Chapter 11: Water and the Major Minerals
advertisement

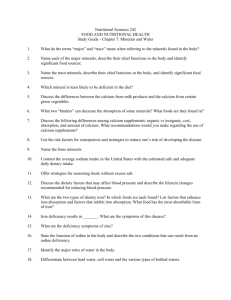
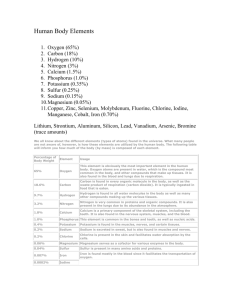
Chapter 9: Water and the Major Minerals Water: Essential Nutrient Death occurs – Without food – Without vitamins, minerals – Without water Water Comprises 50-70% of the body Muscle contains 73% water (fat contains ~20%) Intracellular fluid – Fluid within the cell (2/3 of total) Extracellular fluid – Outside the cells (1/3 of total) Water Content Varies By Tissue Lean muscle Fat Bones Water Content Varies: By Age Newborn Adult Elderly Water Content Varies Daily Salt intake Hormonal 2 cups fluid = 1 pound Kidneys excrete excess Functions of Water Almost universal solvent Dissolves – Nutrients – Wastes – Urea – Carbon dioxide Functions of Water Removal of body waste – – – – – Via urine Excrete 1-2 quarts/day Urea excretion Sodium excretion Avoid concentrated urine 21/2 cups --- dark yellow Can promote kidney stones Functions of Water Body temperature regulation – Metabolism generates heat – Buildup is dangerous – Water absorbs any excess heat – Body secretes fluid via perspiration – Skin is cool as perspiration evaporates Functions of Water Lubricant – Joints – Synovial fluid Shock absorber – Amniotic fluid – Cerebrospinal fluid Are You Drinking Enough? Recommend 1ml per 1kcal ½ oz / pound body weight Daily Water Losses Urine – largest loss Skin –ongoing evaporation Lungs – vapor Feces Sources of Water Fluids – Water – Other beverages Food – Fruits and vegetables – Meat – All but dried foods Metabolism – Energy nutrients → carbon dioxide, The Thirst Mechanism Not reliable Concerns for infants, older adults, athletes Athletes need to monitor their fluid status Weigh themselves before and after training Goal is to consume 3 cups for every pound lost Ignoring Thirst Shortage of water in the body Increase fluid conservation Antidiuretic hormone – From the pituitary glad – Forces the kidney to conserve water (reduce urine flow) Aldosterone – Responds to the drop in blood pressure – Signals the kidney to retain sodium (water) Thirst Signal is not triggered until person loses 1%-2% of body weight in fluid Lost of 4% causes muscle to lose significant strength and endurance Lost of 10%-12% causes heat intolerance Lost of 20% results in coma and death Dark yellow urine is a sign of inadequate fluids Water Safety Most municipal tap water is safe The Environmental Protection Agency and local municipalities look for contaminants Power to local and state authorities to advise public Water Safety Chlorine and ammonia are added to kill most microbes Small cancer risk (2/1 million people) Chlorine can be evaporated via boiling or standing Much higher risk in using untreated water Water Safety Rural areas may need to have their water tested due to well contamination due to agricultural runoff Estimated that 10 million Americans may drink water that doesn’t meet EPA guidelines Cryptosporidium, a parasite, sickened 400,000 people in Milwaukee; not killed by chlorine High risk people are advised to boil their drinking water for one minute prior to use for drinking (HIV-AIDS, chemotherapy patients) Alternatives to Chlorinated Tap Water Boil Store overnight Filters Activated carbon Reverse osmosis Distillation UV sterilization Ozone Bottled Water Expensive Environmental impact – Manufacture – Transport – Landfill Bottled Water Sources 75% springs/wells – Ozone 25% municipal tap water – Carbon filtered Bottled Water Independent testing – – – – 1/3 was contaminated Bacteria Arsenic Organic elements Check label Source Treatment State-interstate FDA regulated Water Safety Let cold water run for a minute or two before drinking or using in cooking; will reduce risk of lead exposure Don’t use hot water for food preparation Water and Minerals Related 3 ways – Hard/soft water – Fluid balance – Acid base balance Fluid Balance Water shifts freely in and out of the cells Controlled by the electrolyte concentration “Where ions go, water is sure to follow” Intracellular water volume depends on intracellular potassium and phosphate concentrations Extracellular water volume depends on extracellular sodium and potassium concentrations Na+, K+, Cl Attract water Dissolve in water Electrical charge = electrolytes Cell Membranes Water permeable Impermeable to minerals