Case Discussions Challenges in End of Life Care
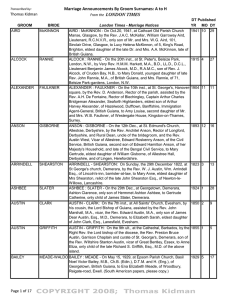
advertisement

Case Discussions Challenges in End of Life Care 15/11/14 MRS B Visit request Mon Afternoon (temp resident) From daughter: Brought Mum to stay with me Has Renal cancer Tired/Sleepy Not Just Eating/drinking not herself MRS B History from daughter Age 77 , Temp Resident RENAL CANCER, LUNG METS Diagnosed 8/12. Palliative Rx , 12/12 prognosis PMH Hypothyroid Medication Levothyroxine, Oxycontin/Oxynorm Allerg: Dexamthazone History and exam Mrs B Feeling generally unwell Hardly eating/drinking/ no nausea Left rib pain few weeks Aware prognosis- Preferred Place of Care = Hospice Pale, looks dry, bit confused Obs normal, abd mass ↓A/E chest, urine NAD Discussion with Mrs B and daughter Daughter struggling Mrs B will consider admission to Hospice but nowhere else BUT NO FEMALE BEDS IN HOSPICE WHAT DO YOU DO NOW? Discussion Differential Patient’s Carer’s diagnosis wishes wishes WHAT HAPPENED NEXT? Urgent bloods requested (done next day) Referred to ERT Next day Increased confusion and reduced mobility Still no Hospice bed available WHAT NEXT ? Patient Admitted to hospital Then bloods phoned through Calcium Albumin ALP Bilirubin ALT GGT CRP Urea Creat Egfr Hb WBC NEUTS 3.34 32 245 9 7 62 38 9.3 90 47 94 25.6 22 (2.20-2.60) (35-60) (30-130) (<21) (< 35) (<35) (<5) (2.5-7.8) (50-130) (>60) (118-148) (3.5-11) (2.0-7.5) Other tests in Hospital CT Head – normal CT Chest/Abdomen/Pelvis – Increase in renal mass and pulmonary metastases MRI Spinal Cord No spinal cord compression Evidence of rib invasion from metastases Urine/ Blood Cultures – negative TREATMENT: IV Fluids IV Bisphosphontes Confusion settled Mobility improved Discharged to own home.