OR TECHNIQUE
advertisement

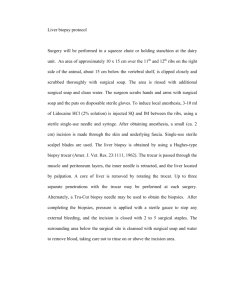
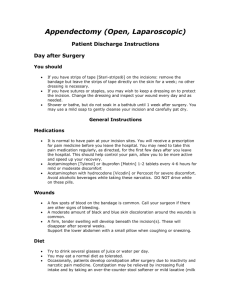
OR TECHNIQUE Composition of OR team • Surgeon. • Assistants the surgeons. • Scrub nurse. • Circulating nurse. • Anesthetists. Division of OR team • The sterile team: includes • Surgeon. • Assistants to surgeons. • Scrub nurse. Un-sterile team: includes: • Anesthesiologist. • Circulate nurse. • Others x-ray tech. Scrub Nurse/Technician Preoperative • Checks the card file for surgeon's special • • • needs/requests. Opens sterile supplies. Scrubs, gowns, and gloves and sets up sterile field. Obtains instruments from flash autoclave if necessary. Checks for proper functioning of instruments/equipment. Performs counts with circulator Pre incision • Completes the final preparation of sterile field. • Assists surgeon with gowning/gloving. • Assists surgeon with draping and passes off suction / cautery lines. During the Procedure • Maintains sterile field. • Anticipates the surgeon's needs (supplies/ equipment). • Maintains internal count of sponges, needles and instruments. • Verifies tissue specimen with surgeon, and passes off to circulator. Closing Phase • • • • • • Counts with circulator at proper intervals. Organizes closing suture and dressings. Begins clean-up of used instruments. Applies sterile dressings Prepares for terminal cleaning of instruments and non disposable supplies. Reports to charge nurse for next assignment. Circulating Nurse Preoperative • • • • • Assists in assembling needed supplies. Opens sterile supplies. Assists scrub in gowning. Performs and records counts. Admits patient to surgical suite. Pre incision • Transports patient to procedure room. • Assists with the positioning of the patient. • Assists anesthesia during induction. • Performs skin prep. • Assists with drapes; connects suction and cautery. During the Procedure • Anticipates needs of surgical team. • Maintains record of supplies added. • Receives specimen and labels it correctly. • Maintains charges and O.R. records. • Continually monitors aseptic technique and patients needs. Closing Phase • • • • • • • • Counts with scrub at proper intervals. Finalizes records and charges. Begins clean-up of procedure room. Applies tape. Assists anesthesia in preparing patient for transfer to post anesthesia care unit [ PACU ]. Takes patient to PACU with anesthesia and reports significant information to PACU nurse. Disposes of specimen and records. Reports to charge nurse for next assignment. Circulate nurse Duties of Circulating Nurse • Application of the nursing process in directing • • and coordinating all nursing activities and supporting the pt. Maintaining the safe and comfortable environment for the pt. and the medical staff. Assisting any members of the O.R. teams if needed. • Must know all supplies, instrument and equipment. • Identification of any environmental dangerous or stressful situation involving the pt. or other team members. • Maintain a good communication link between the O.R. team. • The circulate nurse is the most experienced nursing team members in the O.R. acts as supervisor, advisor and teacher. Classification of surgery • Emergency: without delay life threatening, • • • • immediate attention. Urgent (Imperative): prompt attention (24-30h) acute GB stone, renal stone. Required (planned): patient needs to have surgery (few weeks or months) as Cataracts. Elective: patient should be repair scars, simple hernia. Optimal: cosmetic surgery, individual preference. Scrubbing techniques • Time Method – 5 min. • Counting method Basic positioning for surgery Supine Position and its modifications. Supine position. Trendelenburg position. Reverse Trendelenburg position. Fowler’s and Sitting position. Lithotomy position. Prone position and its modifications. Prone position. Kraske (jackknife) position. Knee-chest position. Lateral position