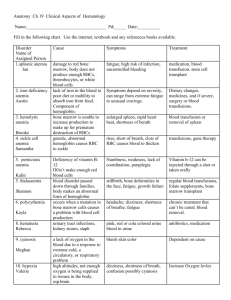
NUR 240 Hematological Stressors JBorrero 10/09 Charting Chuckles 1. She has no rigors or shaking chills, but her husband states she was very hot in bed last night 2. Patient has chest pain if she lies on her left side for over a year. 3. On the second day the knee was better, and on the third day it disappeared. 4 . The patient is tearful and crying constantly. She also appears to be depressed 5. The patient has been depressed since she began seeing me in 1993 6. Discharge status: Alive but without my permissio 7. Healthy appearing decrepit 69-year-old male, mentally alert but forgetful. 8. The patient refused autopsy. 9. The patient has no previous history of suicides. 10. While in ER, she was examined, x-rated and sent home Topics • Anemias resulting in decreased production of RBC’s Pernicious anemia Iron deficiency anemia Folic acid deficiency anemia Aplastic anemia • Polycythemia Vera • Leukemia-CML/CLL • Blood transfusion procedures and reactions Anatomy and Physiology Review • Bone marrow • Blood components Red blood cells (erythrocytes) White blood cells (leukocytes) Thrombocytes (platelets) • Accessory organs of hematopoiesis Spleen Liver Kidneys Bone Marrow Hematopoiesis Erythrocytes • • • • • • RBCs are largest proportion of blood cells Flexible membrane, no nucleus Normal count 4-6 million Lifespan 120 days Produce Hgb Kidneys produce RBC growth factor:erythropoietin Erythrocyte Depletion • Iron deficiency anemia • B12/folic acid deficiency • Pernicious anemia • Aplastic anemias • • • • Sickle cell anemia G6PD Acute blood loss Chronic blood loss Anemia • Result of a condition in which the function or number of RBCs is inadequate to meet tissue oxygen demands. • Insufficient function of RBCs: B12, Iron, Folic Acid deficiencies • Reduction in either the number of red blood cells, the amount of hemoglobin, or the hematocrit • Clinical sign (not a specific disease); a manifestation of several abnormal conditions • Tissue hypoxia is the underlying cause of all symptoms accompanying anemia WBCs or Leukocytes Involved with inflammation and immunity Look for “differential” on WBC count Granulocytes-increase rapidly in presence of infection 1. Monocytes- Macrophages- 1st line of defense 2. Neutrophils- 2nd line of defense 3. Basinophils- help mediate allergic reactions 4. Eosinophils- antiparasitic, limits local inflammation Lymphocytes • B-lymphocytes- antibody mediated immunity • T-lymphocytes- cell mediated immunity Platelets • Smallest of blood cells • Stick to injured blood vessel walls to form platelet plugs • Perform most of their function by aggregation • 80% platelets circulate, 20% stored in spleen Assessment • • • • • • • Family history and genetic risk Personal history Diet history Socioeconomic status HPI Physical Exam Dx Testing Physical Assessment • • • • • • • • • Skin Head and neck Respiratory Cardiovascular Renal and urinary Musculoskeletal Abdominal Central nervous system Psychosocial Diagnostic Assessment Tests of cell number and function: – – – – – Complete blood count Reticulocyte count Differential Coombs’ test Serum ferritin, transferrin, and total ironbinding capacity Coagulation Studies Bone Marrow aspiration/biopsy CAT Scans CBC with Differential WBC RBC HGB HCT MCV,MCH, MCHC Platelets Neutrophils, Eosinophils, Basophils, Lymphocytes (T&B), Monocytes Reticulocytes Count 4.5-11.0 3.80-5.20 11.7-15.7 35.0-47.0% 140K-440K Differential 0.5-2.5% total RBC Tests Measuring Bleeding and Coagulation • • • • • Bleeding time test Prothrombin time (PT) International normalized ratio (INR) Partial thromboplastin time (PTT) Platelet agglutination/aggregation Bone marrow aspiration and Bx • Done when other tests show persistent abnormal results • Results will show bone marrow function • Aspiration • Biopsy Preparation • • • • • • • • • • Physician’s order Consent & Vital Signs Performed at bedside/lab Procedure takes 5-15 minutes Provide support/accurate info Local anesthetic/rapid acting sedative May feel pressure/pushing/pain May feel stinging/burning sensation Site: ileac crest is most common Sterile precautions Follow-up Care • Give client education. • Cover with pressure dressing; observe