Osmosis The passage of a solvent such as water through a semi-permeable membrane from a less concentrated compartment to a more concentrated compartment Osmosis Water moves across membrane – Low concentration to high – Equalizes solute concentration Minerals do not move – Draw water across membrane Acid-Base Balance Blood pH 7.35-7.45 Death – pH 8.0 alkalosis – pH 6.8 acidosis Buffers – Protein – Electrolytes – Gather/release hydrogen ions Minerals: Definition Inorganic (contain no carbon) Separate elements Required in small amounts Functions of Minerals Cofactors Bone and connective tissue Blood Metabolism Growth & reproduction Function/formation nerves & muscles Cell membrane transport Minerals function together: – Bone formation – Electrolytes – Blood Minerals in the Body Mineral Classification Major minerals – Require >100 mg /day (1/50 of a teaspoon) – Calcium, phosphorus Trace minerals – Require < 100 mg/day – Iron, zinc Bioavailability of Minerals Not all ingested minerals can be absorbed Example: only 5% of the calcium in spinach is absorbed because spinach contains oxalic acid About 25% of dietary iron is absorbed (better absorbed from dairy products) Bioavailability of Minerals Presence of binders and dietary fiber Minerals in animal products are better absorbed The more refined a food is, the fewer minerals Only iron is added back to enriched grain products Fiber-Mineral Interactions Phytic acid (phytate) in grain fibers can limit absorption of some minerals by binding to them Oxalic acid: substance in plants (spinach) that binds minerals High fiber diets can decrease the absorption of iron, zinc, magnesium, and other minerals Bioavailability of Minerals Mineral content of plant foods reflects the soil in which is it grown Mineral/mineral competition: too much of one mineral can interfere with the absorption of another – Zinc interferes with copper absorption Presence of vitamins: example, vitamin C enhances absorption of iron Toxicity of Minerals Trace minerals are more toxic Result of supplementation Presence of contaminants in supplements Look for the United States Pharmacopeia (USP)-approved brands Iron Toxicity Men in general and older women should avoid multivitamin-mineral supplements with iron because of the risk of iron toxicity Major Minerals Sodium Table salt (NaCl): 40% sodium, 60% chloride Sodium 95% of ingested sodium is absorbed Major positive ion in extracellular fluid Aldosterone regulates sodium balance Key for retaining body water Excretion regulated by the kidneys Muscle contraction Conduction of nerve impulses Deficiency of Sodium Rare Persistent vomiting/ diarrhea Excessive perspiration (losing 2-3% of body weight) Depletion of sodium in the body Muscle cramp, nausea, vomiting, dizziness, shock, coma Normally kidney will respond by conserving sodium Correcting Deficiency Pedialyte for children Gatorade for adults Salt foods Dietary Sources of Sodium Average American eats 4-6 grams sodium in foods and softened water 20% comes from salt added in cooking or at the table 35-80% comes from processed foods 4-27% comes from water (issue at 500 mg level if water contains more than 40 ppm (40 mg or 2 mEq/liter) Sodium Content of Fresh Foods Plain pasta or rice Fruit (any) <10 mg Vegetables, unsalted Milk 1 cup <75 mg Meat, poultry, fish unsalted <90 mg <10 mg 125 mg Sodium Content of Processed Foods Potato chips 1 oz 180 mg American cheese 1 sl 300 mg Italian dressing 2 T 510 mg Instant noodle soup 1170 mg KFC chicken pot pie 2160 mg Meat lover’s stuffed pizza 2 slices 2850 mg Sodium Needs Body only needs 100-200 mg/day Minimum requirement is 500 mg/day Daily Value is 2400 mg/day Typical intake is 4000-7000 mg/day Sodium Adaptation Today’s salt is tomorrow’s urine People can adjust to the lower salt taste “Salt Sensitive” 10%-15% of adults are (particularly African Americans) High sodium intake leads to fluid retention and high blood pressure Recommend 2-3 gm sodium per day Recommended for all individuals High intake of sodium (>2000 mg) increases calcium loss Check your blood pressure regularly Potassium Positive ion in the intracellular fluid Functions in fluid balance and nerve impulse transmission Associated with lowering blood pressure 90% of potassium consumed is absorbed Food Sources and Need for Potassium Found in