and its modifications. • Lateral position. Kidney position. Sim’s position. Fracture position Preoperative Patient Routines: • Surgical Consent • Nail polish • Sedation. • Diet (NPO 4-8 hr. ) • Make up • Patient Identification • Lab. Tests Technique for transferring the patient to OR table • For mobile pt. 2 of non sterile team • For immobile pt. 4 of non sterile team Hypothermia • Hypothermia------ post- operative shivering----- increase oxygen consumption up to 700%. Intra operative heat loss • Radiation – loss of heat from the patients body • • • to the environment. Convection- loss of heat into the air currents. conduction- loss of heat from the patients body into a cooler surface such as the operating table. Evaporation- loss of heat via perspiration or respiration. Principles of aseptic technique • Only sterile items are used within the sterile field. Sterile persons are gowned and gloved Tables are sterile only at table level Sterile persons touch only sterile items or areas • unsterile persons touch only unsterile items or areas. • Unsterile persons avoid reaching over sterile field • sterile persons avoid leaning over unsterile area. • Edges of anything that encloses sterile contents are considered unsterile • Sterile field is created as close as possible to time of use • Sterile areas are continuously kept in view • Sterile persons keep well within sterile area • Unsterile persons avoid sterile areas Pathogens and infection • Pathogens associated with surgical site infection ( S.S.I.): • Bacteria. • Fungi • Viruse • The most commonly transmitted pathogen in O.R is Staphylococus Aureus (gram + cocci). Mycobacterium Tuberculosis- TB transmitted through airborne droplet nuclei. Infects lungs, kidneys, joints and skin. Sources of Surgical Site Infection ( S.S.I. ): • Normal flora of the patient. 2.Personnel. 3. Inanimate objects (contaminated instruments). 4.Air borne contamination. 5.Contamination during procedure (surg). UNIVERSAL Precautions Applied in an invasive procedure PROTECTION GLOVES MASKS EYEWEAR or FACE SHOELDS GOWNS or APRONS Prevention of puncture injuries • E.g. needles, knifes blades and sharp instruments present a potential hazards for the handler and user. • Do not manipulate by hand • Mouth protection- incase of emergency • Care of specimens- should be contained • Decontamination- all instruments must be cleaned before sterilization or disinfection. • Laundry- soiled linen should be handled as little as possible. • Waste - Blood and suctioned fluids . • Hand washing- following every contact with patient, blood and body fluids. Cleaning, Disinfection and Sterilization Levels of disinfection • High level disinfection – kills all microorganisms and may kill certain spores with sufficient contact time. • Intermediate level disinfection – kills most microorganisms except spores. • Low level disinfection –kills fungi, bacteria, and hydrophilic viruses. Sterilization • Destruction of all microorganisms in or about an object as by steam, chemical agents, ultraviolet radiation. Methods of Sterilization • Thermal. – Steam under pressure\ moist heat. – Hot air\dry heat. – Microwaves\ non ionizing radiation. uv light [ ultraviolet light ]. • Chemical. – – – – – – Ethylene oxide gas. Formaldehyde gas. Hydrogen peroxide plasma\vapor. Ozone gas. Glutaraldehyde activated solution. Per acetic acid solution. •Ionizing radiation (physical). • Disinfectant and disinfectant/ sterilant agents. High level disinfectant and sterility compounds • Glutaraldehyde (cidex)2% concentration with PH of 7.5- 6.5, is a high level disinfectant. 