for 24 hours. • Administer mild analgesic (ASA free) • Apply ice pack. • Avoid contact sports or any activity that might result in trauma to the area. NCLEX TIME • After a bone marrow aspiration, the nurse questions which post procedure order? • A.Administer aspirin for pain • B.Apply ice packs to the puncture site. • C.Administer acetaminophen for discomfort. • D.Maintain sandbag on puncture site until bleeding stops NCLEX TIME In reviewing laboratory data in a client, the nurse recognizes which hematologic change associated with aging? • A.Decreased red blood cells • B.Decreased platelets • C.Increased hemoglobin • D.Increased white blood cells Goals of tx for anemias • • • • • Enhance tissue perfusion Minimize O2 demand Maintain CO Prevent hypovolemia Minimize complications of therapy Iron Deficiency Anemia • This common type of anemia can result from blood loss, poor intestinal absorption, or inadequate diet. • Evaluate adult clients for abnormal bleeding. • Supplemental iron is the treatment. • Microcytic- RBC cell size is smaller than normal Vitamin B12 Deficiency Anemia Pernicious Anemia • Anemia is caused by inhibiting folic acid transport and reducing DNA synthesis in precursor cells. • B12 transports Folic Acid into RBC precursor cell • Pernicious anemia is anemia caused by failure to absorb vitamin B12 by lack of intrinsic factor Etiology: Vitamin B12 deficiency is a result of poor intake of foods containing vitamin B12. OR Intrinsic Factor deficiency Vitamin B12 Deficiency Anemia S&S- paresthesias, loss of coordination, smooth, beefy, sore, bright red tongue weight loss and fatigue, pallor DX test: Schilling Test-24hr urine Tx: Pernicious Anemia: Vitamin B12 (Cyanocobalamin) injections Poor dietary intake: Increase intake of liver/organ meats, dried beans. Citrus fruits, eggs , green leafy vegetables Folic Acid Deficiency Anemia • Can cause megaloblastic anemia • Manifestations similar to those of vitamin B12 deficiency, but nervous system functions remain normal Folic Acid Deficiency Anemia • Caused by: – Poor nutrition and chronic alcohol abuse – Malabsorption syndromes, such as Crohn’s disease – Drugs, including anticonvulsants and oral contraceptives, that slow or prevent absorption of folic acid – Tx- Folic Acid Nursing Interventions for B12 and Folic Acid Deficiency Anemias • • • • Assess VS, labs, pulse ox Provide care for oral mucous membranes Administer B12 IM, Folic Acid Teach about disease process and selfinjection • Pace activities • Eliminate alcohol intake • Diet modification Aplastic Anemia • Deficiency of circulating erythrocytes • Injury to the hematopoietic precursor cell • Usually leukopenic and thrombopenic as well: PANCYTOPENIC ETIOLOGY: chronic toxic exposure, viral, 50% idiopathic CLINICAL MANIFESTATIONS: Medical Management • Immunosuppressive tx • Splenectomy • Bone marrow transplant Anemias from Blood Loss • ACUTE • Severed blood vessels due to trauma • Rupture of aneurysm • • • • • Tx • Tx CHRONIC Peptic ulcers Excessive menses Bleeding hemorrhoids Polycythemia Vera • Malignant disease with a sustained increase in blood hemoglobin • Massive production of red blood cells • Excessive leukocyte production • Excessive production of platelets • Blood viscosity and blood volume increased • Severe congestion of all tissues and organs Etiology • Usually unknown (idiopathic) • Sometimes caused by other conditions such as COPD, high altitudes, heart failure • Bone marrow produces more RBCs to prevent hypoxia Clinical Manifestations • • • • • • • • Hypertension Epistaxis, Ecchymosis, Hemorrhage Complications of MI, CVA Headaches Red, dark, flushed hands & skin Splenomegaly and Hepatomegaly Intense itching Distended superficial veins Treatment • Phlebotomy- keep Hct<45 • Myelosuppressive agents- suppress bone marrow • Radiation tx • Hydration • Promote venous return • Encourage oral fluids • Encourage ambulation • Anticoagulation therapy Leukemia • Type of cancer with uncontrolled production of immature white blood cells in the bone marrow • Invade and destroy bone marrow • Metastasize to liver, spleen, lymph nodes, testes and brain • Acute or chronic • Classified by cell type- lymphocytic vs. myelocytic • Patients are vulnerable