fruits, vegetables, milk, grains, meats, dried beans Minimum requirement is 2000 mg/day Daily Value is 3500 mg/day Typical intake is 2000-3000 mg/day Excess potassium is excreted by the kidneys Potassium Pyramid High Potassium Foods Baked potato: 844 mg Milk: 377 mg Raisins: 825 mg Spinach: 419 mg Sweet potato: 397 mg Tomato: 254 mg Tomato Juice: 400 mg Beer: 128 mg Coffee: 96 mg Chocolate: 174 mg Waffle: 146 mg Eggnog: 420 mg Vegetable soup: 337 mg Potassium Deficiency Rare Use of diuretics Alcoholic, anorexia nervosa, bulimia nervosa Loss of appetite, muscle cramps, confusion, constipation, irregular heart beat Chloride Negative ion for the extracellular fluid Components of hydrochloric acid (HCl), immune response, nerve function Excess is excreted by the kidneys/perspiration Chloride Minimum requirement is 700 mg/day Much is obtained from salt consumption (table salt is 60% chloride) High intake may cause high blood pressure Hypertension Systolic blood pressure/diastolic blood pressure Optimal is less than 120 / 80 mm Hg HTN is a sustained systolic pressure of >140mm Hg or >90 mm Hg for diastolic Hypertension 95% of all HTN have no clear cause (primary or essential HTN) Secondary HTN: related to other conditions, like kidney disease Why Control Blood Pressure? Silent disease (may have no symptoms) Causes cardiovascular disease, kidney disease, stroke, retinopathy, declining brain function African Americans most at risk Causes of HTN Aging Atherosclerosis Obesity (increased fat mass and circulation) Elevated insulin (insulin resistant adipose cells) Inactivity Excess alcohol (usually reversible) Sodium and Blood Pressure Unclear if it is sodium or chloride that is responsible Increases blood pressure with intake Consume no more than 2400 mg/day Increased blood pressure to excrete sodium needed for sensitive people? Fluid retention leads to increased blood volume Lifestyle Interventions in Hypertension Weight loss of as little as 10-15 pounds may normalize blood pressure Regular physical activity Avoid excess alcohol Other Minerals and HTN >1000 mg calcium a day lowers blood pressure 2-4 gm of potassium a day lowers blood pressure Magnesium may lower blood pressure DASH diet: low in sodium, high in fruits, vegetables, whole grains, includes lowfat dairy products Medication and HTN Diuretic – Reduce blood volume – Increase urine output Slows heart rate – relaxation of the blood vessels Calcium 99% is in bones and teeth Makes up 40% of all the minerals present in the body Absorption of Calcium Amount in the body is dependent on amount absorbed Requires a slightly acidic environment Presence of dietary glucose and lactose Increased need Upper part of the small intestine is the site of absorption Availability of vitamin D Absorption of Calcium Normally absorb 25% of calcium in food Increase to ~60% during time of need (pregnancy, infancy) Estrogen increases absorption Parathyroid hormone Factors Decreasing Calcium Absorption Rapid intestinal motility High fiber intake Excess phosphorus Fat malabsorption Factors Decreasing Calcium Absorption Vitamin D deficiency Polyphenols (tannins) in tea Menopause Aging Achlorhydria Blood Calcium is Regulated Blood level is maintained at the price of bone calcium Blood level will be maintained despite inadequate calcium intake (by drawing from bones) Setting stage for future bone fractures Functions of Calcium Blood clot Nerve impulse transmission Muscle contraction Cell metabolism –Activates various enzymes Building Higher Bone Mass Adequate diet Healthy body weight Normal menses Weight-bearing physical activity Moderate intakes of protein, phosphorus, sodium, caffeine Non-smoker Lower the use of certain medications Other Roles of Calcium May lower blood pressure May reduce colon cancer May reduce PMS symptoms May lower blood cholesterol May reduce kidney stones Reduce lead absorption Osteoporosis Calcium deficiency “A pediatric disease with geriatric consequences” Leads to ~1.3 million fractures / year Slender, inactive women who smoke are most at risk “Less bones” Osteoporosis Bone Structure Bone Strength Dependent on bone mass and bone mineral density The more there is, the stronger the bone Bone Growth and Mass Rapid and continual throughout adolescence Peak bone mass: highest attainable density – First 3 decades of life Determined by