20 minutes for disinfection and 10 hours for sterilization. • Hydrogen peroxide 6%. Solution of 6% H2O2 with detergents and 0.58% phosphoric acid have been proven to be parricidal with 6 hours of exposure at 20 degree. • Peracetic Acid (steris) sterilization. This cycle usually takes 30 minutes. • Chlorine compounds. - Chlorine compounds are effective against HIV, HBV and other viruses. • Formaldehyde. It is bactericidal, psudomonacidal and fungicidal in 5minutes exposure, tuberculocidal and virucidal in 10-15 minutes, sporicidal in 12 hours. Intermediate level disinfectants. • Phenolic compounds- (phenol, carbolic acid). • Iodophors- (iodine, Polidine, Povidine) • Alcohol 50-90% Methods of monitoring the sterilization process • Mechanical: Monitoring of parameters (time, temp, and pressure). • Chemical: Internal and external indicator for steam and E.O. • Biological: Is a device that contains a known number and specific type of microorganisms that are killed when exposed to the sterilizing conditions. Homeostasis and Blood Replacement Methods of controlling bleeding during surgery: • Mechanical methods. 1- clamping or ligation or clipping the cut vessels. 2-Sponges-Patties (cottonoids) 3- Pledgets-Teflon. 4- Bone wax- Bee’s wax. 5- Suction, Drains. 6- Tourniquet, Pressure devices . • Pharmacological Agents. - Absorbable gelatin (gel foam). - Collagen - Oxidized cellulose (surgicel). - Silver Nitrate (nasal bleeding). - Epinephrine (vasoconstriction). - Thrombin (enzyme). • Thermal Hemostasis. - Elctrosurgery and Laser. Blood Loss and Blood Replacement: • Blood replacement can be: - Homologous- patient’s own blood. - Autologus- from the same species. Blood types and groups. - A, B, O, AB. Methods of wound closure include • • • • • Sutures. Staples. Clips. Tapes. Glues Suture - means ligation or approximating tissue together. Methods of suturing • Everting sutures- skin edges. 1. Simple continuous. 2. Simple interrupted. 3. Continuous locking. 4. Horizontal mattress. 5. Vertical mattress. • Inverting sutures- used for two layers - Purse String Suture .Tentions sutures .Traction sutures - umbilical tape and vessel loop .Endoscopic suturing- Kinds of sutures • Absorbable suture -Natural 1. Plain surgical gut 2. Chromic surgical gutsalt solution. Is treated in a chromium 3. Collagen suture • Absorbable suture - Synthetic 1. Polydioxanone suture (PDS) 2. Poligleceprone( monocryl ) 3. Polyglyconate (MAXON) 4. Polyglactin 910 (Vicryl) 5. Polyglycolic acid (Dexon) 6. Copolymer(Panacryl) • Non absorbable Suture - Natural 1. Surgical silk 2. Surgical stainless steel • Non absorbable Suture - Synthetic 1. Ethilon, Dermalon ( monofilament ) 2. Nurolon ( multifilament uncoated ) 3. srugilon ( multifilament coated ) 4. NovafiL 5. Prolene 6. Ethibond Kinds of Surgical staples 1. Skin stapler 2. Intra luminal circular stapler (CEEA) Circular End to End Anastomosis . 3. Ligating and dividing stapler ( GIA ) Gastro Intestinal Anastomosis. Roticulator. 4. Endo scopic stapler. Tissue Adhesives • Biologic adhesives - Fibrin glue. - Autologous or homologous- plasma and clotting factors. - Pooled donor plasma- multiple donors. Synthetic adhesives- Cyanoacrylate glue- dries after 2 ½ minutes. - Methyl methacrylate- used for fixation (bone cement). Kinds of skin graft – Auto graft- skin is grafted from one part of the patient's body to another part. – Allograft -Human tissue is grafted to another person (from cadaver). – Xenograft- Skin obtained from a dissimilar species . – Artificial skin- synthetic skin Terms Associated With Wound Healing • Adhesion - Band of scar tissue that holds or unites surfaces or structures together that are normally separated. Contracture-Formation of extensive scar tissue over a joint Dead space - Space caused by separation of wound edges or by air trapped between layers of tissue. Debridement - Removal of damaged tissue and cellular or other debris from a wound to promote healing and to prevent infection. Dehiscence - Partial or total splitting open or separation of the layers of a wound. • Edema - Abnormal accumulation of fluid in interstitial spaces of tissues • Evisceration -Protrusion of viscera through