to infection and anemia Etiology Exact cause is unknown Risk factors: ionizing radiation exposure to certain chemicals and drugs genetic factors immunologic factors treatment for other types of cancer Classification of Leukemia • Acute- can die in days to 6mos without appropriate tx Acute Lymphocytic Leukemia Acute Myelogenous Leukemia • Chronic- gradual onset, can live 5 years or more without tx Chronic Lymphocytic Leukemia Chronic Myelogenous Leukemia Clinical Manifestations • • • • • • • Neuro CV Resp MS GI GU Integumentary • • • • • Signs of bleeding Signs of anemia Lymphadenopathy CBC abnormal Signs of infection Definitive Test Examination of cells obtained from bone marrow aspiration and biopsy Nursing Diagnoses Risk for Injury Alteration in oral mucus membranes Alteration in nutrition, less Grieving Nausea Bleeding Fatigue Risk for infection Acute or chronic Pain Risk for Infections • Infection is a major cause of death in the client with leukemia, and sepsis is a common complication. • Cross-contamination GOAL: prevent, treat and control infection Infection Prevention • “Minimal bacteria diet” without uncooked foods • Monitoring of daily laboratory results • Assessment of vital signs • Skin care, respiratory care • Prevent and manage stomatitis • Teach pt to care for CVAD Protective Isolation • Frequent handwashing • Private room • HEPA filtration or laminar airflow system • Mask for visitor with upper respiratory infection • Institute precautions for pt with low platelet count Treatment for Leukemia: Chemotherapy Intensive/combo at time of dx. Goal: Remission SIDE EFFECTS: Bone marrow suppression N/V/D Alopecia Stomatitis Kidney/liver/cardiac toxicity Leukemia Treatment • • • • • • • • • Radiation tx Antibiotics, anti-virals, anti-fungal agents Interferon/ Interlukin Neupogen Epogen, Procrit, Diet tx PRBC- leukocyte depleted transfusion Patient education Emotional support Side Effects of RT/CT • • • • • Drug induced pancytopenia Severe N&V Skin problems at site of RT Impaired hepatic function Permanent sterility for males with RT to pelvic area • Secondary Ca development Bone Marrow Transplantation • Standard treatment for leukemia • Before procedure, CT and total body irradiation • Purges present marrow of the leukemic cells • After conditioning, new, healthy marrow given to the client toward a cure Types of BMT • Allogeneic • Syngeneic • Autologous Complications of BMT 1.Failure to engraft 2.Graft vs host disease (GVHD) 3.Bleeding / Infection 4.Fatigue 5.Venocclusive disease Blood Transfusions Types of Blood Products • Red blood cell • Platelet transfusions • Plasma transfusions: fresh frozen plasma • Cryoprecipitate • Granulocyte (white cell) transfusions *Review typing/crossmatching *Review ABO Compatibilities Blood Products: Transfusion Therapy Pretransfusion responsibilities to prevent adverse transfusion reactions: – Verify prescription. – Test donor’s and recipient’s blood for compatibility. – Examine blood bag for identification. – Check expiration date. – Inspect blood for discoloration, gas bubbles, or cloudiness. Nursing Interventions • Explain procedure • Get signed consent • Start transfusion within 30 minutes of arrival from blood bank • IV access: What size angiocath? • Y tubing, filter and which fluid? • Check blood with another RN • Obtain Vital Signs • Teach patient to report any untoward symptoms • Premedicate if necessary Transfusion Responsibilities • Provide client education. • Assess vital signs. • Begin transfusion slowly and stay with client first 15 to 30 minutes. • Ask client to report unusual sensations such as chills, shortness of breath, hives, or itching. • If reaction occurs: STOP TRANSFUSION • Change tubing, call MD, call blood bank. Get urine/blood samples. Send blood bag to lab Transfusion Reactions • Clients can develop any of the following transfusion reactions: – Hemolytic – Allergic – Febrile – Bacterial – Circulatory overload Autologous Blood Transfusion • Collection and infusion of client’s own blood • Eliminates compatibility problems; reduces risk for transmission of bloodborne disease • Preoperative autologous blood donation • Intraoperative autologous transfusion • Postoperative blood salvage