gender, race, familial pattern, other genetic factors Bone Growth and Mass Bone loss begin ~age 30 Women experience increased bone loss after menopause DEXA bone scan No noticeable symptoms Types of Osteoporosis Type I (postmenopausal) –Occurs after menopause Type II (senile) –Occurs with age in men and women Risk Factors for Osteoporosis Age Gender Race Inactivity Low body weight Diet low in calcium Family history Early menopause; absence of menses Low testosterone levels in men Anorexia, bulimia Some medications Cigarette smoking Excessive alcohol consumption Caffeine, sodium High protein diet Diet and Lifestyle Factors Adequate diet (Ca, vitamin D) Healthy body weight Correct hormonal irregularities Normal menses Weight-bearing and resistance physical activity Don’t smoke Limit excessive intake of protein, phosphorus, sodium, caffeine, wheat bran, and alcohol Prevention Regular menstruation Weight-bearing exercise (but does not compensate for lack of menstruation) Smoking lowers estrogen concentration in the blood Alcohol is toxic to bone cells Estrogen replacement therapies Accurate measurement of height Medication Estrogen – Slows bone turnover Fosamax (bisphosphonates) – Slows bone breakdown Evista (selective estrogen receptor modulators) – Slows bone turnover Calcitonin – Inhibits bone breakdown Side effects Diet and Lifestyle Factors Adequate diet (Ca, vitamin D) Healthy body weight Normal menses Weight-bearing physical activity Don’t smoke Limit excessive intake of protein, phosphorus, sodium, caffeine, wheat bran, and alcohol Food Sources of Calcium Dairy products Kale, collard, mustard greens Calcium fortified foods Tofu (if made with calcium carbonate) Canned fish Food Sources of Calcium Dairy foods provide 75% of the calcium in the American diet Calcium Supplement Recommended for people who cannot incorporate Ca+ into their diets Not recommended with high iron meal Calcium carbonate (40% calcium) – For those with ample stomach acid – Found in antacids Calcium citrate (21% calcium) – Enhanced absorption due to acidity content – Recommended for elderly Risk With Calcium Supplements Lead contamination No FDA regulation Oyster shell Bonemeal Look for United States Pharmacopoeia seal of approval Calcium Needs Daily Value is 1000 mg/day Adequate Intake is 1000 -1200 mg/day for adults Adequate Intake is 1300 mg/day for adolescents (9-18 yrs. old) Average intake range from 600-800 mg/day for women and 800-1000 mg/day for men Phosphorus Body absorption is based on body’s need (70%-90%) No disease associated with deficiency May contribute to bone loss in elderly women Vitamin D enhances absorption Component of ATP, cell membrane, and bone Food Sources of Phosphorus Widely available in foods Dairy, bakery products, sodas, and meats Some from food additives Most difficult to limit intake RDA is 700 mg/day for adults Daily Value is 1000 mg Current intake exceeds RDA Deficiency highly unlikely Toxicity of Phosphorus Problem for individuals with inefficient kidney function Phosphate ions bind calcium Chronic imbalance may lead to bone loss (Ca+/phos ratio) Upper Level is 3-4 g/day Magnesium Primarily in green leafy plants Absorption based on body’s needs (40%-60%) Absorption enhanced by vitamin D Kidneys regulate blood concentration of magnesium Alcohol increases loss in the urine Much stored in the bones Functions of Magnesium Aids in many enzyme reactions Potassium and calcium metabolism Proper nerve and cardiac functions Insulin release from the pancreas May dilate arteries May prevent heart rhythm abnormalities Deficiency of Magnesium Develops slowly Irregular heartbeat Decreased blood pressure Weakness, muscle spasms, disorientation, nausea, vomiting, seizures Food Sources of Magnesium Plant products: Whole grains, vegetables, nuts, seeds Hard tap water Dairy, chocolate, meat RDA for women is 320 mg/day RDA for men is 400 mg/day Daily Value is 400 mg Average intake is lower than the RDA Magnesium Pyramid Too Much or Too Little Magnesium Magnesium loss – – – – Heavy perspiration Long-standing diarrhea or vomiting Alcoholism Disorientation, weakness, muscle pain, poor heart function Toxicity – Caused by medication Sulfur Found in amino acids and vitamins Acid-base balance Drug detoxifying pathways Part of a natural diet, primarily from protein Used to preserve foods