an abdominal incision. • Extravasations- Passage of blood, serum, or lymph into tissues. • Exudate - Fluid, cells, or other substances that have been discharged from vessels or tissues. • Granulation tissue - Formation of fibrous collagen to fill the gap between the edges of a wound healing by contraction “second intention “. • Hematoma - Collection of extravasated blood in tissue. • Granuloma- Inflammatory lesion that forms around a foreign substance, such as glove powder or a suture Knot. • Homeostasis- Arrest of blood flow or hemorrhage, the mechanism is by coagulation (formation of a blood clot). • Incision- Intentional cut through intact tissue (synonym: surgical incision). • Ischemia- Decrease of blood supply to tissues. • Necrosis- Death of tissue cells. • Scar- Deposition of fibrous connective tissue to bridge separated wound edges & to restore continuity of tissues • Seroma- Collection of extravasated serum from interstitial tissue or a resolving hematoma in tissue. • Tensile strength- Ability of tissues to resist rupture. • Tissue reaction- Immune response of the body to tissue injury or foreign substances. • Wound disruption- Separation of wound edges. Kinds of Drains • Passive drains- T- Tube, Foley catheter, enlarged bulbous ends (mushroom, malecot, pezzer catheters), pen rose. Active drains – Hemovac drain, sump drain, chest drain. Complications of wound healing • Hematoma/ Seroma • Scar/ Surgical • Adhesions • Postoperative wound disruption Classification of Occupational hazards • Physical- back injury, fall, noise, pollution, • • irradiation, electricity and fire. Chemical- including anesthetic gases, toxic fumes from gases and liquids, cytotoxic drugs, and cleaning agents. Biologic- including the patient( as a host for or source of pathogenic microorganisms), infectious waste. Cuts, or needle stick injuries, surgical plume and latex sensitivity. Ionizing Radiation • Radiation has cumulative effects • Sterile team members and others who can not leave room should stand 2 meters or more. • Staff members may request relief from exposure during pregnancy. • Lateral X-Ray more dangerous than Anterior Posterior ( AP ) X-Ray SURGICAL SPECIALITIES • Endescopy: Examination of a body part or cavity with an optical system in a tubular structure. • Insufflation: Act of filling with gas. Laparoscopy is performed with carbon dioxide. • Laparoscopy: Endoscope examination of the peritoneal body Hazards of endoscopy: • Perforation- Major organ or vessel. • Bleeding- from biopsy site, • Hypothermia- CO2 is colder than body temp. • Infection- by microorganism Breast procedures • Incision and drainage- surgical opening of an inflamed area because of infections in lactating breast. Breast biopsy • Fine needle aspiration- 22-25 gauge needle attached to a syringe is inserted into the tumor mass. • Core biopsy- Incisional biopsy- The mass is incised and a portion is removed for histologic examination. Excisional biopsy - The entire mass is removed for pathologic study. Sentinel node biopsy-In OR the tumor is injected with a dye containing iso-sulfan blue that is taken up by the lymph nodes of the breast. Fiber optic ductoscopyA flexiable 0.9mm scope with a 0.2 mm working channel is used in the ductal lumens of the breast. Lumpectomy • Partial mastectomy, consists of removal of the entire tumor mass along with at least 1 to 2 cm of surrounding non diseased tissue. • Done for tumor that measure less than 5 cm. Segmental mastectomy • a wedge of breast tissue is removed. • Simple mastectomy ( total mastectomy )The entire breast is removed without lymph node dissection. Modified radical mastectomy- Removal of the entire breast along with all axillary lymph nodes. Radical mastectomy- Removal of entire breast along with the axillary lymph nodes, the pectoral muscles and all adjacent tissues. Extended radical mastectomy- The entire breast is removed with the underlying pectoral muscles, axillary contents, and upper internal mammary lymph node chain. Characteristics of the incision • Ease and speed of entry into the abdominal cavity. • Maximum exposure. • Least post operative discomfort. • Maximum post operative wound strength. Types of abdominal incisions • Paramedian incision • Longitudinal midline incision • Subcostal upper quadrant oblique incision ( Kocher ) • Chevorn incision –bilateral subcostal incision • McBurney incision • Thoracoabdominal incision • Mid abdominal Transverse incision • Pfannestiel incision • Inguinal incision Biliary Tract • Biliary Tract Procedures • Cholecysectomy – is the removal of gallbladder Choledochoscopy -Intra operative biliary endoscopy provides image, transmission and illumination. CholelithotripsyNon invasive procedure in which high energy shock waves are used to fragment cholesterol gall stones. Choledochostomy- A T-Tube is used to drain the common bile duct through the abdominal wall. Choledochotomy – bile duct. Is an incision of the common CholecystoduodenostomyCholecystojejnostomy – - Both performed to relieve an obstruction in the distal end of the common duct. Anastomosis between the gall bladder and duodenum or jejunum. CholedochoduodenostomyCholedochojejunostomyAre side to side anastomosis between duodenum or jejunum and the common duct. Splenic Procedures • Splenectomy • Splenorrhaphy Pancreatic Procedures • Pancreaticojejunostomy • Pancreaticodudenectomy Esophageal Procedures • Esophageal hiatal heniorrhaphy Nissen fundoplication -360 degree Toupet fundoplication – 180-200 Gastrointestinal Surgery • Gastroscopy • Gatrostomy • Total Gastrectomy • Vagatomy • Pylroplasty • Gastrojejunostomy • Gastroplasty • Gastric Bypass Intestinal Procedures • colectomy • Ileostomy • Cecostomy • Colostomy • Appendectomy Colorectal Procedures • Sigmoidscopy • Colonoscopy • Polypectomy Complications of abdominal surgery • • • • • • Pulmonary complications. Fluid and electrolyte imbalance Peritonitis and wound infection Wound infection can cause wound disruption Incisional hernia Adhesions are the most common cause of post operative intestinal obstruction. Anorectal procedures • Hemorrhoidectomy • Anal abscess • Fistulotomy and fistulectomy • Fissuerectomy • Pilonidal cyst and sinuses Kinds of hernia • Inguinal hernia • Femoral hernia • Umbilical hernia • Ventral ( incisional ) hernia • Hiatal hernia Amputation of extremities • Reasons for amputation: • Massive trauma. • Malignant tumor. • Extensive infection. • Vascular insufficiency. • Phantom limb pain- Is the sensation that the amputated part is still present. Gynecologic and Obstetric Surgery • Colposcopy- Done for identification of abnormal epithelium to target for biopsy of the lower part of cervical canal and vaginal wall. • Culdocentesis- Blood, fluids and pus in the culdesac is aspirated by needle via the posterior vaginal fornix for suspected of intra peritoneal bleeding, ectopic pregnancy, trauma, and tumor. • Colpotomy- Transverse incision is made through the posterior vaginal fornix to facilitate diagnosis by intra peritoneal palpation, inspection of the pelvic organs or determination of fluids. Fallopian tube diagnostic procedures • Hystosalpingography • Hysteroscopy and Laparscopy Vaginal procedures • • • • • • • • Vaginal lesion Vaginectomy Vaginoplasty Vesicovaginal fistula Rectovaginal fistula Vaginal hysterectomy Dilation and Evacuation (D & E) Dilation and Curettage ( D & C ) Abdominal Procedures • • • • • • • • Total Abdominal hysterectomy Salpingo-Oophorectomy Myomectomy Ovarian cystectomy Shirodkar and Cerclage procedures Ectopic Pregnancy Cesarean Section (CS) In Vitro Fertilization (IVF) Urologic Surgery • Surgical Procedures • Nephrectomy • Pyeloplasty- Revesion of the renal pelvis • Percutaneous Nephrolithotomy, Nephrolithotripsy PCNL • Ultrasonic lithotripsy • Electrohydrolic lithotripsy • Nephrolithotomy or pyelolithotomy • Extracorporeal shock wave lithotripsy • • • • • • • (ESWL) Ureteroscopy Percutaneous Uretrolithotomy Ureterolithotomy- An open procedure for the removal of stones from the ureter. Cystolithotomy and cystolitholapaxyRemoval of bladder stone, crushing a urinary stone in the bladder. Cystoscopy Cystotomy or Cystoplasty Cystectomy • Urethrotomy-cut into a urethral stricture • Urethroplasty • Orchiectomy • Testicular Torsion • Hydrocelectomy • Varcocelectomy • Vasectomy • Transurethral Resection of Prostate (TURP) • Suprapubic Prostatectomy Sings of TUR syndrome • • • • • • • • Mental confusion. Nausea and vomiting. Hypertension followed by hypotension. Symptoms of fluid over load and pulmonary edema. Bradycardia and dysrhthmia. Visual disturbances. Seizures and twitching. Coma. Treatment of TUR syndrome • Administration of IV hyper tonic saline • Monitoring of serum sodium levels • Diuretics Orthopedic Surgery • Steps of bone healing – Hematoma formation. – Callus formation, 1-2 weeks. – Calcification process, completed by 6 weeks. - Remodeling phase, 6 months to 1 year. Indications for orthopedic surgery • Fracture of bones. • Reconstruction of joints. • Repair of tendons and ligaments Kinds of fractures – Traumatic fracture- may be closed or open fracture. – Pathologic fracture- due to demineralization of bone (osteoporosis or the aging process). Methods of treating fractures • Closed reduction with immbolization • Skeletal traction • External fixation • Internal fixation • Electrostimulation Arthrodesis • Fusion of a joint may be achieved by removing the articular surface and securing bony implant that inhibits motion. Arthroplasty • • • • It is done to : Restore or improve range of motion Provide stability Relieve pain. • Arthroscopy • Arthrotomy • Bunionectomy: Hallux valgus It is done to remove a painful exotosis or to functionally or cosmetically correct the deformity. • Neurolysis: • Meniscectomy Neurosurgery • Craniotomy • Cranioplasty • Epidural hematoma Bleeding caused by • rupture or tear of the middle meningeal artery or its branches forms a hematoma between the skull and the dura Subdural hematoma Bleeding between the dura matar and arachnoid is caused by laceration of viens that cross the subdural space. • Laminectomy • Diskectomy - discectomy • Spinal fixation Ophthalmic Surgery • Ophthalmic drugs • Mydriatic drugs used to dilate the pupil. • Miotic drugs used to constrict the pupil. Ocular surgical procedures • Extra ocular procedures• • • • are conditions affecting the exterior surface of the eye. Chalazion: an extremely common but benign tumor of the lid, it can be malignant. Correction of pitosis: is a drooping of the upper lid Ectropin: is a condition in which either the upper or the lower lid is everted ( turned out). Entropin: is a condition in which either the upper or the lower lid is enverted (turned in). Lacrimal apparatus • Lacrimal duct dilation –Probing • Dacryocystectomy: removal of the lacrimal sac due to chronic inflammation. • Dacryocystorhinostomy (DCR): construction of a new opening into the nasal cavity from the lacrimal sac Extra ocular muscle • squint – Procedure on the oculomotor muscles which control eye movement, are done to correct misalignment that interferes with the ability of the two eyes to remain in simultaneous focus on a viewed object. ORBIT • Enculation: is the complete removal of the eyeball, severing of its muscular attachments. The muscle stumps are preserved. Over lying fascia and conjunctiva are closed to hold the prosthesis in the socket. • Evisceration: is the removal of the contents of the eyeball only, the outer sclera and muscles are left intact. • Exenteration: is the removal of entire eye and orbital contents including tendon, fatty and fibrous tissue. It is done incase of malignant tumor of the lid or eyeball. Intra Ocular procedures • Pterygium: it is benign growth of the conjunctival tissue over the corneal surface. • Corneal transplantation (Keratoplasty) • Cataract: Is an opacification of the crystalline lens, its capsule or both • Extra capsular cataract Extraction (ECCE) • Implantation of intraocular lens (IOL) • Vitrectomy It is the removal of a portion of the vitrous humor (vitrous body) that fills the space between the lens and the retina Vascular Surgery – The vein has valve and carry deoxygenated blood. – The artery has no valve and carry oxygenated blood. – Thrombectomy and embolectomy: A fogarty catheter is inserted proximally and advanced into a vessel distally beyond the obstruction.The balloon on the tip is then inflated. As the catheter is withdrawn, thrombotic or embolic material is removed to restore blood flow to an extremity. Vascular surgical procedures • Femoropopliteal bypass • Aneurysmectomy -Kinds of aneurysm: 1.Fusiform aneurysm 2.Saccular aneurysm • The most common affected vessels in an aneurysm: 1. 2. 3. 4. Abdominal aorta. Thoracic aorta. Aortic arch. Popliteal arteries. Venous stasis disease • When the valves of the veins fail to function normally, increased backpressure of blood causes the veins to become dilated----- Varicose Vein. • Rx-Ligation and stripping of varicose veins • Fasciotomy: is the treatment of choice for the prevention of compartment syndromes after acute ischemia in the upper or lower extremity. • Vascular shunts: • Arterio venous shunts and fistulas: 1. Anastomosis at the wrist between the radial artery and cephalic vein. 2. Loop fistula may be created with a graft from the brachial artery to the cephalic or basilica vein. Plastic and Reconstructive Surgery • Aesthetic procedures: Blepharoplasty- correct deformities of the upper or lower eyelids of one or both eyes Otoplasty- repair of deformity of one or both external ears of an adult Rhinoplasty- reshaping of the nose. • Mentoplasty- the shape and size of the chin can be altered for aesthetic and functional bite disorders. • Rhytidoplasty- face lift. • Liposuction- localized areas of fat deposits are removed by suction assisted lipectomy. • Abdominoplasty- includes excising excess lax abdominal wall skin and adipose tissue and tightening abdominal wall musculature. ENT, HEAD, and NECK SURGERY The ear consists of three parts: 1. External ear: consists of auricle (pinna), 2. external auditory canal, tympanic membrane (eardrum). Middle ear: consists of Tympanic cavity , a closed chamber that lies between the tympanic membrane and the inner ear inside the cavity there is a three small bones, the ossicular chain ( malleus, incus, stapes) they resemble the hammer, anvil, and stirrups. 3. Inner ear: The two main sections are the cochlear and vestibular • Potential complications of ear infection: 1. Facial paralysis. 2. Meningitis. 3. Intracranial infection (brain abscess). Surgical procedures of the ear • External ear procedure: 1. Removal of a foreign body from the outer canal usually in children 2. drainage of hematoma due to injury 3. Excision of tumor- pinnectomy • Middle ear procedures 1. Mastoidectomy- the eradication of mastoid air cells done to relieve complications of acute or chronic complications. 2. Tympanoplasty: it refers to any procedure performed to repair defects in the eardrum or middle air structures for the purpose of reconstructing sound conduction paths. 3. Stapedectomy: Partial or total removal of the stapes. • Inner ear procedure -Implantation of cochlear prosthesis: A cochlear implant can restore perception of sound to patients who have performed sesorineural deafness not responsive to external amplification of hearing aids. Nose • • • • Turbinectomy- removal of turbinate. PolypectomySeptoplastyRhinoplasty- correction of deformity of the nose. • FESS- functional endoscopic sinus surgery